Gut-Skin Connection Symptom Checker
Answer the following questions to identify possible connections between your gut symptoms and skin rashes:
Answer the questions above to see potential connections between your gut health and skin symptoms.
Key Takeaways
- A disrupted gut microbiome can provoke inflammation that shows up as skin rashes.
- Conditions like Celiac disease, IBD, IBS, and food allergies often have recognizable skin signs.
- Identifying the gut‑skin link involves tracking GI symptoms, rash patterns, and dietary triggers.
- Probiotic‑rich foods, targeted elimination diets, and medical treatment can break the cycle.
- Seek a dermatologist or gastroenterologist if rashes persist despite lifestyle changes.
If you’re dealing with a persistent skin rash, the gut might be the hidden culprit. The connection between the skin and the gastrointestinal (GI) tract isn’t new-doctors have observed it for centuries-but recent research on the gut microbiome has clarified why a problem in one organ often mirrors itself on the other.
Below we’ll unpack the most common GI‑related skin conditions, explain the biological mechanisms that link the gut to the skin, and give you a practical roadmap for spotting the link and managing it.
How Gut Health Affects the Skin
Both the skin and the gut serve as barriers, host millions of microbes, and communicate with the immune system. When the gut’s ecosystem-known as the gut microbiome is the collection of bacteria, fungi, and viruses that reside in the digestive tract, influencing digestion, immunity, and inflammation gets out of balance, it can set off a chain reaction that ends up on the surface of the body.
Three core pathways bridge gut disturbances to skin eruptions:
- Immune activation: A leaky gut allows bacterial fragments (lipopolysaccharides) to cross into the bloodstream, prompting systemic inflammation that can trigger or worsen rashes.
- Metabolite imbalance: Short‑chain fatty acids and other metabolites produced by healthy gut bacteria help regulate skin cells. When production drops, skin barrier function suffers.
- Histamine overflow: Certain gut bacteria store and release histamine. Overgrowth can elevate circulating histamine, leading to itchiness and hives.
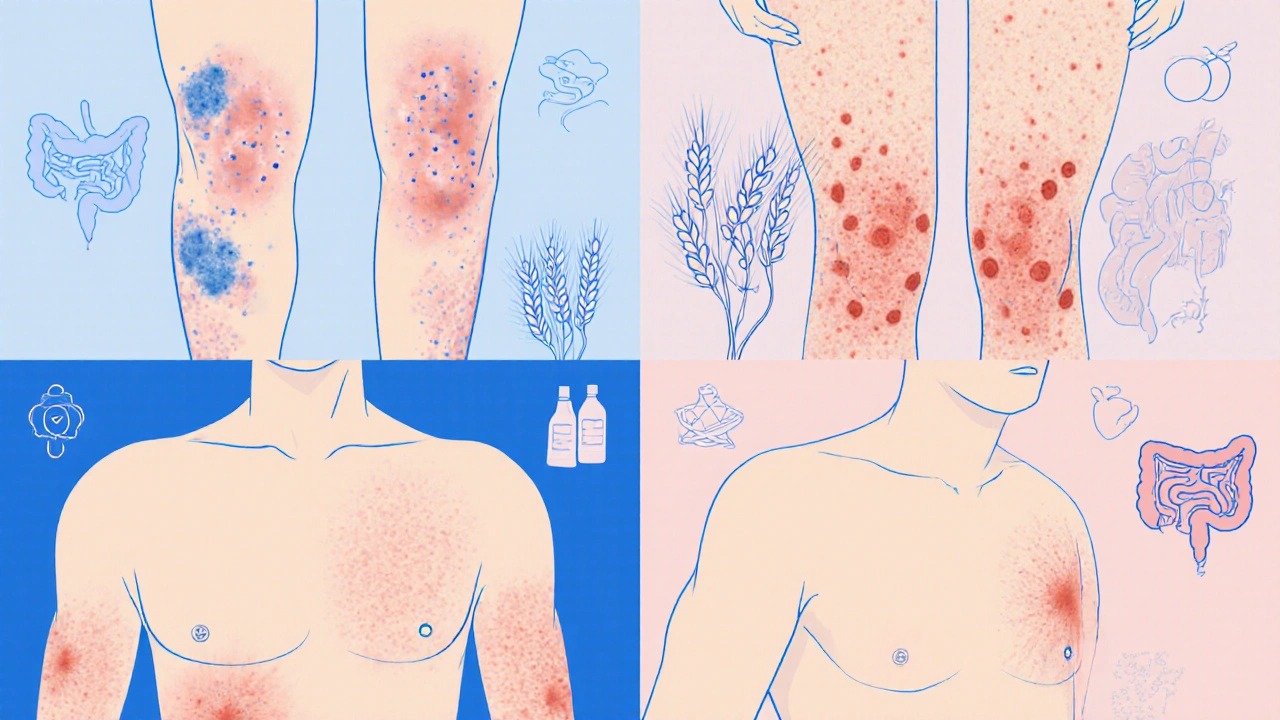
Common GI‑Related Skin Conditions
Below is a quick reference that matches common GI disorders with the skin manifestations they often produce.
