Blood Pressure Decongestant Safety Checker
Is Your Decongestant Safe?
Check if your blood pressure medications interact with common decongestants. Many over-the-counter cold remedies contain ingredients that can dangerously raise your blood pressure when combined with certain heart medications.
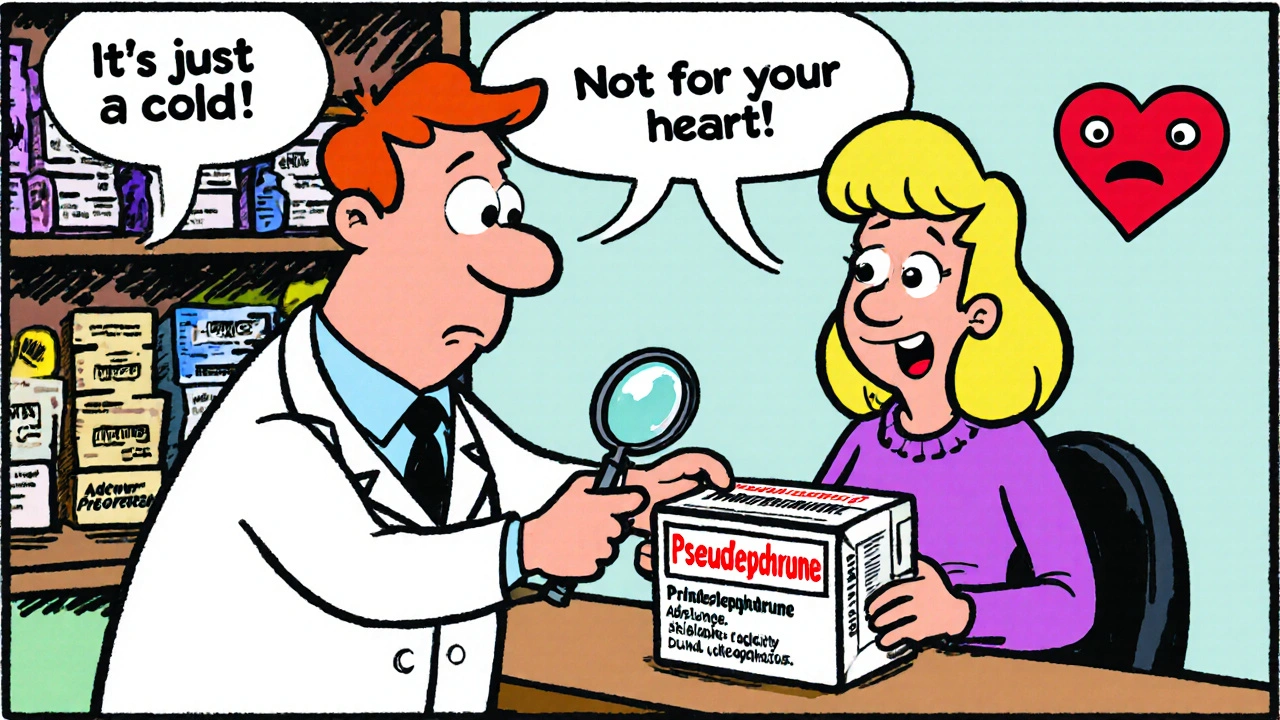
Many people reach for nasal decongestants when they have a stuffy nose. It’s quick, easy, and available over the counter. But if you’re taking medication for high blood pressure, that little bottle could be hiding a serious risk. You might think, It’s just a nasal spray or I’ve taken it before without issues. But the truth is, even short-term use of common decongestants can push your blood pressure into dangerous territory-especially when mixed with your regular heart meds.
