When you’re trying to get pregnant and your body won’t ovulate regularly, it’s not just frustrating-it’s exhausting. For women with PCOS, this isn’t just about irregular periods. It’s about hormones out of balance, insulin running wild, and a system that seems designed to keep conception out of reach. That’s where metformin comes in-not as a magic pill, but as a quiet, powerful tool that helps reset the body’s metabolic foundation.
Why PCOS Makes Ovulation So Hard
Polycystic Ovary Syndrome affects 6 to 12% of women of reproductive age. It’s not just about cysts on the ovaries. The real problem lies in insulin resistance. Your body makes more insulin than it needs, not because you eat too much sugar, but because your cells don’t respond properly to it. That extra insulin tells your ovaries to pump out more testosterone. High testosterone? That shuts down ovulation. It also causes acne, unwanted hair growth, and weight gain-symptoms that make women feel like their bodies are working against them.How Metformin Works in PCOS
Metformin doesn’t lower blood sugar by forcing insulin out. It doesn’t trick your body. It fixes the problem at the source: insulin resistance. It reduces glucose production in the liver, slows down sugar absorption in the gut, and helps muscle cells take up glucose more efficiently. The result? Lower insulin levels. And when insulin drops, so does testosterone. That’s the key.Studies show that within 3 to 6 months of consistent use, many women with PCOS start ovulating again. In one analysis of 44 trials, women taking metformin were over 2.5 times more likely to ovulate than those on placebo. That’s not a small effect. It’s life-changing for someone who hasn’t had a period in months.
Metformin vs. Other Fertility Drugs
For years, clomiphene citrate was the go-to drug for PCOS infertility. It works by tricking the brain into releasing more FSH and LH-hormones that trigger ovulation. But it doesn’t fix insulin resistance. And for many women, it doesn’t work at all.Then came letrozole. A 2023 study found that 88.9% of women ovulated when they took letrozole plus metformin. With metformin alone? Only 69.4%. That gap tells you something: metformin doesn’t replace other drugs. It makes them better.
When clomiphene fails, adding metformin often turns the tide. One study showed that women who took metformin for 3 months before starting clomiphene had significantly higher pregnancy rates than those who started clomiphene right away. Metformin doesn’t just help you ovulate-it helps your body respond to other treatments.
Who Benefits Most From Metformin?
Not every woman with PCOS responds the same way. The biggest gains come from those with clear insulin resistance-even if they’re not overweight. A 2023 review in Annals of Translational Medicine found that non-obese women with high insulin levels had ovulation rates nearly equal to those on clomiphene, but with fewer side effects and better long-term metabolic protection.That’s a big shift. For years, guidelines said only obese women should get metformin. Now, evidence says: if your insulin is high, your body needs it-regardless of weight.

Metformin and Pregnancy: Safe to Keep Taking?
Many women stop metformin as soon as they get a positive pregnancy test. But here’s what the data shows: continuing metformin through the first trimester is linked to higher clinical pregnancy rates and lower miscarriage risk in women with PCOS. A 2023 meta-analysis of 12 trials found that women who kept taking it had better outcomes than those who stopped.Metformin is classified as Category B in pregnancy-meaning no harm was seen in animal studies, and human data shows no increased risk of birth defects. Many OB-GYNs now recommend continuing it until 12 weeks, especially if insulin resistance was a major factor in infertility.
Reducing OHSS Risk During IVF
