Heartburn during pregnancy isn’t just annoying-it’s common. Up to 80% of pregnant people experience it, especially in the second and third trimesters. The growing baby presses on the stomach, and hormones like progesterone relax the valve that keeps acid down. You’re not imagining it. But when your chest burns and your throat feels like it’s on fire, you want relief-fast. The question isn’t whether you should treat it. It’s: what’s safe?
First-Line Defense: Antacids
Start with antacids. They’re the go-to for a reason. Calcium carbonate, found in Tums and Rolaids, works fast. It neutralizes stomach acid right where it is, giving you relief in minutes. And here’s the bonus: your baby needs calcium to build bones. Taking Tums doesn’t just ease your heartburn-it helps your baby grow. That’s why doctors often say it’s the safest option. But not all antacids are created equal. Avoid anything with aluminum hydroxide or magnesium trisilicate. Aluminum can cause constipation and may build up in your system. Magnesium trisilicate? It’s linked to rare but serious issues in newborns. Stick to calcium carbonate or magnesium hydroxide-based products like Mylanta. Just don’t overdo it. More than 1,500 mg of calcium carbonate a day can lead to high calcium levels, kidney stones, or constipation. Stick to the label: 500-1,500 mg every 4-6 hours as needed. And never take antacids with other meds-wait at least two hours. They can interfere with iron, antibiotics, or thyroid pills.Second-Line: H2 Blockers
If antacids aren’t cutting it after a few days, talk to your provider about H2 blockers. These reduce acid production instead of just neutralizing it. Famotidine (Pepcid) is the top choice. It’s been studied in thousands of pregnant women. No increased risk of birth defects. No signs of harm to the baby. It starts working in about an hour and lasts up to 12 hours-perfect for nighttime heartburn. Ranitidine (Zantac) used to be popular. But in April 2020, the FDA pulled it off shelves worldwide because of a cancer-causing contaminant called NDMA. Don’t use it. Ever. Even if you have old bottles lying around. Cimetidine (Tagamet) is another H2 blocker, but it’s less preferred because it can interact with other drugs. Stick with famotidine. It’s the clear winner. Side effects? Rare. Maybe a headache or dizziness in a few people. But compared to the relief it gives, the risks are minimal. Most providers will only suggest this after antacids fail. And even then, they’ll recommend the lowest effective dose for the shortest time.Third-Line: Proton Pump Inhibitors (PPIs)
