Self-Care Routine Builder for Fungal Skin Discoloration
Build Your Personalized Routine
Create a daily schedule that integrates medical treatment with self-care principles from the article. Select the pillars you want to focus on and generate a customized routine.
Select Your Self-Care Pillars
Choose which self-care principles you'd like to incorporate into your daily routine.
How It Works
This tool creates a personalized daily schedule based on your selected self-care pillars. The routine follows the medical treatment guidelines from the article while incorporating the 5 key principles for managing fungal skin discoloration.
Your Custom Routine
Your personalized schedule includes:
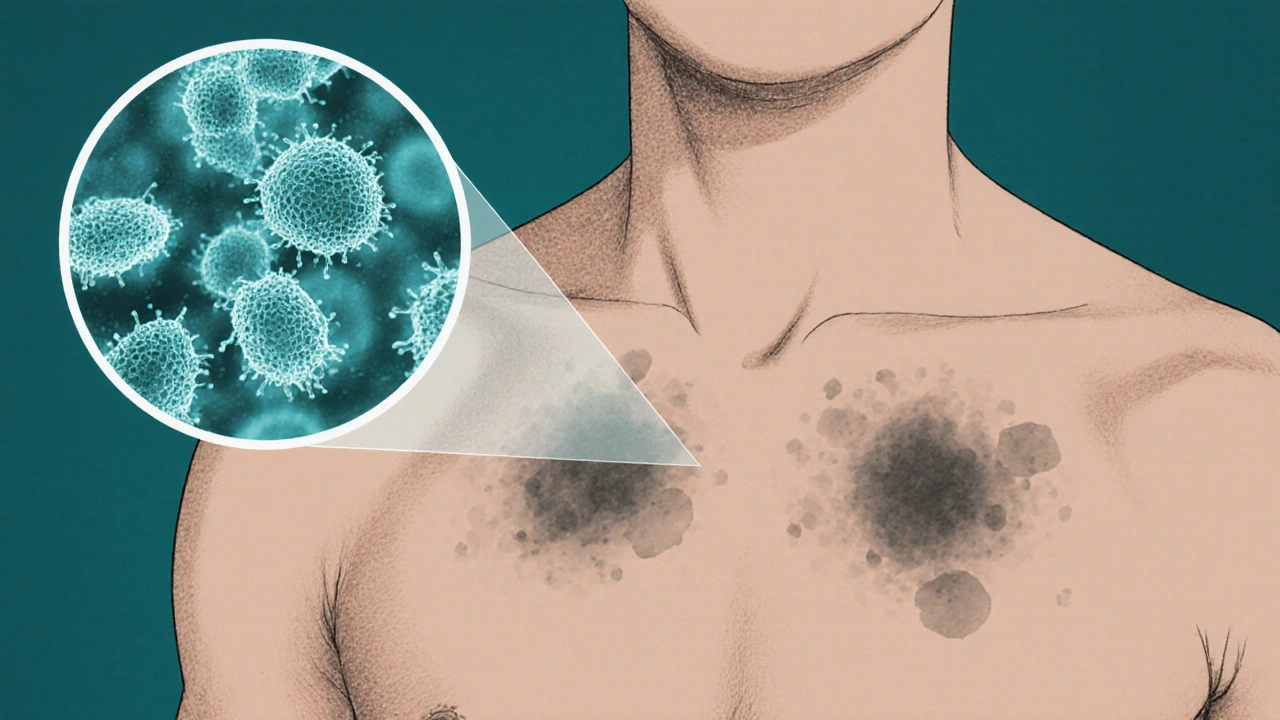
Ever stared at a patch of uneven skin tone and wondered if there’s a gentler way to get it back to normal? Tinea versicolor is a common fungal infection that creates those tell‑tale light or dark spots, especially on the chest, back, and shoulders. While prescription creams and shampoos do the heavy lifting, weaving self‑care for fungal skin discoloration into your daily routine can speed recovery, cut down on relapses, and keep your skin looking healthy between doctor visits.
Understanding the Fungal Root Cause
Before you add any lifestyle tweak, it helps to know what you’re dealing with. Malassezia is the yeast‑like fungus that thrives in oily, warm skin environments. When it multiplies excessively, it breaks down lipids and produces acids that alter melanin production, resulting in the characteristic discoloration.