| GI Condition | Typical Rash | Key GI Symptoms | Common Triggers | First‑Line Treatment |
|---|---|---|---|---|
| Celiac disease is an autoimmune reaction to gluten that damages the small intestine | Dermatitis herpetiformis (itchy, blistery patches) | Diarrhea, bloating, weight loss | Gluten‑containing grains | Strict gluten‑free diet + dapsone for rash |
| Inflammatory bowel disease (IBD) is a group of chronic inflammatory conditions, chiefly Crohn’s disease and ulcerative colitis | Erythema nodosum, pyoderma gangrenosum | Abdominal pain, blood in stool, fatigue | Stress, smoking, certain food additives | Anti‑inflammatories, biologics, wound care |
| Irritable bowel syndrome (IBS) is a functional GI disorder marked by abdominal pain and altered bowel habits without structural damage | Urticaria (hives), eczema flare‑ups | Cramping, diarrhea or constipation, bloating | FODMAP-rich foods, caffeine, alcohol | Low‑FODMAP diet, probiotics, stress management |
| Food allergy is an immune‑mediated reaction to specific foods, often involving IgE antibodies | Hives, angio‑edema, contact dermatitis | Rapid GI upset, nausea, vomiting | Milk, eggs, nuts, shellfish | Allergen avoidance, antihistamines, epinephrine if severe |
| Histamine intolerance is an inability to break down dietary histamine due to DAO enzyme deficiency | Pruritic papules, flushing, eczema‑like lesions | Diarrhea, abdominal cramping, headache | Aged cheese, fermented drinks, cured meats | Low‑histamine diet, DAO supplements |
Why Rashes Appear: Underlying Mechanisms
Understanding the "why" helps you choose the right intervention. Here are the most common biological routes linking gut problems to skin eruptions:
- Leaky gut syndrome: Tight junctions in the intestinal lining become compromised, allowing food particles and bacterial toxins to seep into the bloodstream. The immune system flags these as threats, releasing cytokines that inflame skin tissue.
- Dysbiosis: An overgrowth of pathogenic bacteria (e.g., Clostridium difficile) or a loss of beneficial strains (e.g., Lactobacillus, Bifidobacterium) skews the immune balance toward Th2‑dominant responses, which drive eczema and hives.
- Malabsorption of nutrients: Deficiencies in zinc, omega‑3 fatty acids, or vitamin D-common in celiac disease and Crohn’s disease-impair skin barrier repair, making rashes more likely.
- Autoimmune cross‑reactivity: In celiac disease, antibodies against gluten also target skin proteins, causing dermatitis herpetiformis. Similar cross‑reactivity appears in psoriasis patients with IBD.
- Histamine overload: Certain gut microbes produce histamine as a by‑product. When those microbes dominate, systemic histamine levels rise, leading to itchiness and urticaria.
Spotting the Link: Symptoms to Watch
Not every rash means a gut problem, but a pattern of signs can tip you off. Keep an eye on these combos:
- Itchy, clustered bumps on elbows or knees that flare after a dairy‑heavy meal.
- Blister‑like patches on the scalp or buttocks that appear alongside chronic diarrhea.
- Sudden hives that develop within an hour of eating fermented foods.
- Erythema nodosum (tender red nodules on shins) coupled with abdominal pain and weight loss.
- Persistent eczema that improves when you start a low‑FODMAP diet.
Maintaining a simple journal-recording meals, GI symptoms, and rash changes-can quickly reveal correlations that would otherwise stay hidden.
Managing the Connection
Because the gut‑skin axis is bidirectional, treating both sides yields the best results. Here’s a step‑by‑step plan you can try before booking a specialist.
- Rule out obvious culprits: If you suspect a food allergy, try an elimination diet for two weeks (remove common allergens like dairy, nuts, gluten). Re‑introduce one at a time while monitoring skin and gut responses.
