Every year, Americans fill over 3.9 billion prescriptions for generic drugs. That’s nearly 9 out of every 10 prescriptions written. But here’s the kicker: those same generics account for just 12% of total prescription drug spending. Meanwhile, brand-name drugs, which make up only 10% of prescriptions, eat up 88% of the money spent on meds. This isn’t a glitch. It’s the math of savings.
How Much Do Generics Actually Save You?
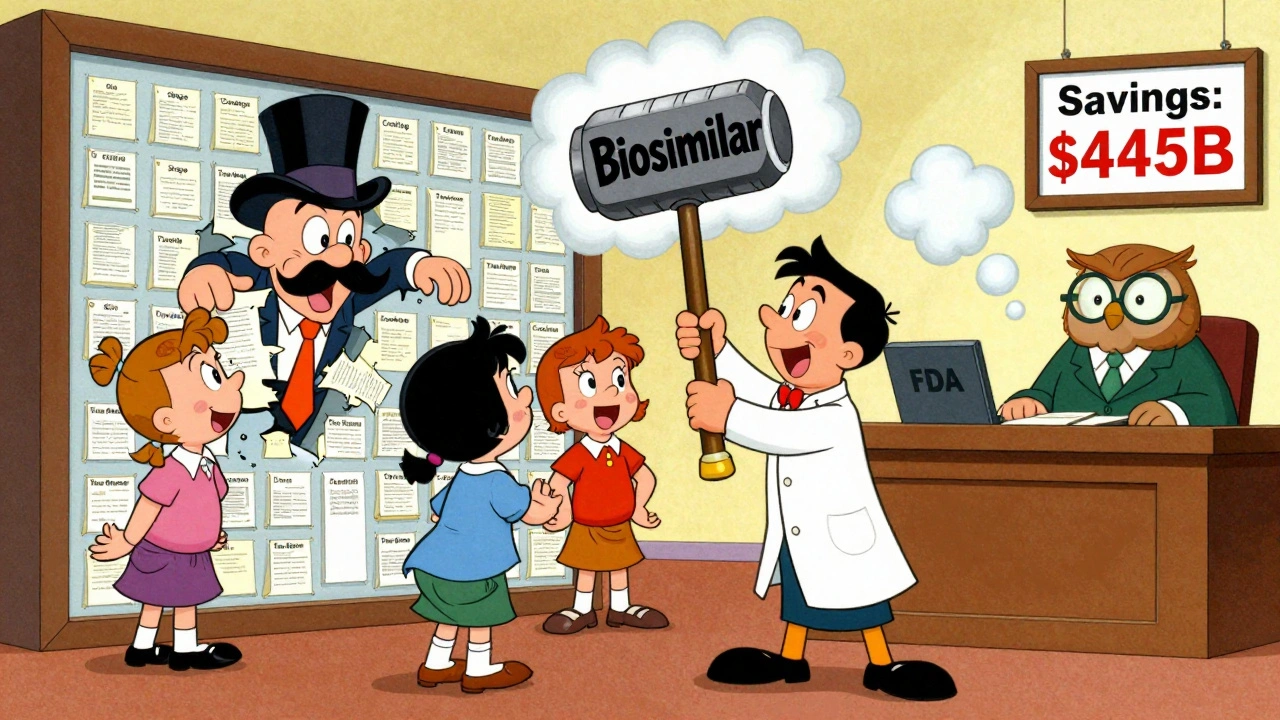
In 2024, the average out-of-pocket cost for a generic prescription was $6.95. For a brand-name drug? $28.69. That’s more than four times as much. For someone filling three prescriptions a month, switching to generics saves about $650 a year. Multiply that by millions of patients, and you get the real picture: Americans saved $445 billion on prescription drugs in 2023 alone because of generics and biosimilars.
These aren’t theoretical numbers. They’re what’s happening in pharmacies right now. A diabetic on metformin pays $4 for a 30-day supply. The brand version? Over $100. A patient with high blood pressure on lisinopril spends under $10 a month. The brand? More than $150. That’s not just convenience-it’s life or death for people choosing between meds and groceries.
Why Are Generics So Much Cheaper?
Generic drugs aren’t cheaper because they’re lower quality. They’re cheaper because they don’t have to repeat the billion-dollar clinical trials that brand-name drugs do. Thanks to the Hatch-Waxman Act of 1984, generic manufacturers only need to prove their drug is bioequivalent-meaning it works the same way in the body. No need to re-prove safety or effectiveness. That cuts development costs by 90%.
That’s why a drug like atorvastatin (the generic for Lipitor) costs pennies. The original brand took years and $1.2 billion to develop. The generic? A few million and a few months. The savings get passed on. And with over 16,000 generic drugs available in the U.S., there’s almost always a cheaper option.
