Antifungal Self‑Care Guide
When talking about antifungal self-care, the practice of preventing and treating fungal skin infections using safe, effective methods. Also known as fungal skin health, it helps keep your skin clear and comfortable.
antifungal self-care starts with knowing what you’re dealing with. One common condition is tinea cruris, a fungal infection of the groin area, often called jock itch. It shows up as a red, itchy rash that spreads outward from the inner thigh. Spotting the early signs—tightness, burning, or a scaly border—lets you act before the fungus spreads to other warm, moist skin folds. Recognizing tinea cruris is a key step because the infection thrives in humidity, tight clothing, and sweaty workouts.
What You Need to Know About Antifungal Self‑Care
Effective griseofulvin, an oral antifungal that interferes with fungal cell division works well for deeper or recurring infections. Typical dosing runs 500 mg once daily for adults, but the exact amount depends on body weight and infection severity. Griseofulvin requires several weeks of consistent use because it builds up in keratin and only reaches the fungus as skin cells turn over. Side effects like headache or nausea are usually mild, yet you should avoid alcohol and stay hydrated while taking it.
For quicker, surface‑level relief many turn to clotrimazole, a topical azole that stops fungal growth on the skin. Apply a thin layer twice daily for two weeks, even if symptoms fade earlier—this prevents the fungus from bouncing back. If the rash is widespread or unresponsive to over‑the‑counter creams, combining a topical with an oral agent like griseofulvin often yields better results. This combination illustrates the semantic triple: antifungal self‑care requires both oral and topical treatments to fully eradicate the pathogen.
Prevention is the third pillar. Keep the affected area dry, change socks and underwear daily, and choose breathable fabrics. Shower right after exercising, and use an antifungal powder on feet and groin if you’re prone to sweat. These habits create an environment where fungi struggle to grow, aligning with the triple: proper skin hygiene reduces the risk of tinea cruris infections.
When you’re unsure whether an itch is fungal or bacterial, look for the characteristic ring‑shaped border and a clear line of demarcation. If the rash expands quickly, cracks, or produces pus, seek medical advice—sometimes a secondary bacterial infection needs antibiotics. Consulting a healthcare professional also ensures you get a prescription for griseofulvin or any stronger oral option when over‑the‑counter remedies fall short.
Overall, antifungal self‑care blends accurate identification, the right medication choice, and daily habits that keep moisture at bay. Below you’ll find curated articles that dive deeper into each of these topics, from dosage tips for griseofulvin to home‑care tricks for jock itch.
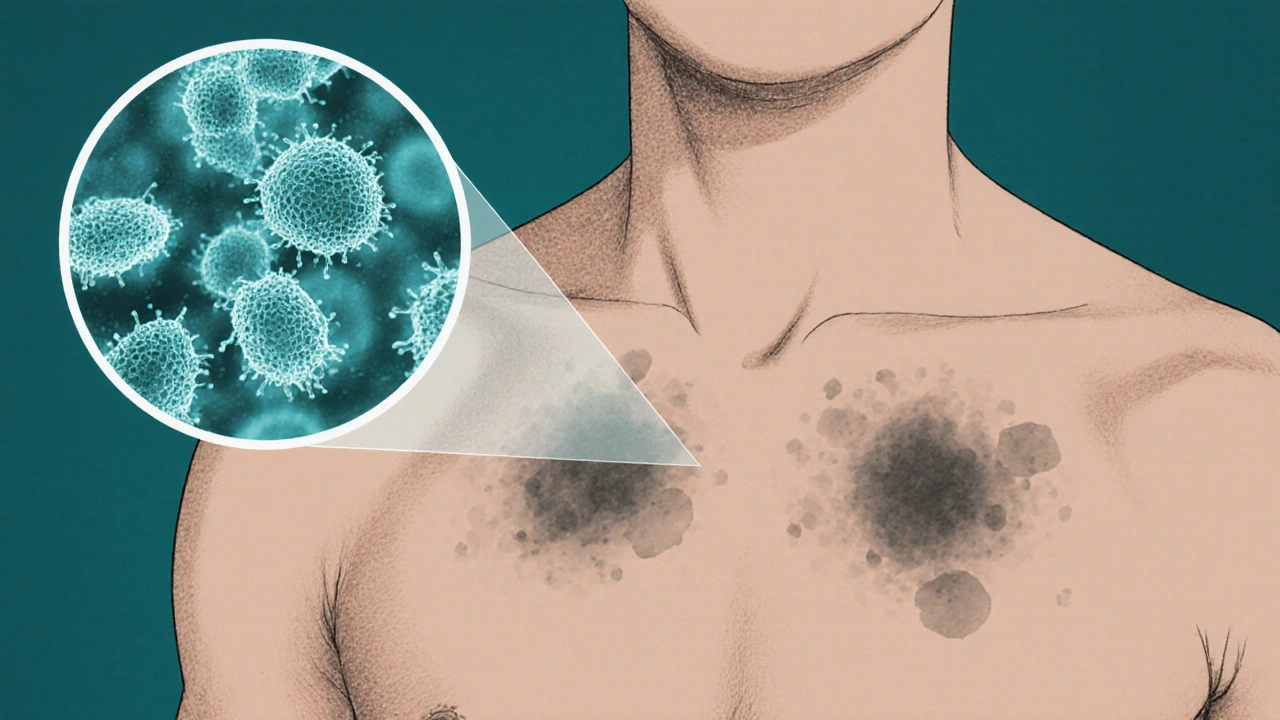
Self‑Care Tips for Managing Fungal Skin Discoloration
Learn how to blend medical treatment with self‑care habits-like gentle cleansing, sunscreen, probiotics, and stress management-to effectively treat and prevent fungal skin discoloration.