Proton pump inhibitors, or PPIs, are some of the most common pills people take for heartburn and acid reflux. You’ve probably seen ads for Prilosec, Nexium, or Prevacid. They work fast, they feel like magic when your chest is burning, and many people take them daily without thinking twice. But what happens when you take them for months-or years? The truth is, these drugs aren’t harmless. And if you’ve been on them longer than you should, you might be at risk for problems you never knew were connected to your medication.
What PPIs Actually Do
PPIs block the final step of acid production in your stomach. They target tiny pumps in the stomach lining called proton pumps-hence the name. When these pumps are shut down, less acid is made. That’s why they’re so effective for healing esophagitis, treating ulcers, and controlling GERD. Most people feel better within a few days. But here’s the catch: your stomach doesn’t stop making acid forever. It just takes a few days for the pumps to rebuild. That’s why you need to take PPIs before meals-they need to be active when the pumps turn on.
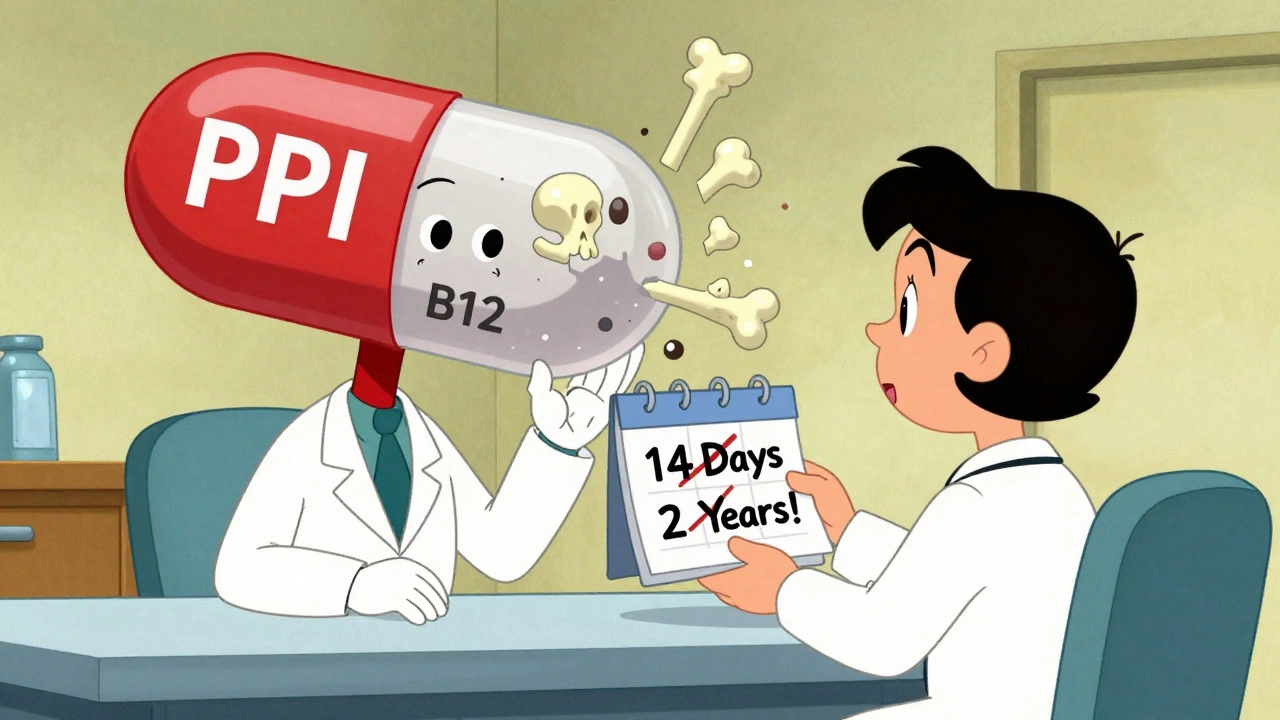
Common PPIs include omeprazole, esomeprazole, lansoprazole, pantoprazole, and rabeprazole. Prescription doses range from 10mg to 40mg. Over-the-counter versions are capped at 20mg, and the FDA says you shouldn’t use them for more than 14 days at a time, and no more than once every three months. Yet, studies show nearly one in four people keep taking them way past that.
The Hidden Risks of Long-Term Use
Just because a drug is widely used doesn’t mean it’s safe forever. The FDA has issued at least seven safety warnings about PPIs since 2010. Some risks are rare. Others are more common than you think.