The Billion-Dollar Patent Game
But here’s where things get messy. Big pharma doesn’t want generics to win. So they play a long game. They file dozens-sometimes over 75-patents on a single drug. These aren’t new inventions. They’re minor changes: a new coating, a slightly different pill shape, a new time-release method. These are called “patent thickets.”
One heart failure drug, Entresto, had its monopoly extended from 2016 to 2034 using this tactic. That’s 18 extra years of high prices. And when generics finally do enter, companies sometimes pay them to stay off the market. These “pay-for-delay” deals cost consumers $3 billion a year, according to Blue Cross Blue Shield’s 2025 report.
It’s not just about patents. Some companies do “product hopping”-pulling a popular drug off the market and replacing it with a slightly modified version that gets a new patent. Patients are forced to switch, often to a more expensive version. The Congressional Budget Office estimates ending these practices could save $1.1 billion over 10 years.

Biosimilars: The Next Big Wave
Biosimilars are the generic version of complex biologic drugs-things like insulin, rheumatoid arthritis treatments, and cancer drugs. They’re harder to copy than pills, but they’re coming fast. Since their introduction, biosimilars have saved the U.S. healthcare system $56.2 billion. In 2024 alone, they saved $20.2 billion.
Take Stelara, a drug for psoriasis and Crohn’s disease. When nine biosimilars hit the market in 2025, prices dropped by up to 90%. Suddenly, thousands of patients who couldn’t afford treatment could get it. That’s not just savings. That’s access.
But here’s the catch: biosimilars still make up less than 30% of the market in most cases. Why? Because doctors aren’t always told they’re safe. Pharmacists can’t always substitute them automatically. And insurance plans don’t always cover them the same way. That’s changing, but slowly.
Who’s Winning? Who’s Losing?
The winners? Patients. Medicare. Medicaid. Employers. Pharmacy benefit managers (PBMs). In 2025, 87% of commercial health plans required generic substitution when available. Kaiser Permanente cut pharmacy costs by 30% in 18 months just by pushing generics.
The losers? Patients without insurance. People on fixed incomes. Those stuck with brand-name drugs because their doctor didn’t know a generic was available-or because their state still doesn’t allow pharmacists to switch without permission. Only 42 states have modern pharmacy laws that let pharmacists substitute generics without re-approving the prescription.
And then there’s the big pharma companies. Their profits are shrinking as more drugs go generic. But they’re fighting back with lobbying, legal battles, and pricing tricks. In January 2025, big pharma raised prices on 250 drugs by an average of 4.5%-nearly double the inflation rate. Meanwhile, generic prices kept falling.
What’s Changing in 2025?
This year, three blockbuster drugs are losing patent protection: Entresto ($5.4 billion in sales), Tradjenta ($1.7 billion), and Opsumit ($1.5 billion). Together, that’s over $8.6 billion in brand-name revenue up for grabs. When generics enter, prices could drop by 80-90%. That’s hundreds of millions in savings in just these three drugs.
The FDA approved 745 generic drugs in 2024-up 12% from 2023. That’s the fastest pace in over a decade. The Inflation Reduction Act is trying to cap brand drug prices, but it doesn’t help until generics are already on the market. That’s backwards. The real solution? Let competition work.
Meanwhile, bipartisan bills like the Affordable Prescriptions for Patients Act and the Drug Competition Enhancement Act are moving through Congress. They aim to shut down patent thickets and product hopping. If they pass, we could see another $3 billion in annual savings by 2027.
Is There Any Risk in Switching?
Some people worry generics don’t work as well. That’s a myth. The FDA requires generics to be identical in active ingredient, strength, and how the body absorbs them. Over 99% of generic drugs perform exactly like the brand.
There are rare exceptions-like narrow therapeutic index drugs (warfarin, levothyroxine, some epilepsy meds)-where tiny differences matter. Even then, the FDA says switching between generic brands is safe for most people. Less than 1% of adverse events reported to the FDA are linked to generic drugs.
If you’ve had a bad experience, it’s likely not the drug. It could be the filler, the coating, or even your body adjusting. Talk to your pharmacist. They can help you find the right version.
What You Can Do Right Now
- Always ask if a generic is available. Don’t assume your doctor already did.
- Use tools like GoodRx or SingleCare to compare prices. Sometimes the cash price for a generic is cheaper than your insurance co-pay.
- Ask your pharmacist if they can substitute a generic-even if your script says “dispense as written.” In most states, they can override that.
- Check the FDA’s Orange Book to see if a generic is approved and what manufacturer makes it.
- For biologics, ask if a biosimilar is an option. Many are just as effective and way cheaper.
