Most people think a bad cough means they need antibiotics. You’ve probably heard someone say, "I had bronchitis last year and the doctor gave me pills-it worked." But here’s the truth: antibiotics don’t help in most cases of acute bronchitis. Not because they’re weak, but because they’re the wrong tool for the job.
What Actually Causes Acute Bronchitis?
Acute bronchitis is an inflammation of the bronchial tubes-the airways that carry air into your lungs. It’s not pneumonia. It’s not the flu. It’s usually a virus, and it’s incredibly common. About 5% of adults get it every year in the U.S., and it’s one of the top 10 reasons people visit their doctor. In Australia, where I live in Brisbane, we see it every winter-especially after colds and flu season. The virus attacks the lining of your airways. Your body responds by making extra mucus and triggering a cough to clear it out. That cough? It’s not a sign of infection spreading. It’s your body doing its job. The most common culprits? Rhinovirus (the same one that gives you a cold), coronavirus, influenza, and respiratory syncytial virus (RSV). These aren’t bacteria. Antibiotics kill bacteria. They don’t touch viruses. And here’s the kicker: 90 to 95% of acute bronchitis cases are viral. That means antibiotics are useless in nearly every case.How Long Does the Cough Last?
This is where people get frustrated. You expect to feel better in a few days. But with bronchitis, the cough sticks around. Studies show the average cough lasts about 18 days. Half of people are still coughing at 10 days. A quarter are still coughing at two weeks. And 1 in 10 are coughing at three weeks. That’s not unusual. That’s normal. If your cough lasts longer than three weeks, then you should see a doctor. But if it’s been 12 days and you’re still hacking? You’re probably right on schedule. The virus is long gone. Your airways are just slow to heal.Why Antibiotics Don’t Work-And Why They Hurt
You might be thinking: "But what if it turns into pneumonia?" That’s a fair concern. But here’s what the data says: A major review of 9 studies with over 5,600 patients found that antibiotics reduce cough duration by just 0.6 days. That’s less than half a day. You’d need to give antibiotics to 39 healthy adults to prevent one case of pneumonia. Meanwhile, for every 14 people who take antibiotics, one will have an adverse reaction-diarrhea, nausea, rash, or worse. And that’s just the immediate cost. The bigger problem is antibiotic resistance. Every time you take an antibiotic when you don’t need it, you help bacteria learn how to survive them. The CDC estimates that 46 million unnecessary antibiotic prescriptions are given for respiratory infections like bronchitis every year in the U.S. That’s contributing to 2.8 million resistant infections and 35,000 deaths annually. Doctors know this. The American Academy of Family Physicians, the American College of Chest Physicians, and the CDC all agree: do not prescribe antibiotics for uncomplicated acute bronchitis. Yet, in 2022, over half of bronchitis patients still got antibiotics. Why? Because patients ask for them. Because doctors feel pressured. Because it’s easier to write a prescription than to explain why it won’t help.What Actually Helps? Evidence-Based Cough Care
So if antibiotics don’t work, what does? Rest and fluids. This isn’t just old advice. Your body needs energy to heal. Drinking water helps thin mucus so it’s easier to clear. Aim for 8-10 glasses a day. Warm tea, broth, or even just plain water-any of it helps. Humidifiers and steam. Dry air makes coughing worse. A cool-mist humidifier in your bedroom helps. So does breathing steam from a bowl of hot water (be careful-not to burn yourself). Just sitting in a steamy bathroom for 10 minutes can soothe irritated airways. Pain and fever relief. If you’ve got a low-grade fever or chest discomfort, use ibuprofen (Advil) or acetaminophen (Tylenol). Follow the label. Don’t exceed 3,000 mg of acetaminophen per day, especially if you drink alcohol or have liver issues. Honey. Yes, honey. A 2018 study in JAMA Pediatrics found honey worked as well as, or better than, over-the-counter cough medicines for kids. For adults, 1 to 2 tablespoons before bed can quiet a nighttime cough. But never give honey to children under 1 year old. It can cause infant botulism-a rare but serious condition. Dextromethorphan. This is the active ingredient in many cough syrups. It doesn’t cure anything, but it can reduce cough frequency. Studies show a modest benefit. Take 15-30 mg every 6-8 hours, no more than 120 mg in 24 hours. Avoid if you’re on antidepressants or have high blood pressure. Don’t use guaifenesin (Mucinex) unless you’re sure it helps you. Some people swear by it. But studies are mixed. Only 2 out of 7 trials showed real benefit. If it doesn’t help after a few days, stop. Don’t use inhaled inhalers (like albuterol) unless you’re wheezing. If your bronchitis comes with wheezing or tightness in your chest, a doctor might prescribe one. But if you’re just coughing? It won’t help-and it might give you a racing heart or shaky hands.What About Natural Remedies and Supplements?
