TCA Side Effects Calculator
TCA Side Effects Calculator
Your Side Effect Profile
Potential Side Effects
Safety Assessment
Recommended Actions
Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline aren’t the first choice for depression anymore-but they’re still used. A lot. Why? Because for some people, nothing else works. Especially when it comes to chronic pain, migraines, or depression that won’t budge after trying SSRIs. But here’s the catch: these drugs come with a long list of side effects that can make daily life harder than the condition they’re meant to treat.
How TCAs Work (And Why They Cause So Many Side Effects)
TCAs were developed in the 1950s, long before SSRIs like Prozac or Zoloft existed. They work by blocking the reuptake of serotonin and norepinephrine, two brain chemicals tied to mood and pain signals. But unlike newer antidepressants, TCAs don’t just target those two systems. They also mess with other receptors in your body-cholinergic, histamine, and alpha-adrenergic receptors. That’s why a drug meant for depression can leave you with a dry mouth, blurry vision, constipation, and a racing heart.
Think of it like using a sledgehammer to fix a watch. It gets the job done, but it breaks a lot of other parts along the way. Amitriptyline, for example, has a strong grip on muscarinic receptors (which control saliva, digestion, and bladder function) and histamine receptors (which make you sleepy). Nortriptyline, its cousin, is a bit gentler. It doesn’t bind as tightly to those receptors, so side effects are usually milder. That’s why doctors often switch patients from amitriptyline to nortriptyline when side effects become too much.
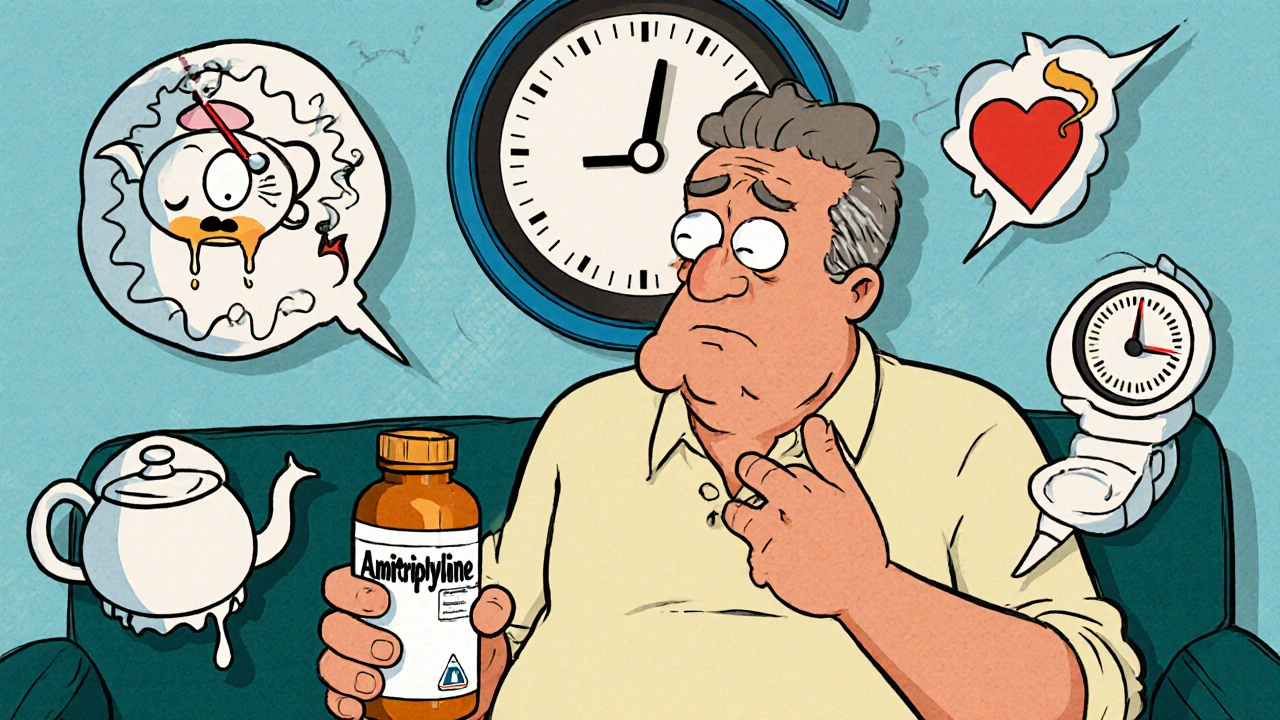
Common Side Effects: The Daily Annoyances
Most people on TCAs will run into at least one of these issues within the first few weeks:
- Dry mouth-affects up to 30% of people on amitriptyline. It’s not just uncomfortable. It leads to tooth decay, gum disease, and bad breath. One user on Reddit said they went through three bottles of Biotene a week and still got two cavities.