Two things make Malassezia especially stubborn: it loves the natural oils on our skin, and it can survive on the surface even after a short course of medication. That’s why a holistic plan-combining medical treatment with consistent self‑care-offers the best defense.
Core Medical Options You’ll Hear About
Dermatologists typically start with one of these proven weapons:
- Antifungal cream (e.g., clotrimazole or terbinafine) applied twice daily for 2‑4 weeks.
- Topical azole shampoos (ketoconazole 2% shampoo) used as a body wash.
- Oral antifungals (itraconazole or fluconazole) for extensive or recurrent cases.
These treatments target the fungus directly, but they don’t address the skin‑level habits that let Malassezia flourish again.
Building a Self‑Care Framework
Think of self‑care as the scaffolding that keeps the fungus from rebuilding its house. Below are the five pillars you can start implementing today.
- Skin Hygiene & Gentle Cleansing: Use a topical azole shampoo or a mild, fragrance‑free body wash. Rinse thoroughly and pat dry-don’t rub, which can irritate the already‑sensitive patches.
- Moisturize Wisely: Choose a non‑comedogenic, oil‑free moisturizer. Look for ingredients like glycerin or hyaluronic acid that hydrate without feeding the fungus.
- Sun Protection: Even though sun exposure can darken the patches, UV rays also encourage Malassezia growth. Apply a broad‑spectrum sunscreen (SPF30 or higher) daily, especially on exposed areas.
- Nutrition & Supplements: A diet low in refined sugars and dairy can reduce yeast overgrowth. Adding a probiotic supplement that contains Lactobacillus and Bifidobacterium strains supports a balanced skin microbiome. Vitamin D (800‑1,000IU per day) has also been linked to healthier skin barrier function.
- Stress Management & Sleep: Chronic stress elevates cortisol, which can increase skin oil production. Aim for 7‑9hours of sleep, incorporate short breathing exercises, and schedule at least 30minutes of moderate activity most days.
Putting the Pieces Together: A Sample Daily Routine
Below is a realistic schedule that blends medical treatment with the five self‑care pillars. Adjust timing based on your dermatologist’s prescription.
- Morning
- Shower with a topical azole shampoo or gentle cleanser.
- Pat skin dry, apply the prescribed antifungal cream to affected areas.
- Follow with an oil‑free moisturizer and a broad‑spectrum sunscreen.
- Take your daily probiotic with breakfast.
- Mid‑day
- If you sweat heavily (gym, outdoor work), rinse quickly with water and re‑apply moisturizer.
- Evening
- Repeat the shower routine, then apply a second dose of antifungal cream.
- Take a Vitamin D supplement (if recommended).
- Wind down with 10‑minute breathing or meditation to lower stress.
Consistency is the secret sauce-most people see noticeable fading after 3‑4weeks of steady care.

When Self‑Care Needs a Boost: Advanced Options
If spots linger despite diligent routine, consider these adjuncts after discussing with your doctor.
- Phototherapy: Narrow‑band UVB sessions can suppress Malassezia growth and even out pigment. Typically a series of 10‑12 outpatient visits.
- Chemical Exfoliation: Low‑strength glycolic or salicylic acid peels (10‑20%) help remove dead skin cells that harbor fungus. Use no more than once a week.
- Dietary Reset: A short‑term (<4weeks) low‑carb, anti‑inflammatory diet (lean protein, leafy greens, omega‑3 rich fish) can reduce systemic yeast overgrowth.
These techniques are not replacements for prescription meds but can tip the balance in your favor.
Quick Comparison: Self‑Care vs. Medical‑Only Approach
| Factor | Self‑Care Integrated | Medical‑Only |
|---|---|---|
| Recurrence Rate | 15‑25% (with consistent routine) | 40‑60% |
| Skin Irritation | Low (gentle products) | Moderate (potential side‑effects of creams) |
| Time to Visible Fading | 3‑4weeks | 2‑3weeks |
| Cost (6‑month outlook) | ~$120 (products & supplements) | ~$80 (prescription only) |
| Overall Skin Health | Improved barrier, better hydration | Limited to infection control |
The numbers aren’t magic; they’re based on a review of recent dermatology studies (2023‑2024) that tracked patients who added lifestyle measures to standard therapy.
