Brand Name Drugs: What They Are, Why They Cost More, and When They Really Matter
When you hear brand name drugs, patented medications sold under a company’s trademark, often at higher prices than their generic versions. Also known as originator drugs, they’re the ones you see advertised on TV or recommended by your doctor after a new diagnosis. These are the drugs that first hit the market after years of research and clinical trials—think Lipitor, Nexium, or Humira. They come with a price tag that often shocks people, especially when they find out a generic version exists that’s 80% cheaper. But here’s the thing: the active ingredient is usually identical. So why do brand name drugs still exist? And when does paying extra actually make sense?
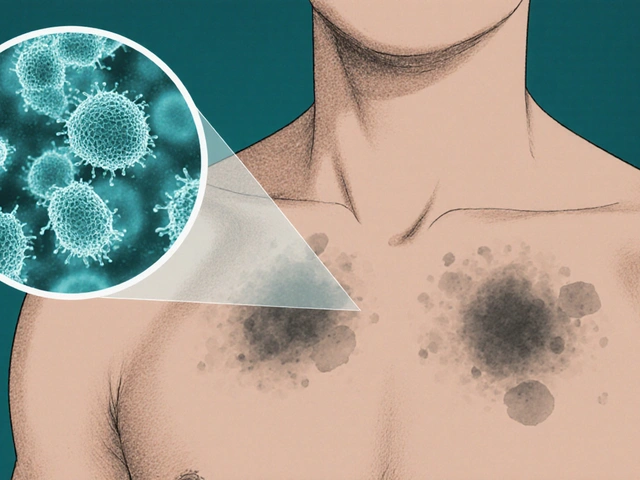
The difference between generic drugs, medications that copy the active ingredient of a brand name drug after its patent expires and brand name ones isn’t in how they work—it’s in the packaging, the marketing, and the cost structure. Generics have to prove they’re bioequivalent, meaning they deliver the same amount of medicine into your bloodstream at the same rate. The FDA requires this. But brand name companies spend millions on ads, patient support programs, and doctor incentives. That’s why your co-pay for the brand version might be $50, while the generic is $5. Still, there are cases where switching isn’t simple. For drugs with narrow therapeutic windows—like warfarin or thyroid meds—even tiny differences in how the body absorbs the drug can matter. Some patients report feeling different on generics, even when tests show no difference. That doesn’t mean the generic is weaker; it might mean your body is sensitive to fillers or coatings that changed.
Then there’s the issue of drug pricing, how pharmaceutical companies set costs based on patents, demand, and market control. In the U.S., companies can charge whatever they want for brand name drugs because there’s no government price negotiation for most prescriptions. A drug that costs $100 in Canada might be $1,000 here. That’s why people are turning to mail-order pharmacies, patient assistance programs, or even buying from trusted international sources. But not all savings are safe. Some online sellers offer fake or expired versions. Always check if the pharmacy is licensed and verify the drug’s lot number with the FDA if you’re unsure.
So when should you stick with the brand name? If you’ve been on it for years and your condition is stable, and switching triggers side effects—even mild ones—it’s worth asking your doctor for a prior authorization. Insurance companies often require you to try the generic first, but they’ll approve the brand if there’s documented medical need. Also, some drugs don’t have generics yet because the patent hasn’t expired. Others, like complex biologics, have biosimilars instead—these are similar but not exact copies, and they’re still expensive.
What you’ll find in the articles below are real stories and facts about how people navigate these choices. From people who had to fight their insurer to keep their brand name medication, to others who saved hundreds a month by switching safely. You’ll learn how to read labels, spot hidden costs, and understand when a brand name drug isn’t just a name—it’s the only option that works for you.

Generic Drug Savings: Real Numbers and Healthcare Statistics
Generic drugs save Americans over $445 billion a year-yet most people don’t know how much they’re paying unnecessarily. See the real numbers behind generic vs brand-name drug costs and how to save big.