- Blurred vision-happens in 15-20% of users. It usually clears up after a few weeks, but some people report trouble reading or driving until they adjust.
- Constipation-20-25% of users struggle with this. It’s not just a nuisance. Severe cases can lead to bowel obstruction, especially in older adults.
- Urinary retention-10-15% of people, especially men with enlarged prostates, have trouble emptying their bladder. Some end up needing a catheter.
- Drowsiness-up to 40% of people on amitriptyline feel like they’re walking through syrup. Nortriptyline is better, but still causes drowsiness in about 25% of users. That’s why these meds are usually taken at night.
- Orthostatic hypotension-a sudden drop in blood pressure when standing up. You feel dizzy, lightheaded, or even faint. This increases fall risk, especially in older adults.
- Tachycardia-resting heart rate can jump by 10-20 beats per minute. Not dangerous for everyone, but risky if you already have heart problems.
These aren’t rare side effects. They’re the norm. And they’re why so many people quit TCAs within the first two months. One study found that 45% of patients stopped taking TCAs because of side effects-compared to just 25% for SSRIs.
Serious Risks: What You Need to Watch For
Some side effects aren’t just annoying-they’re life-threatening.
Heart problems are the biggest concern. TCAs can prolong the QTc interval on an ECG, which can trigger dangerous heart rhythms. Amitriptyline, in particular, can lengthen this interval by 20-40 milliseconds. For someone with existing heart disease, that’s a red flag. A 2019 Lancet study found TCAs increased the risk of cardiovascular events by 35% compared to SSRIs.
Overdose is another scary reality. TCAs have a narrow safety margin. Taking just a few extra pills can be fatal. Symptoms include a widened QRS complex on ECG, dangerously low blood pressure, seizures, and respiratory failure. The mortality rate per prescription is higher than for any other antidepressant. That’s why doctors keep a close eye on dosing and never prescribe large quantities at once.
Cognitive issues are common in older adults. About 25% of people over 65 on TCAs report confusion. 15% become disoriented. The Beers Criteria, a guide for safe prescribing in seniors, specifically says to avoid amitriptyline and other high-anticholinergic TCAs because they raise the risk of dementia and falls by 70%.
Why Doctors Still Prescribe Them
If TCAs are so risky, why are they still around?
Because they work-better than other drugs-for certain conditions.
- Neuropathic pain: Amitriptyline is one of the most effective drugs for diabetic nerve pain, postherpetic neuralgia, and fibromyalgia. A 2020 Cochrane review found it helped 35-40% of patients reduce pain by at least half. That’s better than duloxetine or gabapentin.
- Migraine prevention: For people who get 10+ migraines a month, low-dose amitriptyline can cut attacks in half. One user on Healthgrades said it dropped their migraines from 15 to 3 per month.
- Treatment-resistant depression: When SSRIs and SNRIs fail, TCAs still have a 65-70% response rate. That’s higher than newer drugs.
Dr. Robert Baldassano from the University of Pennsylvania put it simply: “For certain nerve pain conditions, amitriptyline remains the gold standard.”
Amitriptyline vs. Nortriptyline: Which Is Better?
Not all TCAs are created equal. Here’s how they stack up:
| Feature | Amitriptyline | Nortriptyline |
|---|---|---|
| Primary use | Depression, neuropathic pain, migraines | Depression, neuropathic pain (milder side effects) |
| Typical starting dose | 25-50 mg daily | 25 mg daily |
| Max dose | 150-200 mg daily | 100-150 mg daily |
| Sedation | High (up to 40%) | Moderate (about 25%) |
| Anticholinergic effects | Strong (dry mouth, constipation, urinary retention) | Milder |
| Cardiac risk | Higher | Lower |
| Best for | Severe pain, treatment-resistant depression | Older adults, patients sensitive to side effects |
Nortriptyline is often the better pick for older patients or those with heart issues. Amitriptyline is more potent for pain but harder to tolerate. Many patients start on amitriptyline and switch to nortriptyline once their pain is under control.

