Therapeutic Equivalence: What It Means and Why It Matters for Your Medications
When you hear therapeutic equivalence, the condition where two medications produce the same clinical effect and safety profile in patients. Also known as bioequivalence, it means a generic drug isn’t just cheaper—it’s meant to do the exact same job as the brand-name version. This isn’t marketing jargon. It’s a strict standard set by health regulators to make sure you get the same results whether you pick the $5 generic or the $50 brand.
But here’s the thing: not all generic drugs are created equal. generic drugs, medications that contain the same active ingredient as a brand-name drug but are sold under a different name after the patent expires must pass rigorous tests to prove they release the same amount of medicine into your bloodstream at the same speed. If they don’t, they’re not approved. That’s why brand-name drugs, originally developed and marketed by pharmaceutical companies under a patent aren’t always better—just more expensive. The difference often comes down to fillers, coatings, or packaging, not how the drug works in your body.
Therapeutic equivalence matters most when you’re switching from one drug to another. Maybe your insurance pushed you to a cheaper option. Maybe your pharmacy ran out of the brand. If the drugs aren’t truly equivalent, you could see side effects, reduced effectiveness, or even dangerous drops in blood levels—especially with drugs like seizure meds, blood thinners, or thyroid pills. That’s why doctors and pharmacists check the FDA’s Orange Book before swapping medications. It’s the official list that tells them which generics are approved as interchangeable.
And it’s not just about cost. drug substitution, the practice of replacing a prescribed medication with a therapeutically equivalent alternative is a tool to make care more affordable without sacrificing safety. But it only works if everyone—patients, pharmacists, prescribers—understands what therapeutic equivalence really means. Too many people assume all generics are risky. Too many assume brand names are superior. Neither is true. The science says otherwise.
Look at the posts below. You’ll find real cases where therapeutic equivalence plays out in daily life: someone switching from brand-name Zoloft to generic sertraline and wondering if it’ll still work. Or a patient on metformin who noticed a change after a pharmacy swap. Or how doctors decide between Torsemide and furosemide based on how their bodies handle the drug. These aren’t theoretical debates. They’re decisions that affect sleep, energy, heart health, and whether you can afford to keep taking your meds.
Therapeutic equivalence isn’t about cutting corners. It’s about making smart, science-backed choices. And if you’re taking any medication long-term, you deserve to know exactly what’s in your pill—and why it works the way it does.

Therapeutic Equivalence: What It Really Means for Patient Safety
Therapeutic equivalence ensures generic drugs work just like brand-name ones. Learn how the FDA guarantees safety, saves billions, and protects patients through strict bioequivalence standards.
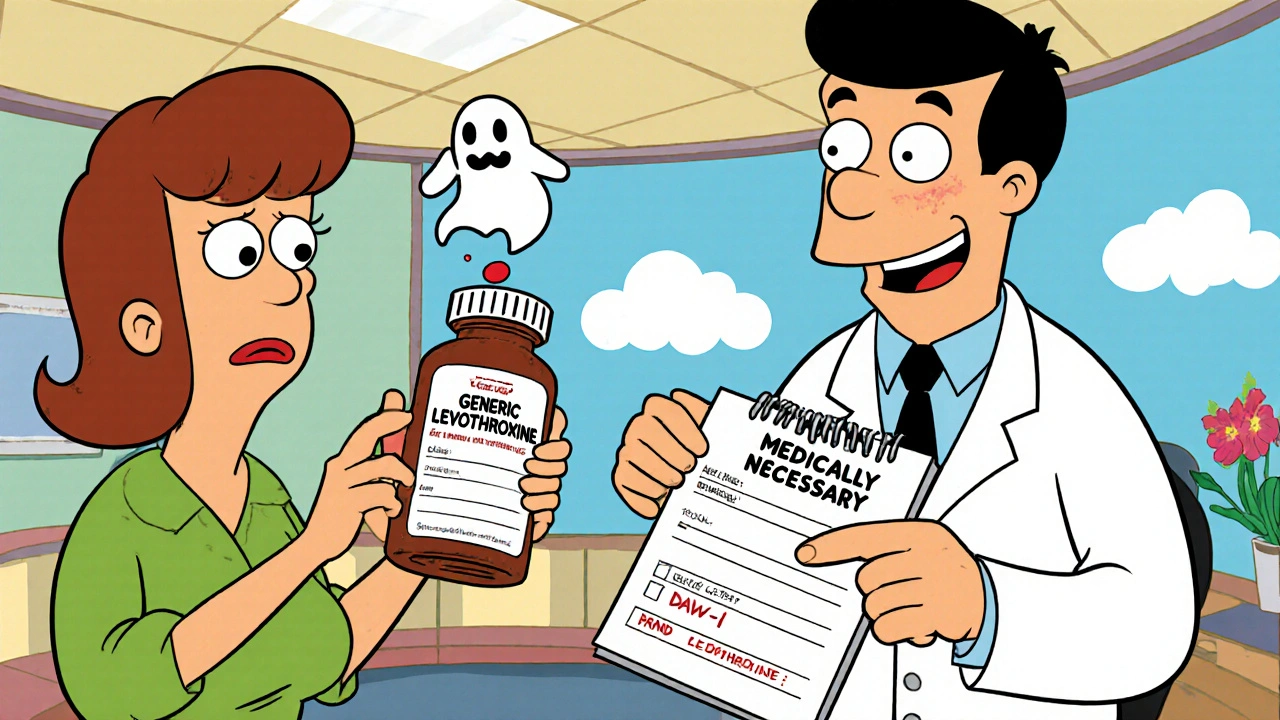
How to Switch Back from a Generic to a Brand Medication Safely
Switching back from a generic to a brand-name medication can be necessary for safety, but it requires medical documentation, insurance approval, and careful monitoring. Learn the steps to do it right.





