Ear Infection Headache Symptom Checker
This interactive tool helps you assess whether your headache might be related to an ear infection. Based on your symptoms and risk factors, it provides guidance on whether you should seek medical care. Remember: this is not a diagnostic tool but a screening aid.
Ever wondered why a simple ear infection can leave you clutching your head in pain? You’re not alone. The link between headaches and ear infections is tighter than most people think, and understanding it can save you trips to the clinic-or at least help you know when they’re truly needed.
Key Takeaways
- Ear infections (especially middle‑ear otitis media) often cause pressure changes that trigger headache pain.
- Symptoms overlap with sinusitis, dental issues, and, in rare cases, meningitis.
- Adults and children experience the same mechanisms, but children report ear pain more frequently.
- Most headaches from ear infections improve with proper treatment of the infection and simple pain‑relief measures.
- Seek urgent care if you notice fever, swelling behind the ear, or neurological signs such as confusion.
How Ear Infections Cause Headaches
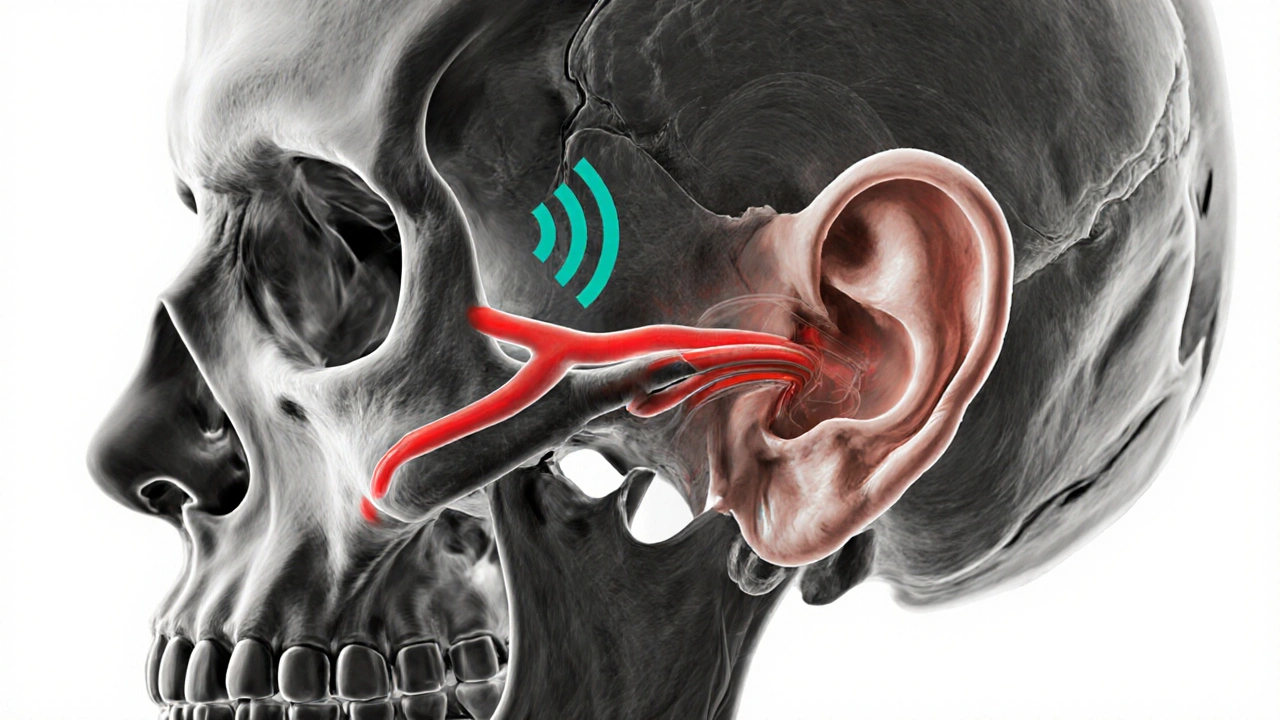
To see why the pain spreads, we need to look at the anatomy. The middle ear the air‑filled space behind the eardrum that vibrates sound waves is connected to the back of the throat by the Eustachian tube a narrow channel that equalises pressure between the middle ear and the nasopharynx. When a bacteria or virus invades, fluid builds up, swelling blocks the tube, and pressure rises.
