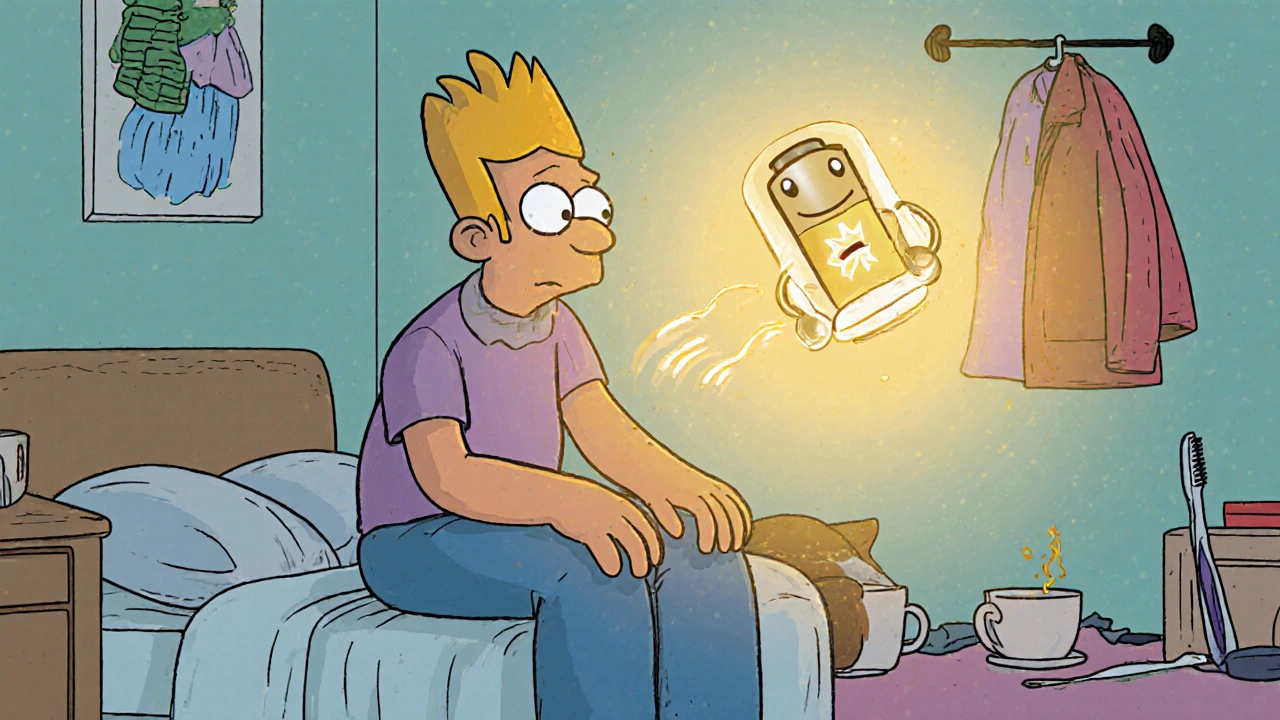
Multiple sclerosis doesn’t just cause weakness or numbness-it drains your energy like a battery that won’t hold a charge. For many people living with MS, fatigue isn’t just tiredness. It’s the kind of exhaustion that makes getting out of bed feel like climbing a mountain, and even simple tasks like brushing your teeth or making coffee become overwhelming. That’s where amantadine comes in. It’s not a cure, but for thousands of people, it’s one of the few tools that actually helps them get through the day.
What Amantadine Actually Does for MS
Amantadine was originally developed in the 1960s as an antiviral drug to fight influenza A. But doctors noticed something strange: patients taking it for the flu also reported feeling more alert and less fatigued. That led to trials in people with multiple sclerosis, and by the 1980s, it became one of the first medications officially used to treat MS-related fatigue.
It doesn’t work by reducing inflammation or slowing nerve damage like other MS drugs. Instead, amantadine affects brain chemicals-mainly dopamine and glutamate-that play a role in energy, focus, and movement. Think of it like a gentle boost to your brain’s internal battery. It doesn’t add power, but it helps your brain use what’s already there more efficiently.
Studies show that about 40% to 60% of people with MS who take amantadine report noticeable improvements in fatigue. One 2021 review of clinical trials found that patients taking amantadine scored, on average, 25% higher on fatigue scales compared to those on placebo. That might not sound like much, but for someone who can’t get out of bed without help, that’s life-changing.
Who Benefits Most from Amantadine
Not everyone with MS responds to amantadine, and it’s not a one-size-fits-all solution. People who tend to see the best results are those with relapsing-remitting MS who struggle with daytime fatigue that doesn’t improve with rest. It’s less effective for people whose fatigue is tied to heat sensitivity, depression, or poor sleep quality.