- Boost gut diversity: Incorporate fermented foods (yogurt, kefir, sauerkraut) or a high‑quality probiotic containing Lactobacillus rhamnosus and Bifidobacterium lactis. Aim for at least 10billion CFU daily.
- Repair the gut lining: Add L‑glutamine (5g twice a day), collagen peptides, and omega‑3 fish oil. Zinc picolinate (15mg) helps skin healing.
- Address inflammation: Curcumin (500mg with black pepper) and quercetin (250mg) have shown to reduce cytokine production in both gut and skin.
- Consider targeted medications: For celiac disease, a strict gluten‑free diet is non‑negotiable. IBD patients may need prescription biologics; consult a gastroenterologist.
- Skin‑focused care: Use gentle, fragrance‑free moisturizers, and include topical steroids or calcineurin inhibitors if inflammation is intense. Avoid harsh scrubs that further damage the barrier.
Remember, lifestyle tweaks often take 4-6weeks to show skin improvement because skin turnover is slow.
When to Seek Professional Help
Self‑management works for mild cases, but see a doctor if you experience any of the following:
- Rash spreading rapidly or accompanied by fever.
- Severe abdominal pain, blood in stool, or unexplained weight loss.
- Persistent itching that disrupts sleep despite antihistamines.
- Signs of nutrient deficiency (hair loss, brittle nails, anemia).
- History of autoimmune disease or a family history of celiac/IBD.
A dermatologist can perform a skin biopsy to confirm conditions like dermatitis herpetiformis, while a gastroenterologist can order blood panels (tTG‑IgA, fecal calprotectin) and endoscopy if needed.
Frequently Asked Questions
Can stress‑induced gut issues cause a rash?
Yes. Stress releases cortisol, which can disrupt gut microbiota and increase intestinal permeability. The resulting inflammation often shows up as eczema or hives. Managing stress with mindfulness, regular exercise, and adequate sleep can reduce both gut and skin flare‑ups.
Is a probiotic safe for someone with IBD?
Most studies suggest specific strains (e.g., Escherichia coli Nissle 1917, Lactobacillus rhamnosus GG) are safe and can even help maintain remission. However, never start a probiotic during an acute flare‑up without doctor approval, as some formulations may cause gas or bloating.
What’s the difference between dermatitis herpetiformis and regular eczema?
Dermatitis herpetiformis is tightly linked to gluten sensitivity and presents as intensely itchy, grouped vesicles usually on elbows, knees, or buttocks. A skin biopsy shows IgA deposits. Regular eczema isn’t tied to a specific food antigen and often appears in flexural areas with dry, scaly patches.
Can a low‑FODMAP diet improve chronic hives?
For many with IBS‑related hives, reducing fermentable carbs lowers gut gas and histamine production, leading to fewer skin reactions. A trial of 4-6 weeks under dietitian guidance can clarify if it helps you.
When should I get tested for celiac disease?
If you have chronic diarrhea, unexplained anemia, or a rash that looks like dermatitis herpetiformis, ask your doctor for serologic tests (tissue transglutaminase IgA). A positive result usually leads to an endoscopic biopsy to confirm.
By paying attention to the tell‑tale signs of gut distress and giving your microbiome the care it needs, you can often calm stubborn skin rashes without endless creams. When the problem persists, remember that a partnership between a dermatologist and a gastroenterologist is the fastest route to relief.





Jenae Bauer
October 9, 2025 AT 12:06The gut whispers, and the skin shouts.
vijay sainath
October 9, 2025 AT 20:26Look, the gut-skin axis isn’t some mystical hype, it’s a measurable cascade of inflammation. When your microbiome is out of whack, endotoxins leak, cytokines surge, and your epidermis lights up like a billboard. Cutting out processed junk and tracking your meals can actually prove the link in real time.
Daisy canales
October 10, 2025 AT 04:46Oh great, another trendy “gut‑skin” thing – because we needed more reasons to diet.
keyul prajapati
October 10, 2025 AT 13:06The relationship between intestinal health and dermatological manifestations has been documented for decades, yet it still surprises many newcomers.
When the mucosal barrier becomes compromised, microbial fragments such as lipopolysaccharides enter systemic circulation, prompting an immune response that often targets peripheral tissues like skin.
This phenomenon is commonly referred to as “leaky gut syndrome,” and it serves as a bridge between gastrointestinal irritation and cutaneous inflammation.