There’s no reason to pay more than you have to. Generics aren’t a compromise. They’re the smart choice.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent-meaning they work the same way in your body. Generic manufacturers are held to the same quality standards as brand-name companies. Over 99% of generics perform identically to their brand counterparts.
Why do some people say generics don’t work as well?
In rare cases, patients report differences when switching between generic versions of the same drug-especially for narrow therapeutic index medications like warfarin or levothyroxine. This isn’t because generics are inferior, but because even tiny changes in inactive ingredients can affect absorption in sensitive individuals. The FDA tracks these reports and has found fewer than 1% of adverse events are linked to generics. If you notice a change after switching, talk to your doctor or pharmacist. They can help you stick with the same manufacturer or adjust your dose.
Can I save money by switching to a generic even if my insurance covers the brand?
Absolutely. Many insurance plans have high co-pays for brand-name drugs-even if they cover them. Sometimes the cash price of a generic is lower than your co-pay. Use a price comparison tool like GoodRx or SingleCare to check. You can often pay cash for a generic at a pharmacy for under $10, even if your insurance would charge you $30 or more for the brand.
What are biosimilars, and how are they different from generics?
Biosimilars are generic versions of biologic drugs-complex medicines made from living cells, like insulin, rheumatoid arthritis treatments, and cancer drugs. Unlike small-molecule generics, biosimilars aren’t exact copies because biologics are too complex to replicate perfectly. But they’re highly similar in structure and function, with no clinically meaningful differences in safety or effectiveness. They’ve saved over $56 billion since their launch and are now cutting cancer drug costs in half in some cases.
Why aren’t more doctors prescribing generics?
Many doctors do. But some still default to brand names out of habit, lack of updated training, or pressure from pharmaceutical reps. Others aren’t aware that a generic is available or that a biosimilar has been approved. Patient education helps: if you ask your doctor, “Is there a generic or biosimilar option?” you’re more likely to get a lower-cost alternative. Pharmacists can also help by suggesting substitutions when appropriate.
Will my insurance cover biosimilars?
Most commercial insurers and Medicare Part D plans now cover biosimilars, often with lower co-pays than the original biologic. Some plans even require you to try a biosimilar first. Check your plan’s formulary or call your insurer. If your doctor prescribes a biologic and a biosimilar is available, ask your pharmacist if your plan will cover the cheaper option. Many patients have saved thousands per year just by switching.
Final Thought: The System Works-If We Let It
Generic drugs aren’t magic. They’re the result of smart policy, fierce competition, and a regulatory system that rewards efficiency. The numbers don’t lie: 90% of prescriptions, 12% of spending. That’s the definition of value.
The real problem isn’t the generics. It’s the barriers keeping them from reaching everyone. Patent abuse. Outdated laws. Lack of awareness. But change is coming. More approvals. More competition. More savings.
If you’re paying full price for a brand-name drug, you’re not just overpaying-you’re missing out on a system designed to help you. Ask the question. Check the price. Switch when you can. Your wallet-and your health-will thank you.







Gilbert Lacasandile
December 8, 2025 AT 12:16Man, I had no idea generics saved us $445 billion last year. I switch everything to generic now-metformin, lisinopril, even the stupid allergy pills. My pharmacist gives me side-eye if I ask for brand. I’m not paying $150 for something that works the same for $8.
Also, GoodRx saved me $120 on my cholesterol med last month. Cash price was cheaper than my insurance co-pay. Who knew?
Guylaine Lapointe
December 8, 2025 AT 14:58It’s not just about savings-it’s about ethics. Big Pharma exploits patent loopholes like a cartel, while patients choose between insulin and rent. This isn’t capitalism; it’s predation dressed up as innovation.
The fact that we need a government to force competition says everything about how broken this system is. And don’t get me started on ‘product hopping’-it’s intellectual theft disguised as R&D.
Also, the FDA’s 99% efficacy claim ignores real-world variability in fillers and coatings. Some of us have *actual* adverse reactions-not placebo, not ‘adjustment.’
Maria Elisha
December 9, 2025 AT 21:35lol i just asked my doc for a generic and she said ‘oh yeah we’ve been doing that for years’ like it was obvious.
turns out i’ve been overpaying for 3 years. $600 a year down the drain. my bad.
also my pharmacist gave me a free bag of gummy vitamins for switching. win win.
Angela R. Cartes
December 10, 2025 AT 22:11Gen Z here. I pay $4 for my anxiety med. Brand? $180. I don’t care if it’s ‘the same.’ I care that I can afford to live.
Also, I don’t trust the FDA anymore. They approved 745 generics last year? That’s like 2 a day. Who’s checking the quality? Who’s even *looking*?