If you’re going through IVF with PCOS, you’re at higher risk for ovarian hyperstimulation syndrome (OHSS)-a dangerous condition caused by over-response to fertility drugs. Metformin cuts that risk by more than 70%. One pooled analysis found an odds ratio of 0.27-meaning women on metformin were far less likely to develop OHSS. That’s not a side benefit. It’s a safety net.Dosing and Side Effects: What to Expect
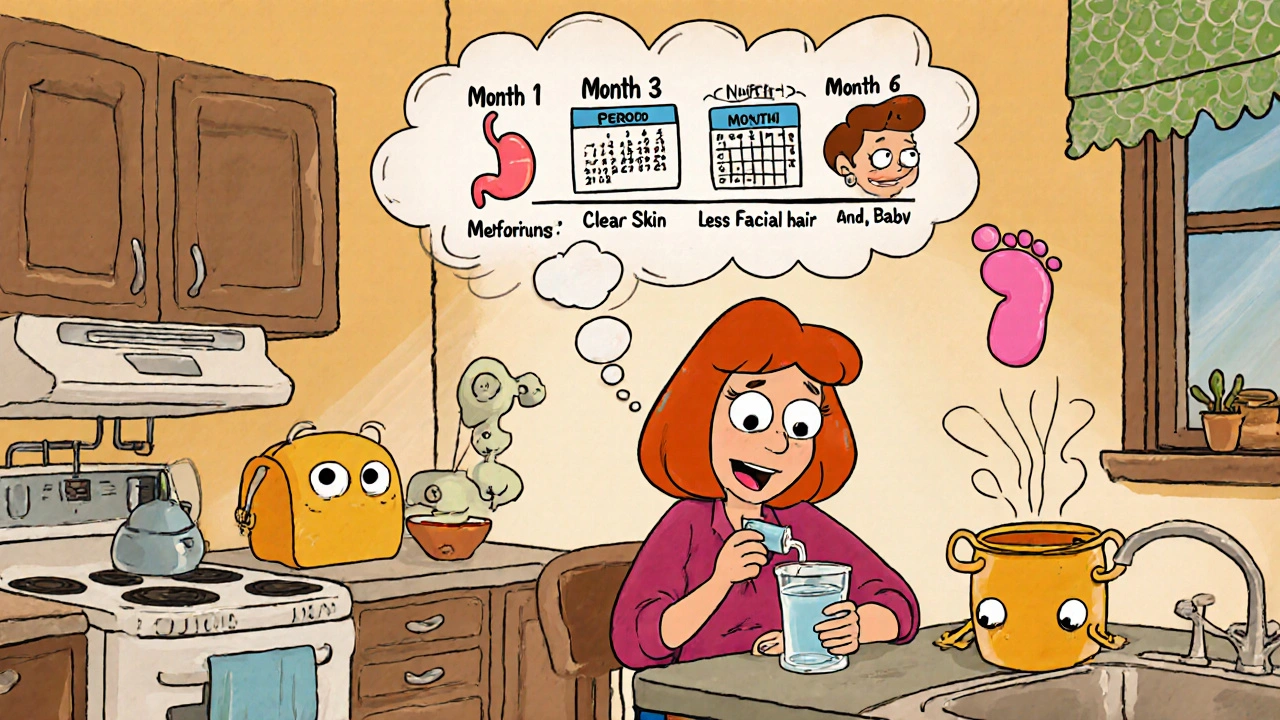
Most doctors start with 500mg once a day with dinner. After a week or two, they bump it to 500mg twice a day. The goal is usually 1,500 to 2,000mg daily. Extended-release (XR) versions like Glucophage XR are easier on the stomach-fewer nausea episodes, less diarrhea. About 20-30% of people get GI side effects at first, but most of them fade within 2 to 4 weeks.Don’t give up after a week. Stick with it. Many women report their periods returning to normal around the 3-month mark. Some notice less facial hair and clearer skin within 6 months. These aren’t instant fixes. They’re slow, steady improvements.
Cost and Accessibility
Metformin is cheap. Generic versions cost $4 to $10 a month in the U.S. Compare that to letrozole ($50-$100) or clomiphene ($30-$50). It’s one of the most cost-effective treatments in reproductive medicine. And because it’s been around since the 1950s, it’s widely available, even in low-resource settings.Long-Term Benefits Beyond Fertility
Metformin doesn’t just help you get pregnant. It helps you stay healthy. Women with PCOS have a higher risk of type 2 diabetes, heart disease, and endometrial cancer. Metformin reduces insulin spikes, lowers LDL cholesterol, and helps with weight management. The REPOSE trial showed it could delay or even prevent diabetes in high-risk women. That’s not just about fertility. It’s about decades of health.What the Evidence Still Doesn’t Clear Up
There’s still debate. Some studies show metformin alone doesn’t improve live birth rates much compared to placebo. Others show clear gains. Why the difference? Because PCOS isn’t one condition. It’s a mix of metabolic, hormonal, and genetic factors. For some women, metformin is the missing piece. For others, it’s just one part of a bigger puzzle.What’s clear: metformin works best when it’s part of a plan-not the whole plan. Used with lifestyle changes, letrozole, or timed intercourse, it becomes a powerful tool. Used alone, it’s still helpful-but not always enough.
Practical Tips for Starting Metformin
- Start low: 500mg once daily with your evening meal.
- Use extended-release if GI side effects hit hard.
- Take it consistently-even on days you don’t feel like it.
- Track your cycles with ovulation tests or basal body temperature.
- Get a progesterone test 7 days after you think you ovulated to confirm it happened.
- Don’t stop if you feel worse at first. Give it 4-6 weeks.
- Ask your doctor about continuing through early pregnancy if you conceive.
Metformin isn’t a cure for PCOS. But for many women, it’s the first step back to control-over their cycles, their hormones, and their future.
Can metformin help me ovulate if I have PCOS?
Yes. Metformin improves ovulation rates in women with PCOS by reducing insulin resistance, which lowers testosterone levels and helps restore normal ovarian function. Studies show women on metformin are over 2.5 times more likely to ovulate than those on placebo. Results typically appear after 3-6 months of consistent use.
Is metformin better than clomiphene for PCOS infertility?
Not always alone-but often better in combination. Clomiphene works better than metformin alone for triggering ovulation. But when metformin is added to clomiphene, pregnancy rates rise significantly. For non-obese women with insulin resistance, metformin may be just as effective as clomiphene, with fewer side effects and long-term metabolic benefits.
Does metformin cause weight loss in PCOS?
Some women lose 2-5% of their body weight on metformin, especially when combined with diet and exercise. It doesn’t directly burn fat, but by improving insulin sensitivity, it reduces fat storage and cravings. Weight loss is more likely in those with higher insulin resistance.
How long should I take metformin before trying to conceive?