If you’re still burning after antacids and H2 blockers, your doctor might consider a PPI. These are stronger. They shut down acid production at the source-the proton pumps in your stomach lining. Omeprazole (Prilosec) is the most studied. Lansoprazole (Prevacid) and pantoprazole (Protonix) are also options, but there’s less data on them. Studies show no major increase in birth defects with omeprazole. But here’s the catch: a 2019 study in JAMA Pediatrics found a small possible link between first-trimester PPI use and childhood asthma. Not proven. Not causal. But enough to make doctors cautious. That’s why PPIs aren’t first or even second choice. They’re reserved for severe, persistent cases where lifestyle changes and other meds haven’t worked. PPIs take longer to kick in-1 to 4 hours. But they last all day. That’s great if you’re suffering all day. But long-term use? It may affect calcium absorption over time. That’s why doctors won’t prescribe them for weeks or months unless absolutely necessary. And never start one without talking to your OB/GYN or a gastroenterologist.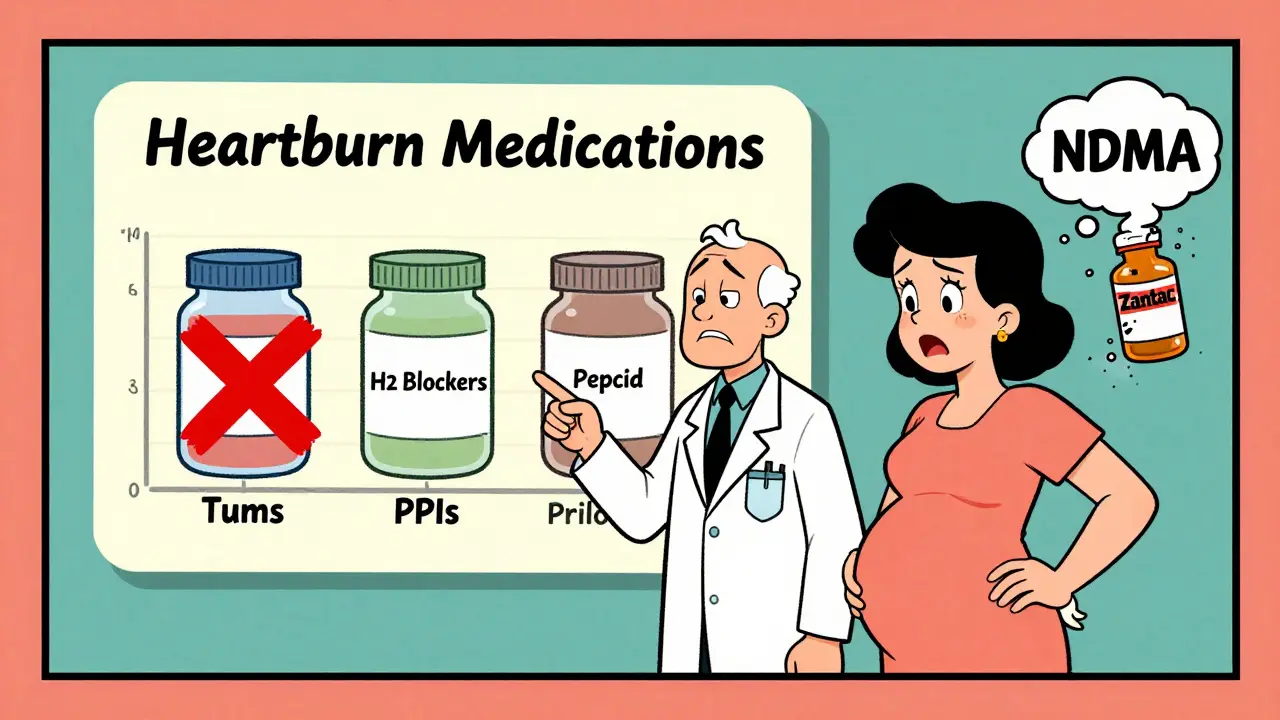
What NOT to Take
Some meds are straight-up dangerous during pregnancy. Pepto-Bismol? Avoid it. It contains bismuth subsalicylate, which turns into aspirin in your body. Aspirin in pregnancy increases the risk of bleeding, premature closure of a fetal blood vessel, and low birth weight. Even one dose isn’t worth it. Also skip any product with “aspirin,” “salicylate,” or “NSAID” on the label. That includes Advil, Aleve, and most cold and flu combos. Even if it says “for heartburn,” check the ingredients. Many contain hidden NSAIDs. And don’t assume “natural” means safe. Herbal teas like licorice root or chamomile? No solid safety data. Ginger is fine for nausea, but don’t use it as a heartburn cure unless your provider says so.Timing Matters-Especially in the First Trimester
The first 14 weeks of pregnancy are when your baby’s organs are forming. That’s the most sensitive window. Most experts agree: avoid all OTC medications during this time unless absolutely necessary. If your heartburn is mild, stick to lifestyle fixes. Eat smaller meals. Don’t lie down for three hours after eating. Skip spicy, fatty, or acidic foods. Wear loose clothes. Prop yourself up with pillows at night. If you’re struggling badly in the first trimester? Talk to your provider. They might suggest calcium carbonate antacids-still considered safest. But even then, use them only when needed. Don’t make it a daily habit without guidance.Non-Medication Strategies That Actually Work
Medication isn’t the only answer. In fact, many women find relief without any pills at all.- Eat five or six small meals instead of three big ones.
- Wait at least three hours after eating before lying down or going to bed.
- Keep your head elevated 6-8 inches while sleeping. Use a wedge pillow or stack regular pillows.