How Decongestants Raise Blood Pressure
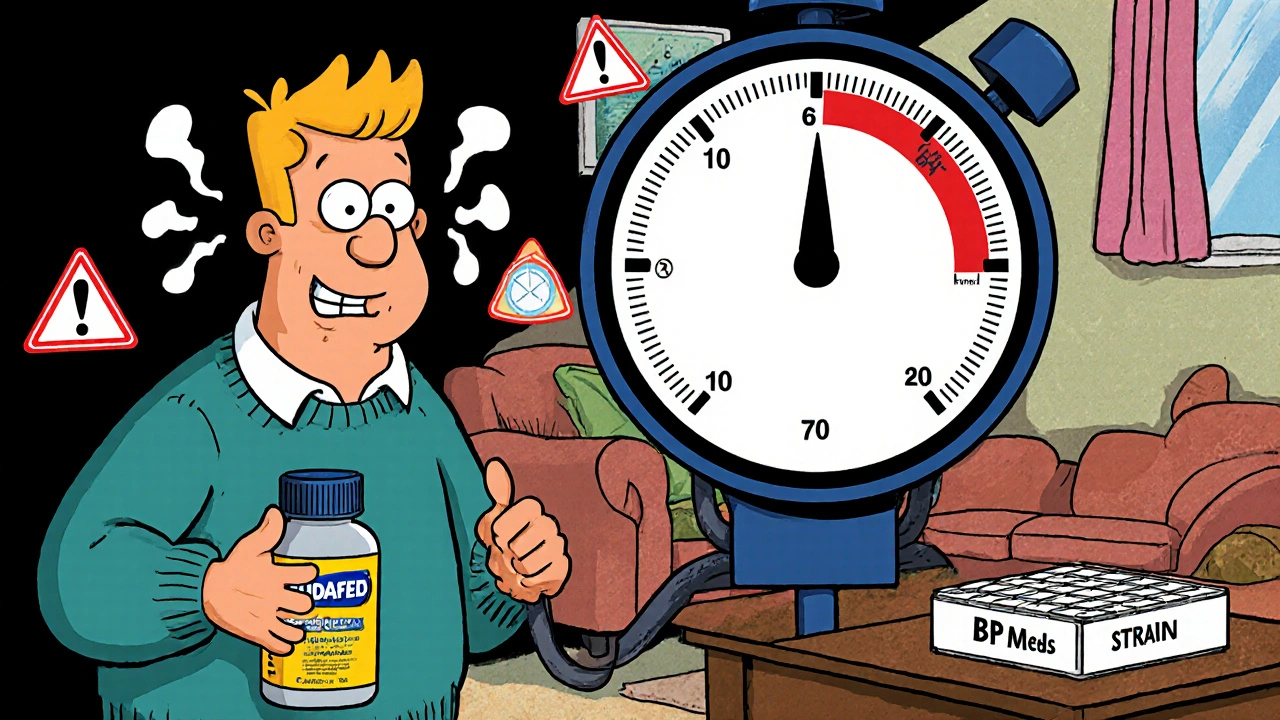
Nasal decongestants like pseudoephedrine (Sudafed), phenylephrine, and oxymetazoline (Afrin) work by tightening blood vessels in your nose. That reduces swelling and clears congestion. But here’s the catch: they don’t just target your nose. These ingredients enter your bloodstream and constrict blood vessels all over your body-including those around your heart and kidneys. This vasoconstriction forces your heart to work harder to pump blood through narrower arteries. The result? A spike in blood pressure. Even if your hypertension is well-controlled, a single dose of pseudoephedrine can raise systolic pressure by 5 to 10 mmHg. That might not sound like much, but for someone on blood pressure meds, it’s enough to undo weeks of careful management. A 2005 meta-analysis in the Journal of Clinical Hypertension confirmed this effect across hundreds of patients. The rise was small on average, but significant-and worse with higher doses or immediate-release forms. One documented case involved a 5-year-old child whose blood pressure climbed to 135/80 after just four days of phenylephrine use. It returned to normal only after stopping the medication.Which Blood Pressure Medications Are Most at Risk?
Not all blood pressure medications react the same way to decongestants, but many are affected. Here’s what you need to watch for:- Beta-blockers (like metoprolol or atenolol): Decongestants can counteract their ability to slow your heart rate, making them less effective.
- Calcium channel blockers (like felodipine or nifedipine): These can become less potent when combined with vasoconstrictors, leading to uncontrolled pressure.
- ACE inhibitors and ARBs: While less directly affected, the added stress on your cardiovascular system can still trigger spikes.
- Diuretics: Decongestants can reduce their effectiveness by altering fluid balance and increasing vascular resistance.
The Hidden Danger in Multi-Symptom Cold Meds
You’re not just at risk from standalone decongestants. The biggest threat comes from combination cold and flu products. Labels like “All-in-One Cold Relief” or “Nighttime Multi-Symptom” often hide decongestants under vague names or small print. Look for these active ingredients on the Drug Facts label:- Pseudoephedrine
- Phenylephrine
- Oxymetazoline
- Ephedrine
What to Do Instead: Safe Alternatives for Congestion
You don’t need to suffer through a stuffy nose. There are effective, safe ways to relieve congestion without risking your heart health.- Nasal saline spray: A simple saltwater rinse flushes out mucus and irritants without any chemical side effects. Use it several times a day-no risk, no interaction.
- Steam and humidity: Take a hot shower, use a humidifier, or inhale steam from a bowl of hot water. Moist air loosens mucus naturally.
- Antihistamines: If your congestion is allergy-related (runny nose, sneezing), antihistamines like loratadine or cetirizine can help. They don’t raise blood pressure and work by reducing inflammation, not constriction.