There’s a lot of hype around elderberry, echinacea, and vitamin C. But here’s the reality: no supplement has proven benefit for acute bronchitis. The NIH is currently studying ivy leaf extract in a trial called BREATHE. Early results look promising for reducing cough, but we won’t know for sure until late 2024. Until then, stick with what’s been tested: honey, hydration, rest, and over-the-counter cough suppressants.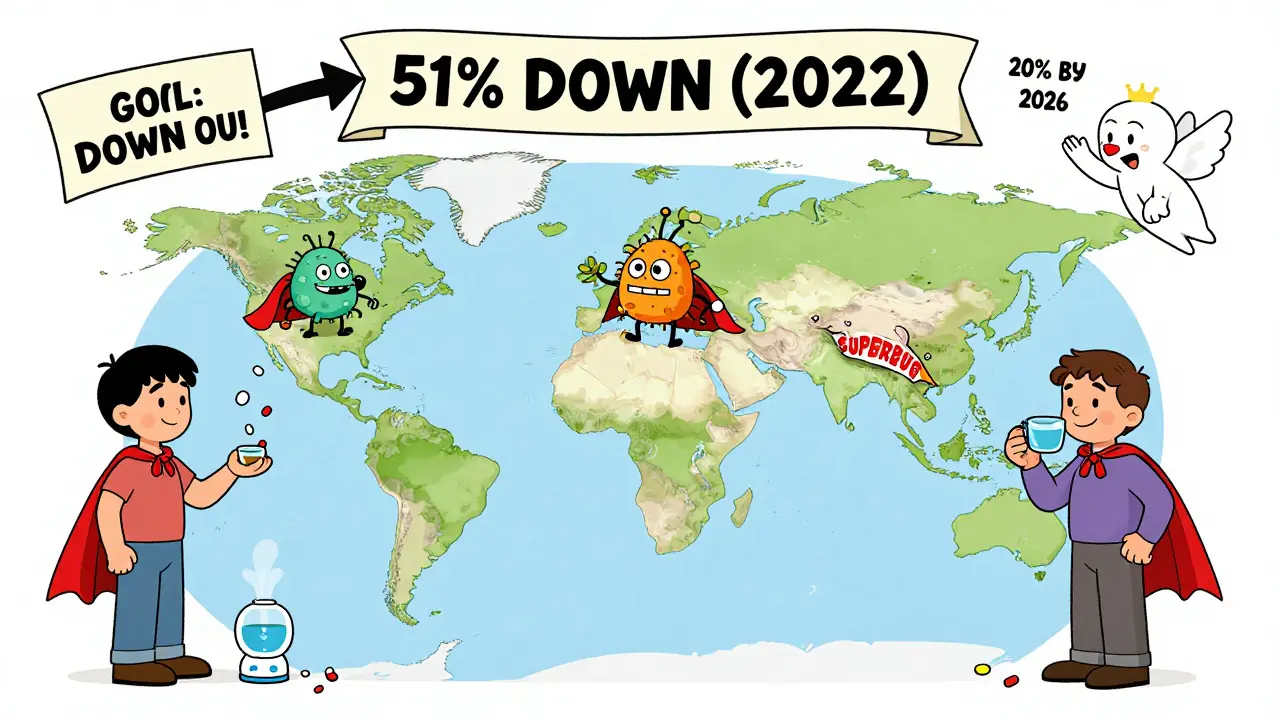
When Should You See a Doctor?