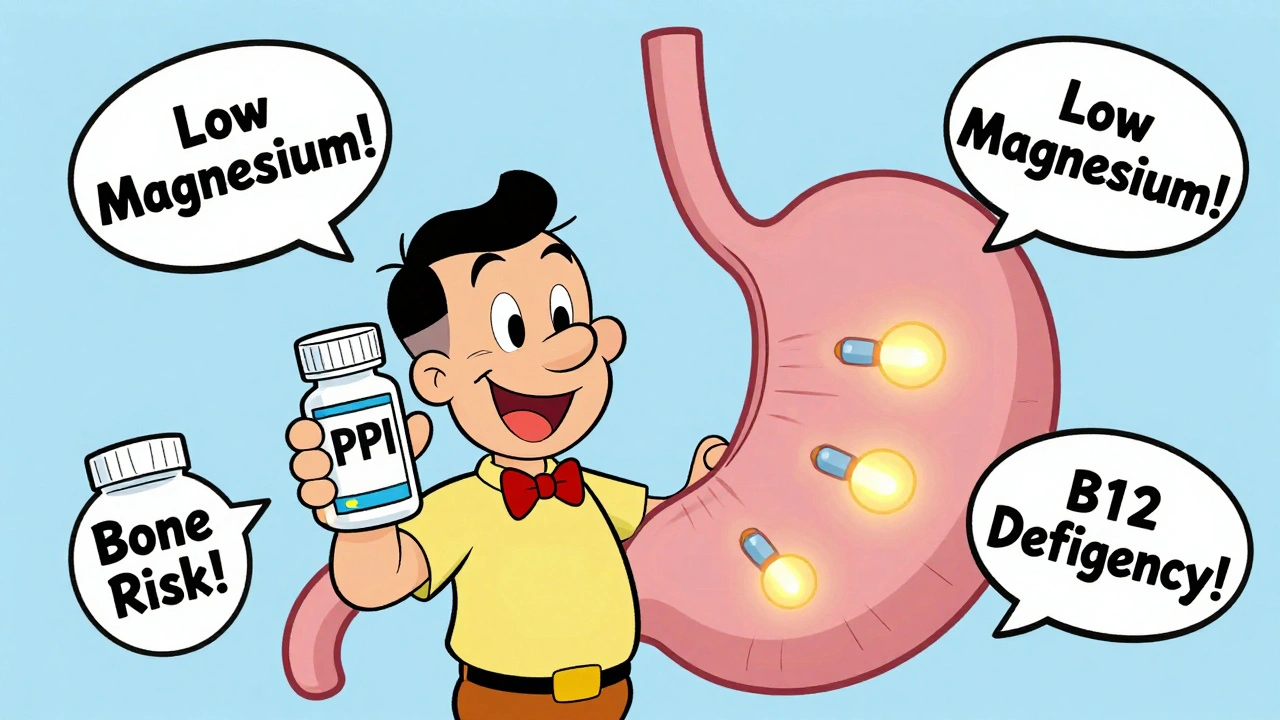
Low magnesium is one of the most serious. Long-term PPI use can lower your magnesium levels. You might not notice it at first. But when it gets bad, you can get muscle cramps, tremors, irregular heartbeat, or even seizures. The FDA now recommends checking magnesium levels if you’ve been on a PPI for over a year.
Broken bones are another real concern. People who take PPIs for more than four years have a 40% higher risk of hip fractures. Why? Acid helps your body absorb calcium. Less acid means less calcium gets into your bones. The good news? This risk goes down if you stop the medication. One study found that women who stopped PPIs more than two years ago had fracture risk back to normal.
Vitamin B12 deficiency affects up to 15% of long-term users. Your stomach needs acid to pull B12 out of food. No acid? Your body can’t absorb it. Symptoms include fatigue, numbness in hands and feet, memory issues, and even depression. It’s often mistaken for aging or stress. If you’ve been on PPIs for two years or more, ask your doctor to check your B12 levels.