Also, my cousin’s mom had a seizure after switching. So yeah, ‘99% safe’ doesn’t mean much when you’re the 1%. 😐
Anna Roh
December 12, 2025 AT 09:41Generics are fine for most people. But if you’re on something like levothyroxine or warfarin, you don’t mess around. I’ve switched brands three times and each time my TSH went haywire.
It’s not the drug-it’s the fillers. Different binders, different dyes, different absorption rates. My endo won’t let me switch unless it’s the exact same manufacturer.
So yeah, generics save money. But sometimes, your body doesn’t care about the math.
om guru
December 13, 2025 AT 08:39Generic drugs are a triumph of public policy and rational economics. The Hatch Waxman Act was visionary. It enabled competition. It reduced cost. It improved access.
Patent thickets are an abuse of intellectual property rights. Product hopping is market manipulation. These practices must be addressed through legislative reform.
The state must protect the public interest. The market alone cannot be trusted. We must ensure equitable access to essential medicines.
Education is key. Pharmacists must be empowered. Patients must be informed.
Let us move forward with wisdom and integrity.
Katherine Chan
December 13, 2025 AT 09:59Y’all are doing it right. I switched to generic lisinopril last year and I’ve never felt better. My blood pressure is stable, my wallet’s happy, and I’m not stressing about the bill.
Also, biosimilars are the future. My sister’s on one for RA and it cut her costs from $8K to $800 a year. She’s back hiking. She’s back living.
Don’t be scared to ask. Don’t be shy. Your body deserves care. Your bank account deserves peace.
And hey-your pharmacist is your secret weapon. Talk to them. They’re the real MVPs.
❤️
Tiffany Sowby
December 14, 2025 AT 22:41Americans think they’re so smart because they save a few bucks on pills. Meanwhile, China’s building hospitals, India’s manufacturing the drugs, and we’re still arguing about whether a $4 pill is ‘safe’ enough.
Our system is a joke. We pay 5x more than every other developed country. And we think we’re winning because we got a generic?
Wake up. This isn’t freedom. It’s exploitation with a smiley face.
Also, why are we letting Big Pharma dictate our health? We need single-payer. Not more ‘smart choices.’
Asset Finance Komrade
December 15, 2025 AT 03:07One must consider the ontological paradox of pharmaceutical value: if a molecule performs identically, yet costs 1/20th, does it retain the same metaphysical essence?
The brand-name drug carries with it the mythos of innovation, of corporate sacrifice, of the ‘American Dream’ in pill form. The generic? A utilitarian artifact. A commodity stripped of narrative.
Yet the body does not care for mythos. Only bioequivalence.
So perhaps the real tragedy is not the price-but our collective refusal to accept that salvation can be cheap.
🫡
Jennifer Blandford
December 15, 2025 AT 07:21I used to be one of those people who thought generics were ‘lesser.’ Then my mom got diagnosed with diabetes and we couldn’t afford the brand.
We switched to metformin. She’s been stable for 3 years. No side effects. No drama.
She told me last week, ‘Honey, I didn’t know I was paying $100 for a sugar pill.’
Turns out, it’s not a sugar pill. It’s a lifesaver. And we were all just too scared to ask.
So I’m telling you now: ask. Always ask. It’s not weird. It’s brave.
And if you’re reading this? You’re already doing better than most.
💛
Brianna Black
December 16, 2025 AT 04:25As someone who works in global health policy, I’ve seen firsthand how generics transform lives-not just in the U.S., but in Kenya, in Nepal, in rural Mexico.
When a woman in a village can afford insulin because a generic version arrived, she doesn’t just survive-she becomes a mother, a teacher, a community leader.
These aren’t just numbers on a spreadsheet. They’re people. They’re futures.
The real scandal isn’t the cost of generics-it’s that we still have to fight for them in the richest country on Earth.
Let’s not just save money. Let’s save dignity.
Shubham Mathur
December 16, 2025 AT 18:25Generics work. I’ve been taking them for 12 years. No issues. No problems. My dad took them for 20 years. Died at 87. Not because of meds.
Stop overthinking. The science is clear. The FDA is not lying. The math is not a lie.
Ask your pharmacist. Use GoodRx. Switch. Save.
And if you’re still scared? Talk to your doctor. Don’t just assume. Don’t just pay. Do something.
Life is too short for overpriced pills.
Ruth Witte
December 17, 2025 AT 21:40Just switched my asthma inhaler to a biosimilar. Cost went from $500 to $45. I cried. Not because I was sad. Because I could finally breathe without panic.
Also, my dog got a new toy today. I didn’t buy it. I saved it. From meds.
So yeah. This isn’t just about money.
It’s about being able to play with your dog.
❤️🐶