Who Should Avoid TCAs?
These medications aren’t safe for everyone:
- People with heart disease, especially arrhythmias or recent heart attacks
- Those with glaucoma (TCAs can raise eye pressure)
- Men with enlarged prostates (risk of urinary retention)
- Anyone over 65-unless no other option exists
- People taking MAO inhibitors (dangerous interaction)
- Pregnant or breastfeeding women (limited safety data)
The American Psychiatric Association says TCAs should only be used after two failed trials of newer antidepressants. That’s not because they’re ineffective-it’s because the risks often outweigh the benefits for most people.
How to Use TCAs Safely
If your doctor prescribes a TCA, here’s how to reduce the risks:
- Start low: Begin with 10-25 mg at bedtime. This helps with sleep and reduces daytime drowsiness.
- Go slow: Increase the dose by 10-25 mg every 1-2 weeks. Don’t rush it. Your body needs time to adjust.
- Stand up slowly: To avoid dizziness from low blood pressure, pause for a few seconds before standing.
- Brush and floss daily: Use sugar-free gum or Biotene spray to fight dry mouth. See your dentist every 6 months.
- Get an ECG: Especially if you’re over 50 or have heart issues. Monitor for QTc prolongation.
- Don’t quit cold turkey: Stopping suddenly can cause withdrawal symptoms like electric shock sensations, nausea, or anxiety. Taper over 4-6 weeks.
Also, give it time. TCAs take 2-4 weeks to work. Many people quit too early, thinking it’s not helping. But if you stick with it, you might find relief where other drugs failed.
What Comes Next?
TCAs are fading from first-line use, but they’re not disappearing. New research is looking at combining low-dose amitriptyline with SSRIs to get the benefits with fewer side effects. Pharmacogenetic testing is also emerging-some people have genetic variants that make them process TCAs too slowly, leading to toxic buildup. Testing for CYP2D6 metabolism could help avoid dangerous side effects before they start.
For now, TCAs remain a powerful, if risky, tool. They’re not for everyone. But for someone with debilitating nerve pain or depression that won’t respond to anything else, they can be a lifeline.
As Dr. Charles Nemeroff, Editor-in-Chief of The American Journal of Psychiatry, said in 2023: “When used judiciously in appropriately selected patients with careful monitoring, TCAs can provide life-changing benefits that newer medications cannot match for certain individuals.”
Do tricyclic antidepressants cause weight gain?
Yes, weight gain is common. Most users report gaining 10-15 pounds in the first 6 months. This happens because TCAs increase appetite and slow metabolism. Amitriptyline is more likely to cause weight gain than nortriptyline. If weight gain becomes a problem, talk to your doctor about switching to a different medication or adjusting your diet and activity level.
Can I drink alcohol while taking amitriptyline?
No. Alcohol makes the sedative effects of TCAs much stronger. It can lead to extreme drowsiness, dizziness, and even dangerous drops in blood pressure. It also increases the risk of falls and accidents. Even one drink can be risky. Avoid alcohol completely while taking these medications.
How long does it take for nortriptyline to work for nerve pain?
For nerve pain, nortriptyline usually starts working within 1-2 weeks, but full effects can take 4-6 weeks. Unlike depression, where you need 2-4 weeks to feel better, pain relief often comes sooner. Keep taking it even if you don’t notice changes right away. Don’t stop unless your doctor tells you to.
Are tricyclic antidepressants addictive?
No, TCAs are not addictive in the way opioids or benzodiazepines are. You won’t crave them or get high from them. But your body can become physically dependent. Stopping suddenly can cause withdrawal symptoms like nausea, headaches, anxiety, and electric shock sensations. Always taper off slowly under medical supervision.
Is amitriptyline safe for elderly patients?
Generally, no. The Beers Criteria strongly advises against using amitriptyline in people over 65. It increases the risk of confusion, memory problems, falls, and hip fractures by up to 70%. Nortriptyline is a safer option for older adults, but even then, it should be used with caution and at the lowest possible dose.
What should I do if I miss a dose of nortriptyline?
If you miss a dose, take it as soon as you remember-unless it’s close to your next scheduled dose. Don’t double up. If you’re taking it at night and remember in the morning, skip it and wait until the next night. Missing doses can cause withdrawal symptoms like headaches or mood swings. Set a daily alarm to stay on track.