Most doctors recommend at least 3 months of consistent use before actively trying to conceive. This gives your body time to lower insulin, restore ovulation, and improve egg quality. Some women benefit from 6 months or longer, especially if insulin resistance is severe.
Can I take metformin while pregnant?
Yes, and many doctors recommend continuing it through the first trimester if you have PCOS and insulin resistance. Studies show higher pregnancy rates and lower miscarriage risk when metformin is continued early in pregnancy. It’s classified as Category B-no evidence of harm to the fetus in human studies.
What are the most common side effects of metformin?
Nausea, diarrhea, bloating, and stomach upset are common at first, affecting 20-30% of users. These usually improve after 2-4 weeks. Switching to extended-release (XR) tablets reduces side effects significantly. Taking it with food also helps.
Does metformin help with acne and facial hair in PCOS?
Yes. By lowering insulin and testosterone levels, metformin can reduce hirsutism and improve acne over time. It’s often used as an alternative to birth control pills for women who can’t or won’t take them. Results take 3-6 months to become noticeable.
Is metformin safe for long-term use?
Yes. Metformin has been used safely for over 60 years. Long-term use is linked to reduced risk of type 2 diabetes, heart disease, and endometrial cancer in women with PCOS. Regular monitoring of kidney function and B12 levels is advised, but serious side effects are rare.







LINDA PUSPITASARI
November 29, 2025 AT 19:01Just started metformin 3 weeks ago and my cravings for sugar are GONE 😭 I thought I’d die without cookies but now I’m actually excited about veggies 🥬😂
gerardo beaudoin
December 1, 2025 AT 05:38Metformin isn't magic but it's the best tool we've got for PCOS. I took it for 4 months before trying to conceive and my cycles went from every 60 days to every 28. No drama, just science.
Brandy Johnson
December 1, 2025 AT 11:13While the data may suggest marginal benefits, the pharmaceutical industry's promotion of metformin as a fertility panacea is a textbook case of off-label exploitation. One must question the long-term metabolic consequences of chemically altering insulin signaling in otherwise healthy women.
Monica Lindsey
December 1, 2025 AT 21:55You're all just taking metformin because it's cheap. Meanwhile, real women are doing IVF with donor eggs and actually getting results. This is the bare minimum of effort.
linda wood
December 2, 2025 AT 10:09So you're telling me the same drug that helps diabetics live longer also helps women with PCOS actually get pregnant? And people still think this is 'just a weight loss pill'? 😅
Steven Howell
December 3, 2025 AT 18:25In many non-Western healthcare systems, metformin remains the first-line intervention for PCOS due to its cost-effectiveness and low adverse event profile. The Western obsession with pharmaceutical alternatives often overlooks the global utility of this agent.
Robert Bashaw
December 5, 2025 AT 01:16I took metformin and suddenly my skin cleared up like I'd been baptized by an angel who hates acne. I cried. Not because I was happy-because I realized I’d been fighting my own body for YEARS.
Richard Thomas
December 5, 2025 AT 21:17It is imperative to note that while the aggregate data from meta-analyses indicate a statistically significant improvement in ovulation rates, the clinical significance of these findings remains debatable when considering heterogeneity across patient populations, dosing regimens, and concomitant interventions. The generalizability of these outcomes to the broader PCOS cohort is not unequivocally established.
Mary Kate Powers
December 7, 2025 AT 20:08If you’re reading this and feeling overwhelmed-take a breath. You’re not broken. You’re not failing. You’re just waiting for your body to catch up. Metformin might be the quiet ally you didn’t know you needed.
Sara Shumaker
December 8, 2025 AT 09:30It’s fascinating how a drug from the 1950s, originally used for malaria, became the cornerstone of reproductive metabolic health. We keep looking for new miracles, but sometimes the answer was in our medicine cabinets all along.
Scott Collard
December 9, 2025 AT 13:34Have you considered the ethical implications of prescribing metformin to non-obese women? Are we medicalizing normal variation?
Peter Axelberg
December 11, 2025 AT 01:43My Nigerian cousin took metformin for 8 months and got pregnant on her own. No IVF. No fancy clinics. Just a $5 pill and some patience. Meanwhile, my sister spent $30k on IVF and still didn’t get a baby. The system is broken.
Jennifer Wang
December 12, 2025 AT 08:34Metformin is indicated for insulin resistance in PCOS patients. Treatment efficacy should be evaluated via fasting insulin levels and HOMA-IR indices. Clinical correlation with ovulation should be confirmed via serial transvaginal ultrasound and serum progesterone assays.
linda wood
December 13, 2025 AT 06:19So you're telling me the same drug that helps diabetics live longer also helps women with PCOS actually get pregnant? And people still think this is 'just a weight loss pill'? 😅
Richard Thomas
December 13, 2025 AT 08:28It is imperative to note that while the aggregate data from meta-analyses indicate a statistically significant improvement in ovulation rates, the clinical significance of these findings remains debatable when considering heterogeneity across patient populations, dosing regimens, and concomitant interventions. The generalizability of these outcomes to the broader PCOS cohort is not unequivocally established.