- Avoid trigger foods: citrus, tomatoes, chocolate, coffee, carbonated drinks, fried foods.
- Drink fluids between meals, not with them. Too much liquid during meals can stretch your stomach.
- Chew gum after meals. It boosts saliva, which helps neutralize acid.
- Try wearing loose clothing around your waist. Tight jeans or belly bands can push stomach contents upward.

When to Call Your Doctor
Heartburn is normal. But pain isn’t. If you have any of these, call your provider right away:- Difficulty swallowing or pain when swallowing
- Vomiting blood or black, tarry stools
- Unexplained weight loss
- Heartburn that wakes you up at night
- Symptoms that don’t improve with antacids or lifestyle changes
What About Breastfeeding?
If you’re nursing, you’re probably wondering: can I still take these? Yes, most are safe. Calcium carbonate passes into breast milk in tiny amounts-no effect on the baby. Famotidine and omeprazole are also considered compatible with breastfeeding. The amount that gets into milk is too low to cause harm. Still, always check with your provider. Some medications are safe for pregnancy but not for nursing, and vice versa. Your doctor can help you pick the best option for both stages.Bottom Line: Safer Options, Smart Choices
You don’t have to suffer through heartburn during pregnancy. There are safe, effective ways to manage it. Start with lifestyle changes. Then, if you need more, use calcium carbonate antacids like Tums. If that’s not enough, famotidine is your next best bet. Save PPIs for when nothing else works-and only with your doctor’s approval. Avoid anything with aspirin. Don’t guess. Don’t rely on internet advice. Talk to your provider. They know your history, your health, and your baby’s needs. What’s safe for one person might not be right for you. Pregnancy is already a rollercoaster. You don’t need heartburn adding to the ride. With the right approach, you can get relief-and peace of mind.Can I take Tums every day during pregnancy?
Tums are generally safe for occasional use during pregnancy, but not for daily, long-term use without medical advice. Taking more than 1,500 mg of calcium carbonate per day can lead to high calcium levels, constipation, or kidney stones. If you need heartburn relief daily, talk to your provider. You may need a different strategy, like an H2 blocker or lifestyle changes.
Is famotidine (Pepcid) safe in the first trimester?
Famotidine is considered safe in the first trimester, but most providers recommend trying lifestyle changes and antacids first. While no major risks have been linked to famotidine in early pregnancy, the first 14 weeks are the most sensitive for fetal development. Use it only if symptoms are severe and other options haven’t worked.
Can PPIs cause birth defects?
Large studies have not shown that omeprazole or other PPIs cause birth defects. However, one study found a small possible association between first-trimester PPI use and childhood asthma-but this doesn’t mean PPIs cause asthma. The risk, if any, is very low. PPIs are only prescribed when benefits clearly outweigh potential risks, and usually after other treatments fail.
Why was Zantac taken off the market?
Zantac (ranitidine) was removed from the market in April 2020 because the FDA found it contained NDMA, a probable human carcinogen. Even small amounts over time could increase cancer risk. It’s no longer available anywhere in the U.S. or most other countries. Do not use it, even if you have old bottles.
Are natural remedies like apple cider vinegar safe for heartburn in pregnancy?
There’s no solid scientific evidence that apple cider vinegar helps heartburn in pregnancy-and it may make it worse. Vinegar is acidic, and drinking it can irritate your esophagus. Some people swear by it, but it’s not recommended by medical professionals. Stick to proven methods: antacids, H2 blockers, and lifestyle changes.