Can TCAs cause sexual side effects?
Yes. About 35-40% of male users report reduced libido, erectile dysfunction, or delayed orgasm. Women may experience decreased arousal or difficulty reaching orgasm. These side effects are similar to SSRIs but often more pronounced with TCAs. If this becomes a problem, talk to your doctor. Lowering the dose or switching to nortriptyline may help.
Do I need blood tests while taking TCAs?
Not routinely, but your doctor may order a blood test to check your TCA levels if side effects are severe or if you’re not responding. This is especially true if you’re taking amitriptyline and have liver or kidney issues. Genetic testing for CYP2D6 metabolism is also becoming more common to predict how you’ll process the drug.
Tricyclic antidepressants are not for everyone. But for some, they’re the only thing that brings relief. The key is knowing when they’re worth the risk-and how to use them safely when they are.




Andy Feltus
November 19, 2025 AT 22:23It's funny how we treat brain chemistry like a leaky faucet you can just turn off. TCAs are the pharmaceutical equivalent of duct tape and prayer - they hold the damn thing together, even if everything else is rusting. We call them 'outdated,' but maybe we just don't want to admit that some problems don't have elegant solutions. Sometimes you need the sledgehammer. Sometimes you just need to stop crying about the broken watch and fix the damn pain.
And yes, I've been on amitriptyline for seven years. Dry mouth? Check. Blurry vision? Still here. Constipation? My colon has filed a formal complaint. But I can walk again. So yeah. I'll take the side effects. You don't get to judge a lifeline until you've been drowning.
Brian Rono
November 20, 2025 AT 18:43Let’s be brutally honest: TCAs are the opioid of psychiatry. A 1950s relic masquerading as a solution because Big Pharma ran out of novel mechanisms and the FDA stopped caring about safety margins. You call it ‘gold standard’ for neuropathic pain? No - you call it ‘last resort because everything else failed and the insurance won’t cover ketamine.’
And don’t get me started on the QTc prolongation. You’re prescribing a drug that can induce torsades de pointes to someone with a family history of sudden cardiac death? That’s not medicine. That’s Russian roulette with a prescription pad. The fact that this is still in the Beers Criteria and people still prescribe it like it’s Prozac speaks volumes about how broken our system is.
seamus moginie
November 21, 2025 AT 12:29As someone who has lived with chronic pain for over a decade, I can say without hesitation that nortriptyline saved my life. I was on 12 different medications before this. Every one failed. Every one left me worse. I was bedridden. Depressed. Alone.
Then I tried 25mg of nortriptyline. Didn’t work for a month. Then - slowly - the fog lifted. The pain dulled. I started walking again. I started laughing again.
Yes, I have dry mouth. Yes, I get dizzy. Yes, I had to change my diet. But I’m alive. And I’m not ashamed of what works. If you’re too scared to use a tool because it’s old, you’re not being cautious - you’re being cowardly.
Sam Reicks
November 23, 2025 AT 12:10Did you know the FDA knew about the cardiac risks in the 80s but didn’t act because the pharmaceutical lobby said it would hurt profits? And now they’re still selling this like it’s safe? They’re not even monitoring people properly. My uncle died on amitriptyline. ECG was never done. He was 68. They said he had a ‘heart attack’ - no mention of the drug.
And the weight gain? That’s not a side effect - that’s a design feature. They want you dependent. More pills. More doctor visits. More money. They don’t care if you live - they care if you keep buying.
They’re hiding the data. You think this is science? It’s corporate theater.
Frank Dahlmeyer
November 23, 2025 AT 21:38Look - I get it. You’re scared. You’ve read the side effect list and your heart is racing. But here’s the thing: medicine isn’t about avoiding risk - it’s about managing it. TCAs aren’t perfect. No drug is. But for someone with severe neuropathic pain, the alternative isn’t ‘better drugs’ - it’s morphine, or spinal cord stimulators, or nerve ablations - all of which cost $50k+, require surgery, and have their own horror stories.
I’ve seen patients on TCAs who were wheelchair-bound for years get back to gardening. Back to playing with their grandkids. Back to life.
Yes, you need monitoring. Yes, you need to start low. Yes, you need to be honest with your doctor. But don’t throw out a tool that’s saved thousands just because it’s not shiny and new. That’s not progress - that’s nihilism dressed up as caution.