- Hydration and rest: Drinking plenty of fluids and getting enough sleep helps your body fight off colds faster. Often, time is the best medicine.
How to Use Medications Safely
If you absolutely must use a decongestant-say, your doctor says it’s okay under close supervision-follow these rules:- Check every label. Don’t assume “cold medicine” is safe. Read every active ingredient.
- Use the lowest dose for the shortest time. Never take it longer than 3 days without talking to your doctor.
- Monitor your blood pressure. Check it twice a day while using any decongestant. If it rises more than 10 mmHg above your usual baseline, stop immediately and call your provider.
- Ask your pharmacist. In the U.S., pseudoephedrine is kept behind the counter for a reason. Use that moment to ask: “Is this safe with my blood pressure meds?” Pharmacists are trained to catch these interactions.
- Keep a full medication list. Include every pill, spray, supplement, and herbal remedy. Bring it to every appointment.

Why This Matters More Than You Think
More than 75 million adults in the U.S. have high blood pressure. That’s nearly one in three people. And according to a 2024 study in the same journal, about 22% of emergency visits for uncontrolled hypertension in adults over 50 were linked to over-the-counter decongestants. It’s not just about one bad reaction. It’s about the quiet, repeated risk: someone taking Sudafed every time they get a cold, thinking it’s harmless. Over months or years, those small spikes add up. They strain your heart, damage your arteries, and increase your risk of stroke or heart attack. The American Heart Association updated its 2023 guidelines to stress that people with hypertension should avoid decongestants unless directed by a doctor. The FDA now requires all decongestant products to carry the warning: “Ask a doctor before use if you have high blood pressure.” That’s not just a legal formality-it’s a critical safety signal.What’s Next? The Future of Safe Congestion Relief
The medical community is taking notice. Several pharmaceutical companies are now in Phase 2 trials for new decongestants that don’t constrict blood vessels. These non-vasoconstrictive alternatives aim to clear congestion without affecting blood pressure at all. The American College of Cardiology plans to update its hypertension guidelines in 2026 to include clearer advice on OTC drug interactions. Until then, the safest approach remains: avoid decongestants unless your doctor says it’s okay.Frequently Asked Questions
Can I use a saline nasal spray if I have high blood pressure?
Yes, saline nasal sprays are completely safe for people with high blood pressure. They contain only salt and water and work by physically flushing out mucus and irritants. They don’t affect your blood pressure or interact with any medications. Use them as often as needed.
Is phenylephrine safer than pseudoephedrine for high blood pressure?
No, phenylephrine is not safer. While it’s often marketed as a replacement for pseudoephedrine, studies show it still raises blood pressure. In fact, some research suggests it may be less effective at relieving congestion while still carrying the same cardiovascular risks. Both should be avoided unless approved by your doctor.
Can I take decongestants if my blood pressure is controlled?
Even if your blood pressure is controlled, decongestants can still cause dangerous spikes. Medications like beta-blockers or calcium channel blockers may not fully protect you from the vasoconstrictive effects. The safest choice is to avoid them entirely. If you absolutely need relief, talk to your doctor first.
Do nasal decongestant sprays like Afrin enter the bloodstream?
Yes. Although applied locally, about 30% of oxymetazoline (the active ingredient in Afrin) can be absorbed into your bloodstream. That’s enough to raise your blood pressure, especially if used for more than 3 days. Topical doesn’t mean safe-especially if you have hypertension.
Are there decongestants that don’t raise blood pressure?
Currently, all standard decongestants-whether oral or nasal-work by constricting blood vessels and carry this risk. However, new non-vasoconstrictive alternatives are in clinical trials and may become available in the next few years. Until then, stick to saline, steam, and antihistamines.
Can decongestants interact with other medications besides blood pressure drugs?
Yes. Pseudoephedrine can dangerously interact with antidepressants (especially tricyclics), antibiotics like linezolid, and migraine medications containing ergot. These combinations can cause sudden, life-threatening spikes in blood pressure. Always tell your pharmacist or doctor about every medication you take.



Dave Wooldridge
November 20, 2025 AT 05:02They’re lying to us. Big Pharma doesn’t want you to know that saline sprays and steam work better-because they don’t make money off them. The FDA warning? A joke. They put it on the bottle so they can’t be sued, but they still sell the poison. I’ve seen people go into hypertensive crisis after taking Sudafed. And who’s to blame? The same corporations that sold cigarettes as ‘healthy.’ This is systemic murder disguised as OTC relief. Wake up.
