Hypertension Safety: What You Need to Know About Medications and Risks
When you have hypertension, a chronic condition where blood pressure stays too high, putting stress on your heart and arteries. Also known as high blood pressure, it’s one of the most common health issues worldwide—and one of the most dangerous if not managed carefully. Taking medication is often necessary, but safety doesn’t end at the prescription bottle. Many people don’t realize that the real risks come from what they mix it with, how long they take it, or ignoring early warning signs like dizziness, swelling, or unusual fatigue.
Blood pressure medications, including ACE inhibitors, beta-blockers, diuretics, and calcium channel blockers, work differently for everyone. Some cause dry cough, others lead to leg swelling or low potassium. And here’s the part most skip: combining them with over-the-counter painkillers like ibuprofen, cold medicines, or even certain herbal teas can spike your pressure or damage your kidneys. A study from the American Heart Association found that nearly 1 in 5 hospitalizations for uncontrolled hypertension were linked to hidden drug interactions—not missed doses.
Medication interactions, especially with common OTC drugs and supplements, are a silent threat. For example, decongestants in cold remedies can undo weeks of blood pressure control. Grapefruit juice? It can make some pills too strong. Even magnesium supplements, often taken for muscle cramps, can interfere with certain diuretics. You don’t need to avoid everything—but you do need to know what’s in your medicine cabinet and talk to your doctor before adding anything new.
Then there’s the long-term stuff. Taking high blood pressure meds for years can lead to side effects that sneak up: kidney changes, electrolyte imbalances, or even sexual dysfunction. That’s why regular checkups aren’t optional—they’re part of the treatment. Monitoring your numbers at home, tracking symptoms, and knowing when to call your doctor (not wait for your next appointment) makes a real difference.
Hypertension safety isn’t about perfection. It’s about awareness. It’s knowing that your pill isn’t magic—it’s a tool that needs the right environment to work. That means avoiding salt bombs, staying active, and speaking up when something feels off. The posts below cover exactly these real-world situations: how certain drugs cause rebound issues, what happens when you mix blood pressure meds with other treatments, how to spot kidney stress from long-term use, and why switching meds isn’t as simple as it sounds. You’ll find practical advice from people who’ve been there—not theory, not brochures, but what actually works when your body says no.
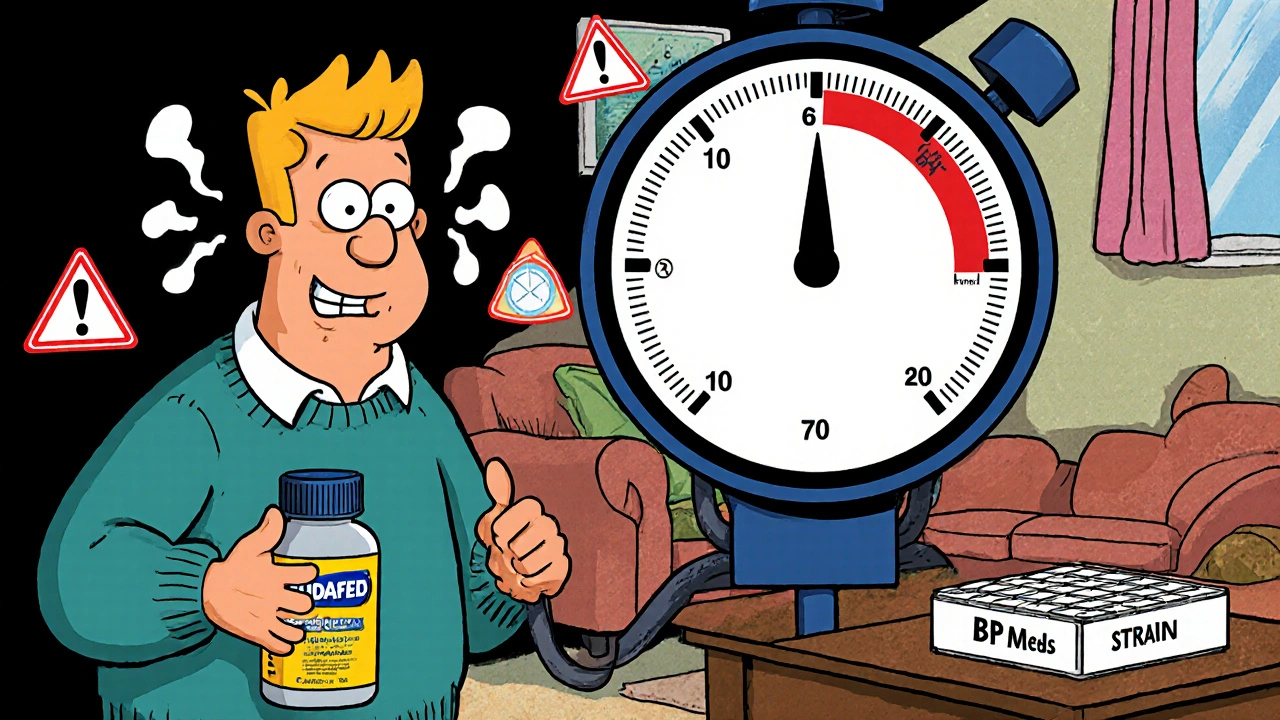
Nasal Decongestants and Blood Pressure Medications: What You Need to Know for Safe Use
Nasal decongestants can dangerously raise blood pressure, especially when taken with hypertension medications. Learn which ingredients to avoid, safe alternatives, and how to protect your heart when you have a cold.