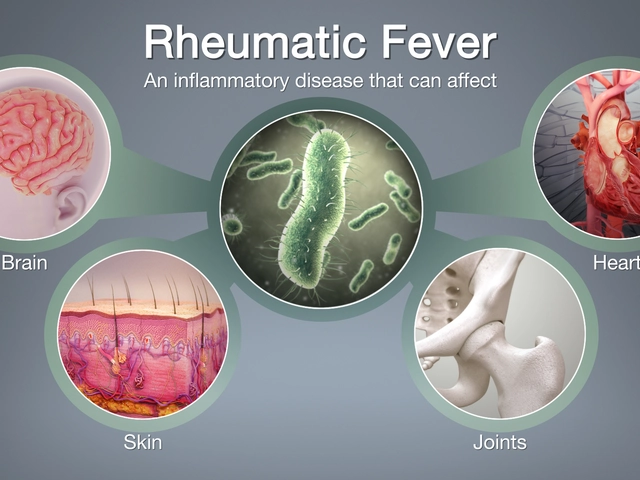
C. difficile infection is a dangerous gut bacteria that can cause severe diarrhea, especially in hospitals. PPIs raise your risk by about 1.7 to 2 times. Why? Acid normally kills harmful bacteria. When acid is suppressed, those bacteria can survive and take over.
There’s also acute interstitial nephritis-a rare but serious kidney inflammation. It can lead to permanent kidney damage if not caught early. And while some studies have linked PPIs to dementia, heart disease, or chronic kidney disease, the strongest evidence doesn’t support these claims. Many of those studies didn’t account for other health problems people taking PPIs often have-like obesity, diabetes, or smoking. So while the headlines are scary, the real risks are more specific.
When You Should Stop
You don’t need to be on a PPI forever. In fact, most people don’t need them long-term. The American College of Gastroenterology says PPIs should be used at the lowest dose for the shortest time possible. Here’s when you should consider stopping:
- You were prescribed a PPI for mild heartburn or dyspepsia without an endoscopy confirming disease.
- You’ve been on it for more than 8 weeks for uncomplicated GERD.
- You’re taking it for prevention of NSAID ulcers but no longer use NSAIDs.
- You’re on an over-the-counter PPI and have used it longer than 14 days without seeing a doctor.
Even if you have a confirmed diagnosis like erosive esophagitis, you should still try to stop every 6 to 12 months. This is called a “drug holiday.” Your doctor can help you test whether you still need it.
Stopping PPIs Isn’t Easy-Here’s How to Do It Right
Here’s the part no one tells you: if you stop PPIs cold turkey after months or years, you’ll likely get worse heartburn than before. That’s called rebound acid hypersecretion. Up to 80% of long-term users experience it. Your stomach overcompensates for the lack of acid and produces even more than normal.
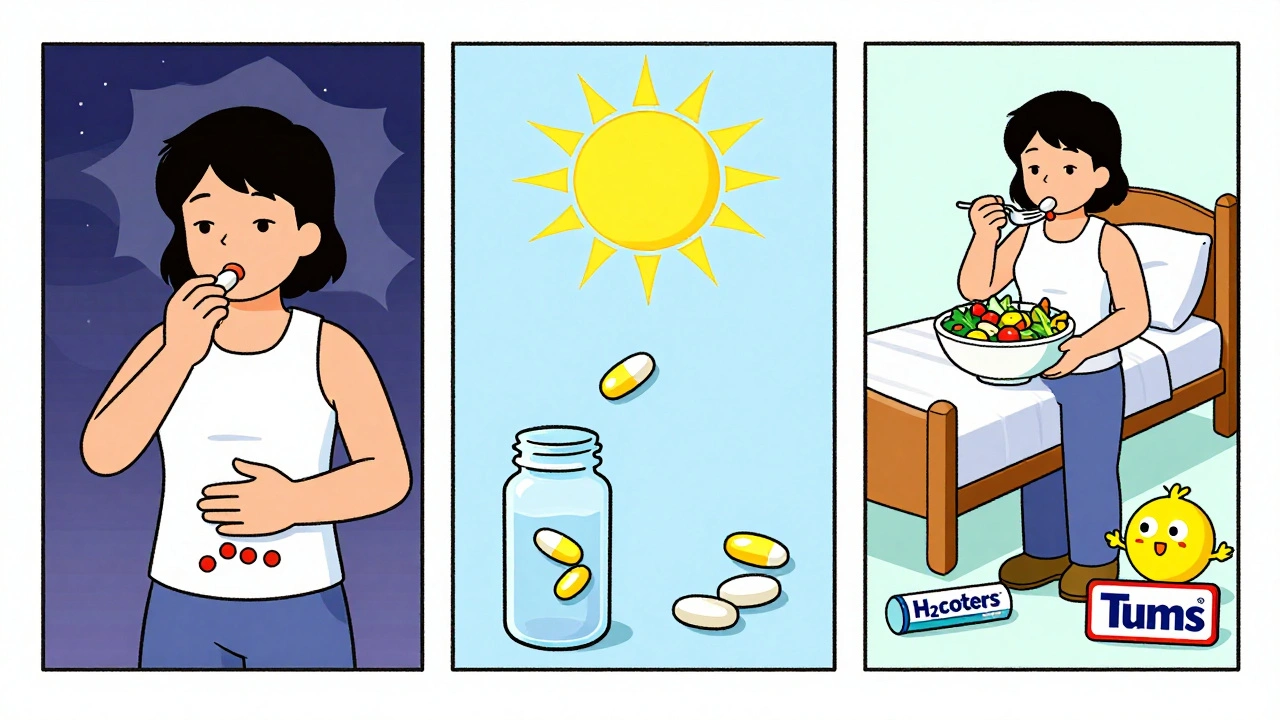
You can’t just quit. You need a plan:
- Reduce your dose by half for 1-2 weeks.