lisa Bajram
January 11, 2026 AT 20:06Okay, but can we talk about how Tums are basically baby calcium supplements with a side of relief? I took them daily in my third trimester and my OB literally said, 'Keep going, you're doing great for the baby.' My daughter's teeth are perfect-no cavities at all. Also, chewing gum after meals? Game changer. I started doing it and my heartburn dropped by 70%. No pills, no stress. Just gum, small meals, and a wedge pillow. You’re not broken-you’re just pregnant. And this? This is totally normal.
neeraj maor
January 12, 2026 AT 00:04Let’s be real-PPIs are a corporate scam wrapped in a clinical trial. The JAMA Pediatrics study? They didn’t even control for breastfeeding habits or maternal diet. And why is omeprazole ‘most studied’? Because Big Pharma paid for the research. Meanwhile, the FDA banned Zantac for NDMA but let PPIs slide? That’s not science-that’s profit. I’ve seen three pregnant women on PPIs develop severe B12 deficiency. No one talks about that. You think your doctor’s looking out for you? They’re just following the algorithm.
Dwayne Dickson
January 13, 2026 AT 10:45While I appreciate the clinical rigor of the original post, I must respectfully assert that the omission of pharmacokinetic data regarding placental transfer coefficients for famotidine and omeprazole constitutes a significant epistemic lacuna. The assertion of ‘safety’ is predicated on observational cohort studies with confounding variables unaddressed-particularly maternal BMI, gestational diabetes status, and concomitant use of iron supplements. In my professional capacity as a clinical pharmacologist, I would urge readers to consult a pharmacovigilance database prior to self-administration, lest they inadvertently induce iatrogenic hypocalcemia or subtherapeutic antibiotic efficacy.
Michael Marchio
January 13, 2026 AT 20:20Look, I get it-you want to feel like you’re doing everything right. But let’s not pretend this is all about ‘safety.’ It’s about control. We’re told to eat six tiny meals, sleep at a 45-degree angle, avoid chocolate, and chew gum like it’s our job-while our bodies are literally being rewired to grow a human. Meanwhile, the medical industry sells us antacids like they’re vitamins and then acts shocked when we’re still in pain. And don’t even get me started on the ‘natural remedies’ crowd. Apple cider vinegar? That’s just stomach acid with a fancy label. If you’re still burning after Tums and famotidine, you’re not failing-you’re just pregnant. And that’s okay. You don’t need to ‘optimize’ your way out of this. Sometimes, you just need to lie down, breathe, and let your body do its thing. The rest is noise.
Also, the fact that we have to Google whether our heartburn meds might cause asthma in 2035? That’s not medicine. That’s anxiety marketing.
Kunal Majumder
January 15, 2026 AT 09:40Bro, I'm from India and my mom used to give me ajwain water for heartburn when I was a kid. Turns out, it's carom seeds-natural antispasmodic. I drank it during my wife's pregnancy and she said it helped more than Tums. No science? Maybe not. But real women have been using this for centuries. Just warm water, a pinch of ajwain, sip slow. No pills. No side effects. And yeah, it smells weird-but so does pregnancy. Try it. What do you have to lose?
Jaqueline santos bau
January 16, 2026 AT 15:06OMG I took Zantac for 3 months in my first trimester and now I’m terrified. Like… what if my kid gets cancer? I didn’t know it was banned until last week. I have a bottle in my cabinet right now. Should I throw it out? Should I tell my OB? What if they judge me? I already feel like a terrible mom for not reading the label. I cried for an hour. I just wanted to sleep. Why is everything so damn complicated??
Aurora Memo
January 18, 2026 AT 14:49To the person above: you’re not a terrible mom. You were trying to find relief. That’s love, not negligence. The system failed you by not making warnings clearer. And the fact that you’re even asking this question means you care deeply. Please talk to your provider-they’ve seen this before. No judgment. Just support. You’re doing better than you think.
chandra tan
January 20, 2026 AT 03:48My cousin in Bangalore took Tums daily for 8 months. Her baby was born at 8 lbs, no issues. Her doctor said, 'If it works, keep going.' Meanwhile, her sister took PPIs and had a preterm baby. Coincidence? Maybe. But I’m sticking with Tums. Simple. Safe. Works. No drama. No conspiracy. Just a pill that helps. And if you’re still hurting? Elevate your bed. Drink water between meals. Stop eating at 7 PM. Your body’s not broken. It’s just building a person. Be gentle with it.