Insurance Drug Coverage: What’s Covered, What’s Not, and How to Fight Denials
When you rely on insurance drug coverage, the portion of your health plan that pays for prescribed medications. Also known as prescription insurance, it’s not a guarantee—you’re often stuck navigating hidden rules, step therapy, and surprise denials. Many people assume if a doctor prescribes it, insurance will pay. That’s not true. Even common drugs like metformin or amitriptyline can be blocked if they’re not on your plan’s formulary, or if your insurer demands you try cheaper alternatives first.
Prior authorization, a requirement where your doctor must get approval before the insurer pays for a drug is one of the biggest roadblocks. It’s not just for expensive biologics—sometimes even generic painkillers or antivirals need it. And if your doctor’s office doesn’t push back, your prescription sits on hold. Drug prior authorization, a bureaucratic hurdle that delays treatment often leads to people skipping doses, switching meds, or paying out of pocket. Meanwhile, medication affordability, how much you actually pay after insurance kicks in can vary wildly between plans—even for the same drug. One plan might cover Tadalista at $10 a month; another charges $200. No one tells you this until you’re at the pharmacy counter.
Insurance denials happen for reasons you can’t always control: a drug isn’t on the formulary, it’s deemed "not medically necessary," or you didn’t try a cheaper version first. But you’re not powerless. Many people get denied medications approved by simply appealing with their doctor’s notes, citing clinical guidelines, or switching to a different plan during open enrollment. The posts below show you how to spot dangerous interactions between your meds and OTC drugs, how to handle side effects that make adherence hard, and why switching from generic to brand isn’t always a luxury—it’s sometimes a medical necessity. You’ll find real stories about people fighting for coverage on drugs like metronidazole, pirfenidone, and hydroquinone combinations—medications that insurers often try to restrict. Whether you’re managing diabetes, MS, or chronic skin conditions, knowing how to navigate these systems isn’t optional. It’s how you stay healthy without going broke.
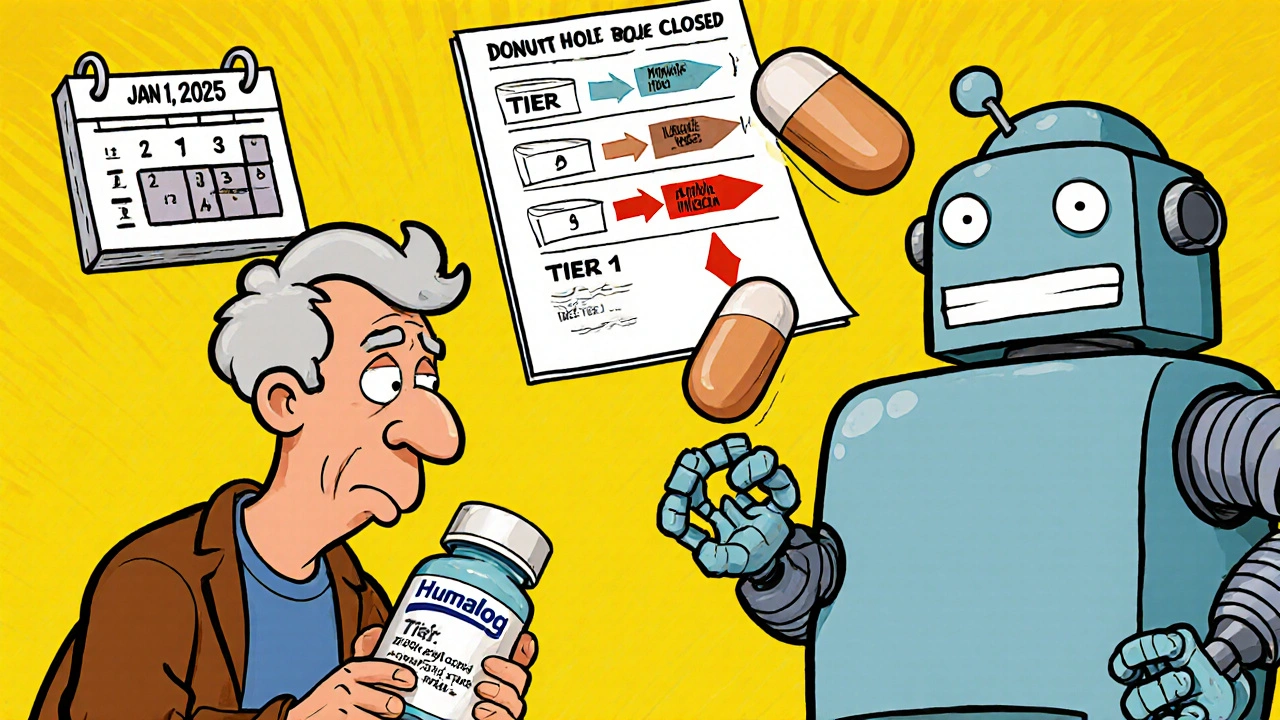
Insurance Changes and Generic Switching: How Formulary Updates Affect Your Prescription Costs in 2025
Understand how 2025 Medicare formulary updates are pushing patients toward generics and biosimilars, what it means for your prescription costs, and how to protect yourself from unexpected drug switches and price hikes.