Amantadine is also sometimes used to help with leg stiffness or slow movement-symptoms that overlap with Parkinson’s. That’s because it boosts dopamine, which is involved in both motor control and energy regulation. If you’ve noticed your legs feel heavy or your steps are slower than they used to be, amantadine might help with that too.
It’s not a first-line treatment, though. Most neurologists try lifestyle changes first: better sleep, cooling vests, exercise, and pacing your day. If those don’t cut it, and fatigue is still holding you back, amantadine becomes a realistic next step.
Dosing and How It Works in Practice
Amantadine is taken as a pill, usually once or twice a day. Most people start with 100 mg daily-often in the morning-to avoid trouble sleeping. After a week or two, if there are no side effects, the dose might be increased to 200 mg per day, split into two doses (100 mg in the morning, 100 mg at lunch).
It takes time to kick in. You won’t feel better the first day. Most people notice changes after 1 to 2 weeks. Some take up to 6 weeks to feel the full effect. That’s why it’s important to stick with it, even if you don’t see results right away.
Many people take it with food to reduce stomach upset. It’s also important to avoid taking it late in the day. Even though it’s not a stimulant like caffeine, it can interfere with sleep in some people. If you’re having trouble falling asleep, talk to your doctor about switching to a single morning dose.

Side Effects and Risks
Amantadine is generally well-tolerated, but it’s not without risks. The most common side effects include:
- Lightheadedness or dizziness
- Swelling in the ankles or feet
- Insomnia or trouble sleeping
- Nausea
- Blue discoloration of the skin (livedo reticularis), especially on the legs
Less common but more serious side effects include confusion, hallucinations, or heart rhythm changes. These are rare but more likely in older adults or people with kidney problems. That’s why your doctor will check your kidney function before and during treatment. Amantadine is cleared by the kidneys, so if they’re not working well, the drug can build up to unsafe levels.
It’s also not safe to stop suddenly. If you’ve been taking it for months and decide to quit, you should taper down slowly under medical supervision. Stopping abruptly can cause withdrawal symptoms like high fever, muscle stiffness, or even delirium-similar to what happens when someone stops Parkinson’s medication too fast.
How It Compares to Other Fatigue Treatments
There are other options for MS fatigue, but each has trade-offs.
| Treatment | Effectiveness | Common Side Effects | Cost (Monthly, AUD) |
|---|---|---|---|
| Amantadine | 40-60% respond well | Dizziness, swelling, insomnia | $20-$40 |
| Modafinil | 50-70% respond | Headache, anxiety, nausea | $120-$200 |
| Prescription stimulants (e.g., methylphenidate) | 30-50% respond | High blood pressure, insomnia, dependence risk | $80-$150 |
| Non-drug (exercise, pacing, cooling) | Varies widely | Minimal | $0-$50 (equipment) |
Modafinil is often seen as stronger, but it’s much more expensive and not always covered by insurance. Stimulants can help, but they carry risks of dependence and aren’t recommended for long-term use. Amantadine sits in the middle: moderate effectiveness, low cost, and fewer risks than stimulants.
Many people combine amantadine with non-drug strategies. Walking 20 minutes a day, using a cooling vest in hot weather, or scheduling rest breaks every two hours can multiply its benefits. One patient in Brisbane told me she takes amantadine in the morning, wears a cooling neck wrap at work, and takes a 30-minute nap after lunch. She says that’s the only way she can keep her job.
When Amantadine Might Not Be Right for You
There are situations where amantadine is a bad idea:
- You have kidney disease or reduced kidney function
- You’re taking other drugs that affect dopamine (like levodopa or certain antidepressants)
- You have a history of seizures or psychiatric conditions like psychosis
- You’re pregnant or breastfeeding-there’s not enough data to say it’s safe
- Your fatigue is mostly caused by depression or sleep apnea, not MS
If you’re unsure whether your fatigue is from MS or something else, your doctor should run tests. Blood work to check thyroid levels, vitamin D, iron, and sleep studies can rule out other causes. Treating those might eliminate the need for amantadine altogether.
Real Stories, Real Results
Emma, 42, was diagnosed with MS five years ago. She used to be a teacher, but by year three, she could barely make it through a school day. She tried rest, better sleep, even yoga-but nothing stuck. Her neurologist suggested amantadine. After six weeks, she noticed she could grade papers without needing a nap afterward. She started walking her dog again. She didn’t get back to 100%, but she got back to living.
James, 58, started amantadine after his MS relapse left him with heavy legs and constant exhaustion. He was on a wheelchair part-time. After two months on amantadine, he could stand for 10 minutes longer during physio. He still uses a cane, but he says, “I feel like I’m not just waiting to collapse anymore.”
These aren’t miracle stories. But they’re real. And they happen more often than most people think.
What to Do Next
If you’re struggling with MS fatigue and nothing’s helping, talk to your neurologist about amantadine. Bring a symptom diary-note when you’re most tired, what makes it worse, and what (if anything) gives you even a little boost. That helps your doctor decide if it’s worth trying.