This pressure doesn’t stay confined to the ear. The skull’s interior is a tightly linked network of nerves and blood vessels. The trigeminal nerve the main facial sensory nerve that also supplies the front of the head shares pathways with the auditory nerves. Increased pressure irritates the trigeminal branches, sending pain signals that the brain interprets as a headache.
In children, the Eustachian tube is shorter and more horizontal, making blockage even more likely. That’s why toddlers often present with ear‑related headaches before any obvious ear pain is noticed.
Common Symptoms Overlap
Because the same nerves serve both ears and the sinuses, the symptom list can be confusing. Below is a quick cheat‑sheet to differentiate an ear‑infection headache from other common headache triggers.
- Location: Ear‑infection pain often feels deep behind the ear or around the cheekbone, whereas sinus headaches are centered in the forehead or bridge of the nose.
- Sound sensitivity: A popping or muffled sound is a giveaway for middle‑ear involvement.
- Fever: Low‑grade fevers (<38°C) are common with otitis media; high fevers (>39°C) may point to more serious infections like meningitis.
- Neck stiffness: If the neck is stiff, think meningitis and seek emergency care.
When to Seek Medical Help
Most ear‑infection headaches resolve on their own or with a short course of antibiotics. However, certain red flags demand prompt evaluation:
- Fever above 39°C lasting more than 24hours.
- Swelling or redness behind the ear (possible mastoiditis).
- Sudden, severe headache with vomiting or altered consciousness.
- Persistent ear pain beyond 72hours despite over‑the‑counter pain relief.
- Hearing loss or ringing (tinnitus) that does not improve.
Both pediatric and adult patients should be taken seriously when these signs appear. A quick visit to a primary‑care physician or an urgent‑care clinic can rule out complications such as mastoiditis infection of the bone behind the ear that can spread to the brain or meningitis.
Treatment Options
Once a healthcare provider confirms an ear infection, the treatment plan usually follows a tiered approach.
- Antibiotics: For bacterial otitis media, amoxicillin or a macrolide is standard. Antibiotics medications that kill or inhibit bacterial growth typically improve symptoms within 48hours.
- Pain relief: Acetaminophen or ibuprofen can lower both fever and headache intensity. Pain relief over‑the‑counter analgesics for symptom management is safe for most ages when dosed correctly.
- Warm compress: Applying a warm cloth to the affected side can loosen fluid and ease pressure.
- Decongestants: For adults, oral pseudoephedrine or nasal saline sprays help open the Eustachian tube.
- Watchful waiting: In children over 2years with mild symptoms, doctors may monitor for 48‑72hours before prescribing antibiotics, as many infections resolve spontaneously.
If the headache persists after the infection clears, consider a follow‑up to rule out lingering inflammation or referred pain from the temporomandibular joint (TMJ).

Prevention Tips
Keeping the middle ear clear is the best defense.
- Breastfeed infants for at least the first six months - it reduces bacterial colonisation.
- Avoid exposure to tobacco smoke; secondhand smoke irritates the Eustachian tube.
- Practice good hand hygiene during cold and flu season.
- Use a humidifier in dry environments to keep nasal passages moist.
- Stay up‑to‑date on the pneumococcal and influenza vaccines, which lower the risk of secondary ear infections.
Comparison: Ear Infection vs Sinusitis Headaches
| Feature | Ear Infection Headache | Sinusitis Headache |
|---|---|---|
| Typical Location | Behind the ear, cheekbone, or temple | Forehead, bridge of nose, maxillary area |
| Associated Ear Symptoms | Muffled hearing, ear pressure, popping | None |
| Associated Nasal Symptoms | Occasional congestion | Thick nasal discharge, facial fullness |
| Response to Decongestants | Often improves pressure | Usually provides relief |
| Common Triggers | Upper‑respiratory infection, allergies, barometric changes | Allergies, viral colds, dental infection |
Frequently Asked Questions
Can an ear infection cause a migraine?
Typically, ear infections trigger tension‑type or pressure headaches rather than true migraines. However, the stress of persistent pain can lower a migraine threshold in people already prone to them.
How long does a headache last after the ear infection clears?
Most patients feel relief within 24‑48hours once the infection resolves. If pain lingers beyond a week, it may be referred pain from the TMJ or lingering inflammation that needs a follow‑up.
Are over‑the‑counter antibiotics effective for ear‑infection headaches?