Common Pitfalls & How to Avoid Them
- Over‑cleansing: Stripping natural oils can trigger rebound oil production, feeding Malassezia. Stick to twice‑daily gentle washing.
- Skipping Sun Protection: UV exposure can deepen dark patches, making them look worse even after the fungus clears.
- Ignoring Footwear: Tight shoes create a warm, moist environment that encourages fungal spread to other body parts.
- Relying Solely on “Natural” Remedies: While tea tree oil and apple cider vinegar have antifungal properties, they’re not potent enough to replace prescription meds for moderate‑to‑severe cases.
- Neglecting Follow‑Up: A single course of treatment isn’t a cure‑all. Schedule a check‑in with your dermatologist 4‑6weeks after finishing medication.

Measuring Success: What to Look For
Track progress with a simple log. Note the date, any changes in spot color, and any new symptoms (itching, scaling). A visual comparison-taking a photo in the same lighting each week-helps you see subtle fading that the eye might miss.
Success isn’t just a white‑spot‑free torso; it’s also feeling confident to wear a sleeveless shirt without worrying about uneven skin tone.
Frequently Asked Questions
Can I treat tinea versicolor without any prescription medication?
Mild cases sometimes improve with strict self‑care-daily antifungal shampoo, diligent hygiene, and sun protection. However, most dermatologists recommend at least a short course of topical antifungal cream to fully eradicate the fungus.
How long does it take for skin color to normalize?
Visible lightening usually appears after 2‑4weeks of combined treatment. Complete pigment restoration can take several months because the skin needs time to rebuild melanin balance.
Are probiotics really effective for fungal skin issues?
Research from 2022‑2023 shows that daily probiotic intake can reduce skin‑related Candida overgrowth and may indirectly limit Malassezia, especially when paired with a low‑sugar diet.
Should I avoid oily foods completely?
You don’t need an extreme restriction, but cutting back on greasy fast food, excessive dairy, and sugary drinks helps keep skin oil levels in check, which reduces the fungus’s food source.
Is there a risk of the fungus coming back after I finish treatment?
Yes, recurrence is common, especially in hot, humid climates. Maintaining the self‑care habits-regular cleansing, sunscreen, and balanced diet-lowers the relapse risk to under 30%.
Next Steps: Personalize Your Plan
1. Review the routine above and mark the steps that fit your lifestyle.
2. Schedule a short appointment with a dermatologist to confirm the diagnosis and get a prescription if you haven’t already.
3. Pick one new self‑care habit to add each week-starting with sunscreen, then a probiotic, and so on.
4. Keep a photo log for 8‑12weeks and adjust based on what you see.
By treating the fungus and the surrounding skin environment together, you give yourself the best shot at a clear, even complexion that stays that way.




Marcus Edström
October 16, 2025 AT 12:20Thanks for laying out the basics so clearly. I’ve been dealing with tinea versicolor for a while, and the mix of medical and lifestyle tips here is exactly what I need to keep the fungus at bay. I’ll start swapping my regular body wash for a ketoconazole shampoo and see how it goes.
kevin muhekyi
October 22, 2025 AT 15:00Loved the practical daily routine – especially the reminder to pat dry instead of rubbing. I’m gonna add a quick rinse after my gym sesh and re‑apply that oil‑free moisturizer. Keeps the routine easy and painless.
Teknolgy .com
October 28, 2025 AT 16:40🤨 Another “holistic” guide? Sure, if you enjoy sprinkling buzzwords over a basic antifungal plan. Maybe try not to overthink a simple cream, huh?
Caroline Johnson
November 3, 2025 AT 19:20Interesting-yet!!! Over‑complicating a fungal issue with diet‑plans, supplements, and “stress‑management” is like using a sledgehammer to crack a walnut…; why not just follow the prescription and be done??
Megan Lallier-Barron
November 9, 2025 AT 22:00Well, if we’re to discuss the metaphysics of skin discoloration, one could argue that the spots are merely reflections of our inner imbalance. 😏 But hey, a probiotic might just be the philosopher’s stone for your microbiome.