Most of the time, you don’t need to. But there are red flags:- Fever over 38.5°C (101.3°F) that lasts more than a few days
- Coughing up blood or thick, discolored mucus (yellow/green isn’t always a sign of infection-it can just be old mucus)
- Shortness of breath or wheezing that gets worse
- Cough lasting more than 3 weeks
- Weight loss, night sweats, or extreme fatigue
Why This Matters Beyond Your Own Cough
Choosing not to take antibiotics isn’t just about you. It’s about everyone else too. Every unnecessary antibiotic you take adds to the global crisis of superbugs. These are bacteria that no drug can kill. We’re already seeing infections that once were easily treated-like urinary tract infections or skin abscesses-becoming life-threatening because antibiotics no longer work. The Choosing Wisely campaign, backed by medical societies across the U.S. and Australia, lists "Don’t prescribe antibiotics for acute bronchitis" as one of the top 5 recommendations for doctors. And it’s working-slowly. Antibiotic prescribing for bronchitis dropped from 74% in 2010 to 51% in 2022. But we still have a long way to go. The goal? Get that number below 20% by 2026. That’s the target set by the American Academy of Family Physicians. And it’s possible-if patients understand the science and stop asking for pills that won’t help.Final Advice: Be Patient, Be Smart
Acute bronchitis is annoying. It steals your sleep. It makes you feel weak. It makes you feel like something’s seriously wrong. But it’s not. It’s your body fighting off a virus. And it will win. Don’t rush to the pharmacy for antibiotics. Don’t pressure your doctor. Instead, rest. Drink water. Try honey. Use a humidifier. Give your body time. And if someone tells you antibiotics fixed their bronchitis? They probably had a bacterial infection-like pneumonia-or their cough was from something else entirely. Your cough isn’t broken. It’s just slow. And that’s okay.Are antibiotics ever needed for acute bronchitis?
Almost never. Only about 5-10% of cases are bacterial, and even then, it’s usually in people with other health problems like COPD or weakened immunity. For healthy adults, antibiotics provide no meaningful benefit and carry real risks. The guidelines from the CDC, AAFP, and ACCP all say: avoid them unless there’s clear evidence of a bacterial complication.
How long should I wait before seeing a doctor for a cough?
Wait until your cough lasts more than three weeks. Most people recover within 18 days. If you’re still coughing hard after 21 days, or if you develop new symptoms like fever, shortness of breath, or chest pain, it’s time to get checked. Don’t rush in after 5 days-your body just needs more time.
Is green or yellow mucus a sign I need antibiotics?
No. Mucus color changes as your immune system fights the virus. Thick, yellow, or green mucus doesn’t mean bacteria are present. It’s just dead immune cells and mucus. Studies show mucus color doesn’t predict whether antibiotics will help. Don’t use color as a guide-use symptoms like fever, breathing trouble, or cough lasting over three weeks.
Can I give honey to my child for cough?
Yes-for children over 1 year old. Honey is safer and often more effective than over-the-counter cough syrups. Give 2.5-10 mL (half to two teaspoons) as needed, especially before bed. Never give honey to babies under 12 months. It can cause infant botulism, a rare but dangerous illness.
Why do doctors still prescribe antibiotics for bronchitis if they don’t work?
Pressure. Patients expect them. Some doctors feel rushed and think it’s easier to write a script than to explain why it won’t help. Some fear losing patients if they don’t prescribe. But studies show that when doctors take 2-3 extra minutes to explain the natural course of bronchitis, antibiotic requests drop by 32%. It’s not laziness-it’s a communication gap that’s slowly closing.
What’s the best way to prevent acute bronchitis?
Wash your hands often, avoid close contact with sick people, and get your annual flu shot. Since bronchitis often follows a cold or flu, preventing those reduces your risk. Avoid smoking and secondhand smoke-irritants make your airways more vulnerable. There’s no vaccine for bronchitis itself, but protecting against its triggers helps.







Lily Steele
February 1, 2026 AT 11:12Just wanted to say thanks for this. I had bronchitis last winter and took antibiotics because I thought I had to. Turns out I just needed rest and honey. My cough lasted 17 days-felt like forever, but now I know it was normal.
Claire Wiltshire
February 1, 2026 AT 23:30Thank you for writing this with such clarity and evidence. It’s frustrating how often patients (and even some providers) equate mucus color with bacterial infection. The data is clear: color is not a reliable indicator. Educating the public on the natural course of viral illnesses is one of the most important public health tasks we have right now.