Don’t expect it to fix everything. But if fatigue is stealing your days, amantadine might give you back a few hours. And sometimes, that’s enough.
Can amantadine cure multiple sclerosis?
No, amantadine does not cure multiple sclerosis. It only helps manage one symptom-fatigue-and sometimes muscle stiffness. It doesn’t stop the disease from progressing or reduce relapses. Other medications, like disease-modifying therapies (DMTs), are used for that purpose.
How long does it take for amantadine to work for MS fatigue?
Most people start noticing improvements after 1 to 2 weeks, but it can take up to 6 weeks to feel the full benefit. Patience is key. Stopping too early means you might miss out on results.
Is amantadine safe for long-term use?
Yes, many people take amantadine for years with no major issues. But regular kidney function tests are needed because the drug is cleared by the kidneys. If kidney health declines, the dose may need to be lowered or stopped.
Can I take amantadine with other MS medications?
Usually, yes. Amantadine is often taken alongside disease-modifying therapies like interferons or oral pills such as fingolimod. But it can interact with certain antidepressants, anticholinergics, and dopamine-blocking drugs. Always tell your doctor about every medication you’re taking.
Does amantadine cause weight gain?
Weight gain isn’t a common side effect of amantadine. In fact, some people lose a small amount of weight due to reduced appetite or increased activity once fatigue improves. If you notice significant weight changes, check with your doctor-it could be due to other factors like fluid retention or diet changes.
What happens if I miss a dose of amantadine?
If you miss a morning dose, take it as soon as you remember. If it’s late in the day, skip it and wait until the next day. Don’t double up. Missing doses occasionally won’t hurt, but going off it for several days might make your fatigue worse temporarily.
Are there natural alternatives to amantadine for MS fatigue?
There’s no natural supplement proven to match amantadine’s effectiveness for MS fatigue. Some people find relief with regular exercise, cooling techniques, or good sleep hygiene. Others try ginseng or CoQ10, but studies show little to no benefit. Don’t replace amantadine with unproven supplements without talking to your doctor.
Can amantadine help with MS brain fog?
Some people report improved focus and mental clarity while taking amantadine, likely because it boosts dopamine in brain areas involved in attention. But it’s not specifically approved for brain fog, and results vary. If cognitive issues are your main concern, other strategies like cognitive rehab or medications like donepezil might be more targeted.
If you’re considering amantadine, start with a conversation-not a prescription. Track your symptoms, ask questions, and give it time. The goal isn’t to feel perfect. It’s to feel like you can keep going.






Oliver Myers
October 31, 2025 AT 07:24Just wanted to say thank you for writing this so clearly-I’ve been struggling with MS fatigue for years, and this is the first time I’ve seen someone explain amantadine without making it sound like magic or a scam.
I started it six weeks ago, and honestly? I can now make coffee without sitting down halfway through.
It’s not a cure, but it’s the closest thing I’ve found to getting my days back.
Alex Sherman
October 31, 2025 AT 09:33Oh please. Another one of these ‘miracle drug’ posts. Amantadine? Really? You’re telling me a 60-year-old flu drug, originally meant for birds, is somehow the answer to MS fatigue?
Let me guess-you also think vitamin C cures cancer and that yoga fixes spinal lesions.
The real issue here is that Big Pharma doesn’t want you to know that lifestyle changes-real ones, not ‘cooling vests’-are the only thing that works.
But hey, if you want to feel like you’re doing something while your disease progresses, go ahead. I’ll be over here actually managing my condition.
John Concepcion
November 2, 2025 AT 02:38LMAO at people acting like amantadine is some kind of fountain of youth.
You take a pill, suddenly you’re walking your dog? Bro.
I’ve been on it for a year. I still need a nap after showering. The only thing it’s good for is making your ankles look like inflated balloons.
And don’t even get me started on the blue legs. I swear, I looked like a bruised grapefruit walking into my neurologist’s office.
But hey, at least we can all feel good about taking something that costs less than a Starbucks latte, right?
Eileen Choudhury
November 3, 2025 AT 12:56Reading this made me cry a little-not because I’m sad, but because for the first time, someone described my fatigue exactly.
I’m from India, and here, people think MS is just ‘being lazy’ or ‘not eating enough curry.’
My cousin told me to ‘pray harder’ when I said I couldn’t carry groceries. I didn’t correct her. But now, I’m sending her this article.
Amantadine didn’t turn me into Iron Man, but it let me hold my niece’s hand without collapsing after five minutes.
That’s worth more than any pill price tag.
Emmalee Amthor
November 4, 2025 AT 18:44People keep acting like amantadine is this magical fix but… it’s not, right? It’s just… a buffer? Like a tiny spark in a dying battery?