Codie Wagers
November 24, 2025 AT 00:33You call this ‘life-changing’? Let me reframe it: you’re trading your dignity for relief. Dry mouth? You’re a walking desert. Blurred vision? You can’t read your own child’s handwriting. Constipation? You’re bloated like a Thanksgiving turkey. Drowsiness? You’re a zombie at 3pm. Weight gain? Your body becomes a monument to pharmaceutical neglect.
And you call that a win? No. You call it surrender. And worse - you call it courage. It’s not courage. It’s resignation. There are better ways. Ketamine. TMS. Even psychedelics now. But you’d rather cling to a 70-year-old relic because it’s cheap and your insurance covers it. That’s not healing. That’s settling.
Paige Lund
November 24, 2025 AT 19:07So… I can’t drink alcohol. Got it. Thanks for the 2000-word essay on how my liver is now a cautionary tale. I’ll just go back to crying in the shower like before. 🙃
Timothy Reed
November 26, 2025 AT 03:27For anyone considering TCAs: this post is one of the most balanced, well-researched summaries I’ve seen. It doesn’t sugarcoat the risks - and it doesn’t dismiss the benefits. If you’re struggling with treatment-resistant depression or chronic pain, this is exactly the kind of information you need before making a decision.
Start low. Go slow. Track your symptoms. Talk to your doctor. Don’t quit because of day 3 drowsiness. Give it 6 weeks. And if it works - even partially - it’s worth the trade-offs. You’re not broken for needing this. You’re resilient for seeking it.
harenee hanapi
November 26, 2025 AT 08:08I’ve been on amitriptyline for 3 years. I gained 47 pounds. My hair fell out. I couldn’t orgasm. My husband left me because I was ‘emotionally unavailable’ - which is code for ‘I’m too tired and dry and numb to care.’
And now I’m on SSRIs. And I’m still in pain. But at least I can kiss my kids without feeling like a robot who forgot how to feel.
So yes - TCAs work. But they don’t care if you live. They just care if you take them.
And now I’m the girl who cries in the pharmacy aisle because she can’t afford ketamine. And nobody says a word. 🤍
Christopher Robinson
November 27, 2025 AT 17:27Just wanted to say - if you're on TCAs and you're reading this, you're not alone. I've been on nortriptyline for 5 years. Dry mouth? Yeah. Blurry vision? Still here. But I can work. I can hug my daughter. I can sleep through the night without screaming.
Also - Biotene is a miracle. Sugar-free gum. Water bottles everywhere. And I take it at 8pm like clockwork. 📅💧
You don't have to be ‘cured’ to be healed. You just have to be able to breathe again. And for some of us? That’s enough.
💙
James Ó Nuanáin
November 27, 2025 AT 23:50It is a matter of profound national shame that the United Kingdom’s National Health Service continues to prescribe these antiquated and hazardous agents to vulnerable populations. In the United Kingdom, we have long since moved beyond such barbaric pharmacological interventions. We now employ precision medicine, cognitive behavioural therapies, and neurostimulation techniques that are not only more efficacious but ethically superior.
That British citizens are still being subjected to this 1950s-era pharmacological malpractice is a scandal - and one that must be addressed with immediate legislative intervention. This is not healthcare. This is negligence dressed in a white coat.
Angela Gutschwager
November 28, 2025 AT 17:22My doctor prescribed me amitriptyline for migraines. I took it for 2 weeks. Got dizzy. Couldn’t focus. Gained 8 pounds. Headaches didn’t improve.
Quit. Now I take CBD oil and cry less. 😌
Dion Hetemi
November 29, 2025 AT 08:16Let’s not romanticize this. TCAs are the pharmaceutical equivalent of a chainsaw used to trim hedges. Sure, it cuts - but it also maims. The fact that 45% of people quit because of side effects isn’t ‘resilience’ - it’s a warning sign. And the cardiac risks? That’s not ‘careful monitoring.’ That’s gambling with someone’s life.
And the ‘gold standard’ nonsense? That’s just corporate propaganda wrapped in clinical language. There’s no such thing as a ‘gold standard’ when the cost is your heart, your bladder, your libido, your dignity.
They’re not ‘still used because they work.’ They’re still used because nobody’s funding the alternatives - and because the people who need them most can’t afford the real solutions.
So yeah. They work. But they’re a symptom of a broken system. Not a solution.