They even hide it in ‘natural’ blends now. Look at the label. Look closer. That ‘herbal extract’? Probably phenylephrine in disguise. They’re engineering dependency. I’m not paranoid-I’m informed.
Rebecca Cosenza
November 21, 2025 AT 16:41Stop risking your life for a sniffle. 🙄
swatantra kumar
November 22, 2025 AT 19:07Bro, I live in Delhi and my nose is always stuffed from pollution. I used Afrin for 3 weeks straight last winter. My BP went from 120/80 to 160/95. My doctor nearly yelled at me. 😅
Now I use saline rinse + turmeric tea. Yeah, it’s slower. But I’m still alive to post this. Also, why do Americans think a pill fixes everything? We’ve been doing steam + jhinga masala for centuries. 🌿
Cinkoon Marketing
November 24, 2025 AT 06:42Actually, you’re kinda missing the point. The real issue isn’t the decongestants-it’s that doctors don’t educate patients. I work in pharma marketing and we get training on this stuff, but patients? They get a bottle and a smile. No one tells them to check the label. Even worse, pharmacies don’t always flag it. The system’s broken, not the meds.
Also, antihistamines aren’t always safe either-some cause drowsiness that makes people fall, especially elderly folks. It’s not black and white. Just… be careful. And read the tiny print. It’s there for a reason.
robert cardy solano
November 24, 2025 AT 16:24I used to take Sudafed every time I got a cold. Didn’t think twice. Then I started checking my BP at home. One dose and it jumped 15 points. Didn’t feel anything. No headache, no dizziness. Just… higher numbers.
Now I just breathe through my mouth and drink hot tea. Feels weird at first, but my BP’s been stable for a year. Weird how your body just… adapts if you give it a chance.
Pawan Jamwal
November 26, 2025 AT 07:40USA thinks it invented medicine. We in India know steam, salt, and patience. You think your pills are science? We had Ayurveda when your ancestors were still scratching fleas. This post is just another Western panic dressed up as education. Saline? We’ve been using it since the Vedic texts. 🙄
Also, why is everyone so scared of a little pressure spike? My uncle had BP 200/110 and still ran marathons. Maybe you’re weak.
Bill Camp
November 27, 2025 AT 22:29This is why America’s dying. People think a $5 bottle of Sudafed is harmless because it’s ‘over the counter.’ Like that means it’s safe. You wouldn’t let your kid play with a loaded gun because it’s ‘easy to get.’ But you’ll pop a decongestant like candy?
They don’t even put the warning in bold. It’s buried under ‘other ingredients.’ That’s not an accident. That’s corporate malice. And you’re all too lazy to read it.
Wake up. Your life isn’t a marketing campaign.
Lemmy Coco
November 28, 2025 AT 12:49just wanted to say i switched to saline spray after reading this and my nose feels way better and my bp is finally normal. i used to take those night time cold meds all the time. i didnt even know they had decongestants in them. my bad. thanks for the info. i think i’ll start keeping a med list like they said. 🤦♂️
rob lafata
November 29, 2025 AT 16:34Oh, so now we’re treating adults like toddlers who can’t read labels? Congrats, you’ve weaponized medical advice into a guilt trip. You know what’s more dangerous? People who don’t know their own bodies. I’ve been on beta-blockers for 12 years. I’ve taken pseudoephedrine 3 times. My BP spiked 8 points. I stopped. I didn’t need a 10-page lecture to figure that out.
What’s really toxic here isn’t the decongestant-it’s the condescension. You’re not saving lives. You’re just making people feel stupid for being sick. Grow up.
Matthew McCraney
December 1, 2025 AT 03:30they're watching us. every time you take a cold pill, they log it. your bp, your meds, your search history-everything. they're building a profile. why do you think the warning is so vague? so you don't realize how much they know. i stopped buying anything with 'phenyl' in it. now i use a neti pot and pray. the gov't doesn't want you to know how easy it is to kill you with a $4 bottle.
also, my cousin died after taking a cold med. they said 'natural ingredients.' turns out it had pseudoephedrine and a banned stimulant. they buried it. they always bury it.
serge jane
December 1, 2025 AT 16:48I think what’s really being asked here isn’t just about decongestants-it’s about how we treat our own bodies in a culture that treats health like a transaction. We’ve outsourced our intuition to labels and pills. We don’t listen to our bodies anymore. We just want the problem gone. Fast. Cheap. Easy.
But the body doesn’t work that way. It remembers. Every spike. Every strain. Every time we ignore a whisper and reach for the bottle instead of the steam. Maybe the real question is: are we trying to heal… or just escape?
I don’t have the answers. But I’m starting to wonder if the medicine we’re taking isn’t the problem. It’s the mindset.