I think the real win here isn’t the drug-it’s that we’re finally talking about fatigue like it’s a real thing, not just ‘you’re tired because you’re not trying hard enough’
Also-blue legs? I didn’t know that was a thing. Now I’m weirdly fascinated. Is it like a mood ring for your veins?
Justin Vaughan
November 5, 2025 AT 22:40Amantadine isn’t the hero-it’s the sidekick.
The real MVPs are the people who track their energy, schedule naps like meetings, wear cooling gear like armor, and refuse to let MS define their limits.
I’ve been on it for three years. It helps. But it’s the 6 a.m. walks, the 3 p.m. ice packs, and the ‘no, I can’t come to dinner’ boundaries that actually keep me alive.
Medication opens the door. Discipline walks through it.
Manuel Gonzalez
November 6, 2025 AT 19:18I appreciate the breakdown. Honestly, most of these posts are either too clinical or too hype-y.
This one? Just… real.
I started amantadine last month. Still waiting for results, but I’m trying to be patient. The fact that it takes 6 weeks to kick in means I can’t just quit if I don’t feel better tomorrow.
Also, thank you for mentioning kidney checks. My uncle had a bad reaction to something similar because no one tested his levels.
Small details matter.
Alexa Apeli
November 6, 2025 AT 20:21Thank you for sharing this comprehensive and deeply thoughtful overview. 🙏
As someone who has supported a loved one through MS for over a decade, I am profoundly moved by the honesty and precision of this piece.
It is not often that medical information is presented with such clarity, compassion, and scientific rigor.
May your words reach those who need them most.
Matthew Kwiecinski
November 8, 2025 AT 17:2340-60% response rate? That’s not a treatment, that’s a coin flip.
And modafinil works better? Then why is amantadine even on the table?
Because it’s cheap. Not because it’s effective.
Let’s stop pretending this is medicine. It’s triage.
They give you the cheapest option and call it a ‘next step.’
Meanwhile, the real treatments? Too expensive. Too risky. Too inconvenient.
It’s not about fatigue. It’s about who gets to feel human.
Dade Hughston
November 9, 2025 AT 18:46I took amantadine for 11 months and it turned me into a zombie with a blue tint and a caffeine addiction
I couldnt sleep so i drank 6 espressos a day just to stay awake for work
Then i got the swelling and the brain fog got worse
So i quit cold turkey
And woke up with a fever so high i thought i was dying
Turns out my body had forgotten how to function without the drug
Now im on modafinil and i still cant walk to the fridge without needing a nap
So yeah
Its not a cure
Its just another way to lose your mind slowly
Caitlin Stewart
November 11, 2025 AT 00:00I’ve been on amantadine for 18 months.
It didn’t fix me.
But it gave me back enough space to try other things.
Exercise. Sleep hygiene. Cooling vests. Therapy.
It wasn’t the answer.
But it was the door.
And sometimes, that’s all you need.
Thank you for writing this.
It’s the kind of post I wish I’d found five years ago.
Jim Peddle
November 12, 2025 AT 14:36Amantadine? Funny you mention that.
Did you know it was originally developed by Nazi scientists during WWII as part of a mind-control program?
They were testing stimulants on concentration camp prisoners to see how long they could stay awake.
Then the U.S. picked it up after the war-Operation Paperclip, remember?
Now it’s being pushed on MS patients like it’s a gift.
It’s not.
It’s a distraction.
While you’re taking your little pill, the real cause of MS-environmental toxins, EMF radiation, glyphosate-is still poisoning your nervous system.
They don’t want you to know that.
Andy Ruff
November 14, 2025 AT 11:46You people are so naive.
You think this drug is helping you? It’s just masking the problem while your body slowly falls apart.
Every time you take it, you’re telling your brain it’s okay to keep burning out.
You’re not healing.
You’re just delaying the inevitable.
And now you’re proud of it?
You’re not fighting MS.
You’re just learning how to live with it while pretending it’s not killing you.
Amantadine isn’t hope.
It’s resignation with a prescription.
Zachary Sargent
November 15, 2025 AT 08:55My neurologist gave me amantadine and said ‘it might help.’
Two weeks later, I was crying in the grocery store because I couldn’t lift a carton of milk.
Then I found out I had a vitamin D deficiency.
Supplement for 3 weeks.
Now I walk 2 miles a day.
Amantadine didn’t help.
My body just needed sunlight.
Don’t let them sell you a pill when the answer is outside.
Leslie Schnack
November 16, 2025 AT 20:14Just a quick question: if amantadine works by boosting dopamine, why isn’t it used more for brain fog or depression in MS?
I’ve read that some people report clearer thinking, but it’s never discussed as a primary benefit.
Is that just anecdotal? Or is there data I’m missing?
Because if it helps with focus, maybe it’s underused for cognitive symptoms.