No. Antibiotics require a prescription. For symptom relief, acetaminophen or ibuprofen are safe choices. If bacterial infection is confirmed, a doctor‑prescribed antibiotic will treat the underlying cause.
Should I use ear drops for pain?
Ear drops are useful only if the eardrum is intact and the pain is from outer‑ear (exterior) infection. For middle‑ear issues, drops do not reach the site of inflammation and provide little benefit.
Can allergies cause both ear infections and headaches?
Yes. Allergic inflammation can block the Eustachian tube, leading to fluid buildup and infection, while also irritating sinus passages and triggering headaches.






Penny X
October 15, 2025 AT 13:43It is incumbent upon each of us to acknowledge the moral imperative of recognizing how seemingly innocuous ear infections can precipitate severe cranial distress. One must not dismiss these ailments as merely trivial, for doing so undermines our collective responsibility to promote health literacy. The intertwining of otologic pathology with headache syndromes exemplifies the interconnectedness of bodily systems, a fact that should inspire ethical vigilance. By embracing a proactive stance, we honor both scientific truth and societal duty.
olivia guerrero
October 28, 2025 AT 00:43Wow!! This article really shines a light on a hidden health issue!!!, and it's so encouraging to see such comprehensive detail!!!, keep spreading the knowledge!!!!
Mark Eddinger
November 9, 2025 AT 12:43Ear infections initiate a cascade of physiological events that can readily culminate in cranial discomfort.
The obstruction of the Eustachian tube creates a pressure differential between the middle ear and the nasopharynx.
This pressure stimulus is transmitted via the tensor tympani and the stapedius muscles to adjacent neural pathways.
Notably, the trigeminal nerve shares afferent connections with the auditory system, providing a conduit for pain signals.
When the pressure exceeds a critical threshold, nociceptors within the mucosal lining become activated.
The central processing centers in the brainstem interpret these signals as headache pain rather than isolated ear pain.
In pediatric patients, the anatomical configuration of a shorter, more horizontal Eustachian tube predisposes them to higher pressure buildup.
Consequently, children often present with headache symptoms before overt otalgia becomes apparent.
Clinical observation demonstrates that timely administration of antibiotics or anti-inflammatory agents reduces the inflammatory edema.
This reduction restores patency to the Eustachian tube, thereby normalizing middle‑ear pressure.
Adjunctive measures such as warm compresses and decongestants further expedite fluid drainage.
Moreover, adequate hydration and avoidance of tobacco smoke limit mucosal irritation.
For patients with recurrent episodes, vaccination against common respiratory pathogens has been shown to decrease incidence.
Should red‑flag symptoms such as high fever, mastoid swelling, or neurological deficits emerge, urgent medical evaluation is warranted.
In summary, understanding the mechanistic link between otitis media and cephalic pain empowers clinicians and patients to intervene early and mitigate suffering.
Graham Smith
November 22, 2025 AT 00:43The description is accurate, however teh pressure dynamics could be further clarified. I reserve my judgement pending more data.
Jeremiah Morgan
December 4, 2025 AT 12:43I wholeheartedly agree with the preceding points, yet I note a minor slip in the spelling of 'eustachian' which is common in hurried drafts. Nonetheless, the essence remains crystal clear.
nina greer
December 17, 2025 AT 00:43The discourse surrounding otologic cephalgia is undeniably superfluous.
Montague Tilmen
December 29, 2025 AT 12:43This American health crisis would vanish if we stopped pandering to foreign medical advice and returned to homegrown, proven treatments!
Roberta Giaimo
January 11, 2026 AT 00:43I appreciate your thorough analysis and the practical tips you provided :)
Tom Druyts
January 23, 2026 AT 12:43Let’s power through the pain with warm compresses, hydration, and a positive mindset-together we can conquer those headaches!
Julia C
February 5, 2026 AT 00:43It’s absurd how the medical establishment keeps us in the dark about the real dangers of ear infections-maybe they’re hiding a larger agenda! Honestly, I’m too tired to care about the minutiae when the system seems rigged. The whole thing feels like a staged performance. I could write a whole novel about it, but I’m feeling lazy right now.
Brooke Bevins
February 17, 2026 AT 12:43I hear your frustration, and it’s valid-dealing with persistent pain is exhausting 😠-but channeling that anger into proactive self‑care can make a real difference.