- Switch to taking it every other day.
- Then move to on-demand use-only when you feel symptoms.
- Use antacids like Tums or H2 blockers like famotidine (Pepcid) for breakthrough symptoms.
- After 4-6 weeks, try stopping completely.
Some people need to go slower. If you’ve been on a high dose for years, your doctor might recommend switching to a lower-dose PPI first, then tapering. Don’t rush it. Rebound symptoms can last 2-8 weeks. But they will fade.
What to Do Instead
If you’re stopping PPIs, you need alternatives. Lifestyle changes are the most powerful tool:
- Eat smaller meals. Don’t lie down for 3 hours after eating.
- Avoid trigger foods: spicy dishes, caffeine, chocolate, alcohol, citrus.
- Loosen tight clothing. Belly pressure pushes acid up.
- Elevate the head of your bed by 6-8 inches.
- Lose weight if you’re overweight. Even 10 pounds helps.
- Quit smoking. It weakens the valve that keeps acid down.
For occasional heartburn, try antacids (Tums, Rolaids) or H2 blockers (Pepcid, Zantac). They work fast and don’t suppress acid long-term. They’re perfect for on-demand use.
Why So Many People Take PPIs Too Long
It’s not just about ignorance. Doctors prescribe them too freely. Patients ask for them. Pharmacies sell them over the counter. Insurance covers them. And because they seem harmless, people keep taking them.
But here’s the cost: in the U.S. alone, inappropriate PPI use costs over $12 billion a year. And it’s not just money. It’s your health. One study found that 70% of people taking PPIs didn’t even have a clear medical reason to be on them. That’s not just overprescribing-it’s a systemic problem.
Many doctors don’t follow guidelines. The ACG says you shouldn’t give PPIs for dyspepsia without an endoscopy. But 40% of prescriptions are still for this vague symptom. And when patients say, “I feel better,” doctors don’t always ask, “How long have you been taking it?”
What’s Next?
New drugs called potassium-competitive acid blockers (P-CABs), like vonoprazan, are being studied. They work faster and may have fewer long-term side effects. But they’re not widely available yet, and we don’t have long-term safety data. For now, PPIs are still the gold standard for severe cases-like healing severe esophagitis. But for mild reflux? Lifestyle changes and H2 blockers are safer, cheaper, and just as effective.
The bottom line: PPIs are powerful tools. But they’re not meant to be lifelong. If you’ve been taking one for more than a few months, talk to your doctor. Don’t assume you need it. Don’t fear stopping. With the right plan, most people can get off PPIs without going back to daily heartburn.
Can I stop taking PPIs cold turkey?
No, stopping PPIs suddenly after long-term use often causes severe rebound acid reflux. Up to 80% of people experience worse symptoms. Always taper off gradually under medical supervision-reduce the dose slowly over weeks, then switch to on-demand use before stopping completely.
How long is too long to be on a PPI?
For most conditions like GERD or ulcers, 4 to 8 weeks is enough. If you still need it after that, your doctor should reassess. Long-term use-defined as more than 12 months-increases risks like low magnesium, bone fractures, and vitamin B12 deficiency. Regular reviews every 6 to 12 months are recommended.
Do PPIs cause kidney disease?
PPIs can cause acute interstitial nephritis-a rare but serious kidney inflammation. This usually happens within weeks to months of starting the drug. While some studies suggest a link to chronic kidney disease, higher-quality research hasn’t confirmed it. The risk is low, but if you notice swelling, fatigue, or changes in urination, get your kidney function checked.
Are over-the-counter PPIs safer than prescription ones?
No. OTC PPIs have the same active ingredients and risks as prescription versions. The FDA limits OTC use to 14 days every 3 months because long-term self-medication is dangerous. Many people ignore this label and take them daily for months, increasing their risk of side effects without medical oversight.