In addition to barrier dysfunction, dysbiosis-an imbalance in the gut microbial community-shifts the metabolic output toward pro‑inflammatory metabolites.
Short‑chain fatty acids, which normally nourish colonocytes and reinforce tight junctions, are depleted, leaving the gut more permeable.
Histamine‑producing bacteria, such as certain strains of Morganella, can also proliferate, raising systemic histamine levels that manifest as pruritus and urticarial eruptions.
Clinically, this is why patients with irritable bowel syndrome frequently report flares of eczema or chronic hives after high‑FODMAP meals.
Moreover, autoimmune conditions like celiac disease generate specific IgA antibodies that deposit in the dermis, producing dermatitis herpetiformis, a blistering rash with a distinctive distribution.
The interplay is further complicated by nutrient malabsorption; deficiencies in zinc, vitamin D, and omega‑3 fatty acids impair keratinocyte function and skin barrier repair.
Therefore, a comprehensive approach that includes both dietary modification and targeted supplementation often yields the most noticeable improvement.
A practical first step is to keep a detailed journal of foods, bowel movements, and skin changes for at least two weeks to identify patterns.
If a clear trigger emerges-say, gluten or fermented dairy-an elimination diet can be instituted under professional guidance.
Probiotic regimens that include strains like Lactobacillus rhamnosus GG and Bifidobacterium lactis have been shown in randomized trials to reduce inflammatory markers and improve rash severity.
For those with severe dysbiosis, a short course of a narrow‑spectrum antibiotic followed by a structured re‑colonization protocol may be warranted, but only after thorough evaluation.
Finally, collaborating with both a dermatologist and a gastroenterologist ensures that both the cutaneous presentation and the underlying gut pathology are addressed concurrently.
In summary, treating the gut‑skin axis requires patience, data‑driven adjustments, and a willingness to explore the interconnectedness of our body systems.
Alice L
October 10, 2025 AT 21:26Esteemed members of this forum, I wish to draw your attention to the substantive evidence linking gastrointestinal dysbiosis with dermatological disorders, a relationship substantiated by peer‑reviewed literature spanning immunology and microbiology. The methodological rigor employed in recent randomized controlled trials underscores the efficacy of probiotic supplementation and targeted elimination diets in ameliorating cutaneous manifestations. I respectfully recommend consultation with qualified healthcare professionals to tailor an evidence‑based therapeutic regimen.
Seth Angel Chi
October 11, 2025 AT 05:46The premise that gut flora influence epidermal health is not merely anecdotal but underpinned by quantifiable cytokine profiles and microbial metabolite analyses.
Kristen Ariies
October 11, 2025 AT 14:06Wow!!! This whole gut‑skin connection is like a backstage drama where the gut steals the spotlight and the skin gets the dramatic encore!!! 🎭✨
Ralph Louis
October 11, 2025 AT 22:26Yo, if your belly’s acting up and you’re freaking out over a rash, it’s probably the microbes throwing a party you didn’t RSVP to-cut the junk, add some kefir, and watch the fireworks calm down.
Angela Allen
October 12, 2025 AT 06:46i totally get how frustrating it is when you try all the creams and nothing works-maybe try keeping a simple food log and see if certain meals line up with the rash.
Christopher Jimenez
October 12, 2025 AT 15:06While many attribute dermatological issues to superficial causes, the literature indicates that up to 30% of chronic urticaria cases have an underlying gastrointestinal trigger, a statistic often overlooked in primary care.
Olivia Christensen
October 12, 2025 AT 23:26Honestly, a quick probiotic trial for a month and watching your diet can make a huge diff 😊
Lauren W
October 13, 2025 AT 07:46Interesting that the article recommends probiotics, yet some studies suggest certain strains may exacerbate histamine intolerance; consider a trial period without them first.
Crystal Doofenschmirtz
October 13, 2025 AT 16:06Could there be a genetic component that predisposes some individuals to a stronger gut‑skin axis response than others?
Pankaj Kumar
October 14, 2025 AT 00:26Hey buddy, think of your gut as the engine and your skin as the paint job-keep the engine clean with diverse veggies and the paint will shine!
sneha kapuri
October 14, 2025 AT 08:46Stop buying into the hype; most of these “gut‑skin” claims are just marketing fluff for supplement sales.
Harshitha Uppada
October 14, 2025 AT 17:06idk why ppl keep writing these long essays when a simple diet change works.