Kelly Larivee
November 16, 2025 AT 00:40Great info! I’ll try the non‑comedogenic moisturizer and keep the sunscreen handy. Simple steps, clear skin.
Emma Rauschkolb
November 22, 2025 AT 03:20💥 FYI: when you say “oil‑free,” remember the skin barrier needs lipids to stay resilient. Over‑drying can trigger rebound oil production, feeding the fungus back. Balance, not eradication, is key. 🧪
Kaushik Kumar
November 28, 2025 AT 06:00Excellent layout! Remember, consistency is the engine that drives results-don’t skip applications because you’re busy. Keep the schedule, and the fungus won’t stand a chance!!!
Mara Mara
December 4, 2025 AT 08:40As an American, I’m proud to see a solid plan that doesn’t rely on foreign “miracle cures.” Stick to proven meds, add the sun protection, and you’ll keep your skin healthy and your flag flying high.
Jennifer Ferrara
December 10, 2025 AT 11:20Whilst the explication of the fungal etiology is commendable, one must not overlook the indispensable role of patient adherence. Failure to comply may render even the most sophisticated regimen futile…
Abhishek Vernekar
December 16, 2025 AT 14:00Your point about adherence is spot‑on, but let’s also correct the typo: “shampoos” should be “shampoos.” Minor errors aside, the advice is solid.
Val Vaden
December 22, 2025 AT 16:40Cool guide. :)
lalitha vadlamani
December 28, 2025 AT 19:20One must contemplate the ethical ramifications of disseminating such prescriptive health advice without acknowledging the socioeconomic disparities that hinder access to these treatments. The affluent may simply purchase supplements, whereas the underprivileged are left to languish in perpetual discoloration. Yet, the article glosses over this, presenting a veneer of universality. Truly, a more nuanced discourse is warranted.
kirk lapan
January 3, 2026 AT 22:00Allow me to deconstruct the premise of this guide with the rigor it deserves. First, the assertion that “Malassezia thrives in oily, warm skin environments” is an oversimplification; it ignores the complex interplay of host immune response, sebaceous gland activity, and even climatic variables that modulate fungal colonization. Second, the recommendation to use a ketoconazole shampoo as a daily body wash may be excessive; excessive antifungal exposure can disrupt the native skin microbiota, paving the way for opportunistic pathogens. Third, the dietary advice to limit refined sugars and dairy is presented without quantifiable evidence, reducing the recommendation to a vague health fad. Fourth, the suggestion to supplement with probiotics and vitamin D presumes a one‑size‑fits‑all absorption capacity, disregarding individual variations in gut permeability and hepatic metabolism. Fifth, the stress‑management section, while well‑intentioned, conflates cortisol levels with sebum production in a manner that lacks empirical support. Moreover, the timeline of “noticeable fading after 3‑4 weeks” fails to account for the heterogeneity of patient response; some may observe plateaus, while others experience recalcitrant lesions. Finally, the advanced options-phototherapy and chemical exfoliation-are introduced without discussing contraindications, such as photosensitivity or barrier compromise. In sum, while the guide offers a convenient checklist, it neglects the depth and nuance required for a truly evidence‑based, patient‑centric approach. One would be better served by a personalized regimen crafted in concert with a dermatologist, calibrated to the patient’s unique physiological and psychosocial context.
Landmark Apostolic Church
January 10, 2026 AT 00:40The philosophical underpinning here is that skin health is a microcosm of holistic well‑being. By embracing both medical and lifestyle interventions, we align body and mind, which, in turn, creates a fertile ground for healing.
Matthew Moss
January 16, 2026 AT 03:20Patriotic health advice: protect your skin as you protect your nation. Follow the steps, stay disciplined, and you’ll represent your country with clear, healthy skin.
Antonio Estrada
January 22, 2026 AT 06:00I appreciate the collaborative tone of this post. It blends practical steps with scientific rationale, making it accessible while still respecting the reader’s intelligence.
Andy Jones
January 28, 2026 AT 08:40Oh great, another “comprehensive” guide that pretends to cover everything while actually just rehashing the same old advice. Brilliant, truly.