What are the best alternatives to PPIs for acid reflux?
For occasional heartburn, antacids like Tums or H2 blockers like famotidine (Pepcid) work well and don’t suppress acid long-term. For ongoing management, lifestyle changes are most effective: lose weight, avoid trigger foods, don’t eat before bed, and elevate your bed. These changes often eliminate the need for medication entirely.
Can PPIs cause dementia or Alzheimer’s?
Some early studies suggested a link, but later, better-designed research found no clear connection. The initial studies didn’t account for other health factors common in older adults taking PPIs, like diabetes or high blood pressure. Current evidence doesn’t support PPIs as a cause of dementia. Focus instead on proven risks like B12 deficiency and bone health.
Final Thoughts
PPIs saved lives and improved quality of life for millions. But they’re not candy. They’re powerful drugs with real, documented risks when used too long. If you’ve been on one for over a year, it’s time to talk to your doctor-not because you’re doing something wrong, but because you deserve to be on the least risky treatment possible. You don’t have to live with heartburn. You also don’t have to live with the hidden costs of long-term PPI use. With the right plan, you can get off them safely-and feel better than ever.




Carolyn Ford
December 5, 2025 AT 14:59Oh please. Another ‘PPIs are evil’ scare piece. I’ve been on omeprazole for 12 years, my esophagus is healed, and I’m not about to turn into a brittle-boned, B12-deficient zombie because some blog thinks I should ‘taper.’ I’ve had three bone density scans-perfect. My B12? Normal. My doctor monitors me. You’re not my doctor. Stop guilt-tripping people who actually need this.
Alex Piddington
December 5, 2025 AT 19:06Thank you for this comprehensive and evidence-based breakdown. It’s refreshing to see a post that doesn’t sensationalize but instead clarifies the nuanced risks and practical steps for discontinuation. The tapering protocol outlined is especially valuable-many patients aren’t warned about rebound acid hypersecretion, leading to unnecessary suffering and discontinuation failure. I’ve shared this with several patients already.
Libby Rees
December 6, 2025 AT 12:10This is exactly the kind of information that should be in every patient’s discharge summary. I work in a clinic and see so many people on PPIs for years without review. The fact that 70% have no clear indication is alarming. I always ask: ‘When was the last time you saw a gastroenterologist?’ Most can’t answer. Education is the first step to change.
George Graham
December 6, 2025 AT 20:19I was on PPIs for 5 years after being diagnosed with erosive esophagitis. I finally tapered off last year using the exact method described here-half dose, then every other day, then as needed. It was rough for about 6 weeks, but now I’m symptom-free. I lost 15 pounds, stopped eating late at night, and use Pepcid only when I eat too much pizza. I feel better than I have in a decade. It’s possible.
John Filby
December 8, 2025 AT 02:17Big thank you for this 🙏 I’ve been on Nexium since 2020 and never thought twice about it. Just read this and immediately booked a doctor’s appointment. Also, I had no idea OTC PPIs were just as risky. I thought ‘over-the-counter’ meant ‘safe for casual use.’ Whoops. Time to reevaluate everything.
Elizabeth Crutchfield
December 9, 2025 AT 21:48i just realized i’ve been taking prilosec every day for 3 years bc my mom said it was fine… i’m gonna try the taper thing. thanks for not making me feel dumb for not knowing this
Ben Choy
December 10, 2025 AT 05:46Love this. As a GP in the UK, I see this daily. Patients come in saying, ‘I feel better on it,’ but haven’t had a review in 5 years. We need better systems to flag long-term PPI use. Also, the lifestyle advice here? Gold. Simple, effective, and free. Why aren’t we prescribing that first?
Emmanuel Peter
December 11, 2025 AT 06:51Let’s be real-this is just Big Pharma’s way of keeping people hooked on meds. You’re ignoring the fact that PPIs are cheaper than surgery and way safer than letting acid eat your esophagus. Your ‘lifestyle changes’ are useless if you’re a 50-year-old with a desk job and three kids. Stop shaming people who need help just because you think they should ‘eat better.’
Ollie Newland
December 12, 2025 AT 02:51Rebound acid hypersecretion is the elephant in the room. Docs don’t explain it, patients panic, go back on PPIs, and the cycle repeats. The taper protocol here is spot-on. Also, H2 blockers are underrated-they’re not as potent but way less disruptive to gut microbiota. I use famotidine on-demand now after ditching my PPI. No more bloating, no more ‘acid rebound.’ Just… peace.