Amy Insalaco
February 2, 2026 AT 10:39Let’s be honest-this entire post is a beautifully crafted piece of medical propaganda designed to pacify the masses while preserving the pharmaceutical-industrial complex’s profit margins. The notion that antibiotics are ‘useless’ in bronchitis ignores the subtle immunomodulatory effects of macrolides, which have been shown in multiple double-blind RCTs to reduce cytokine-mediated airway hyperreactivity independent of their antimicrobial activity. And don’t get me started on the epistemological arrogance of dismissing anecdotal evidence as ‘confirmation bias’-human experience is data too, even if it doesn’t fit your p-value.
Also, honey? Really? That’s your evidence-based intervention? Next you’ll be recommending crystal healing for pneumonia.
Rohit Kumar
February 3, 2026 AT 10:06In India, we’ve always known this. Grandmas don’t give antibiotics for cough-they give ginger tea, steam with tulsi leaves, and patience. Modern medicine sometimes forgets what traditional systems knew instinctively: the body heals itself if you don’t interfere with the wrong tools.
Also, the antibiotic resistance crisis here is already catastrophic. We’re seeing untreatable UTIs and skin infections in young people. This post should be mandatory reading in every clinic.
Kathleen Riley
February 3, 2026 AT 11:42It is an incontrovertible fact, grounded in empirical epidemiological analysis, that the systemic overprescription of antimicrobial agents for viral etiologies constitutes a profound epistemic failure within contemporary primary care paradigms. The conflation of symptomatology with pathogenetic causality-particularly the erroneous attribution of mucopurulent discharge to bacterial superinfection-reflects a persistent diagnostic heuristic rooted in cognitive bias rather than evidence-based reasoning.
Furthermore, the sociological dimension of patient expectation, reinforced by commodified healthcare models, creates a feedback loop wherein therapeutic nihilism is institutionalized under the guise of patient satisfaction.
Jodi Olson
February 3, 2026 AT 20:08My doctor actually took 5 minutes to explain this to me last year. I was shocked. No one ever talks about how long the cough lasts. I thought I was dying at day 10. Now I just drink tea and wait. It’s weird how simple it is when you stop listening to commercials.
Carolyn Whitehead
February 4, 2026 AT 12:43So true about the honey. I use it every time I get a cold now. No more cough syrup for me. Also, humidifier = game changer. I didn’t know steam could help so much. Just sitting in the bathroom with the hot water running feels like a spa day for my lungs lol
April Allen
February 4, 2026 AT 18:34The real tragedy isn’t the overprescription of antibiotics-it’s the epistemological collapse of public trust in biological complexity. We’ve reduced the human organism to a machine that requires a switch-flip fix, when in reality, healing is a nonlinear, emergent process governed by homeostatic feedback loops, circadian rhythms, and immune memory. Antibiotics are a blunt instrument in a world that needs precision. The cough isn’t a bug to be eradicated-it’s a signal, a symphony of clearance, a testament to the body’s capacity to self-regulate when not interrupted by pharmacological overreach.
We’ve forgotten that illness is not an enemy to be defeated, but a teacher. And we’re failing the lesson.
Yanaton Whittaker
February 6, 2026 AT 18:10LOL at the honey thing. Next they’ll say we should pray for pneumonia. 🤡 I’ve had bronchitis 3 times. Antibiotics fixed it every time. You people are just scared of real medicine. #AmericaFirst #AntibioticsWork
Blair Kelly
February 8, 2026 AT 07:55Look, I don’t care what the CDC says. I’ve seen people die because they didn’t get antibiotics fast enough. You think I’m gonna sit around for 18 days coughing up my lungs while some academic tells me to drink tea? No. I’m not a lab rat. I’m a human being who wants to feel better. And if a pill helps-even if it’s just placebo-I’ll take it. You want to save the world? Start by saving me.
Katie and Nathan Milburn
February 8, 2026 AT 12:13Thank you for this. We shared it with our parents, who still believe green mucus = antibiotics. It helped them understand why their doctor refused the prescription. It’s hard to change minds, but facts like these make it possible.