Most people take medications without a second thought. But for some, even a simple pill can trigger a life-threatening reaction. Drug allergies aren’t just rashes or upset stomachs-they’re immune system overreactions that can turn a routine treatment into a medical emergency. The truth? Many people think they’re allergic to common drugs like penicillin or ibuprofen, but they’re wrong. And that mistake is costing lives, time, and money.
Penicillin: The Most Misunderstood Drug Allergy
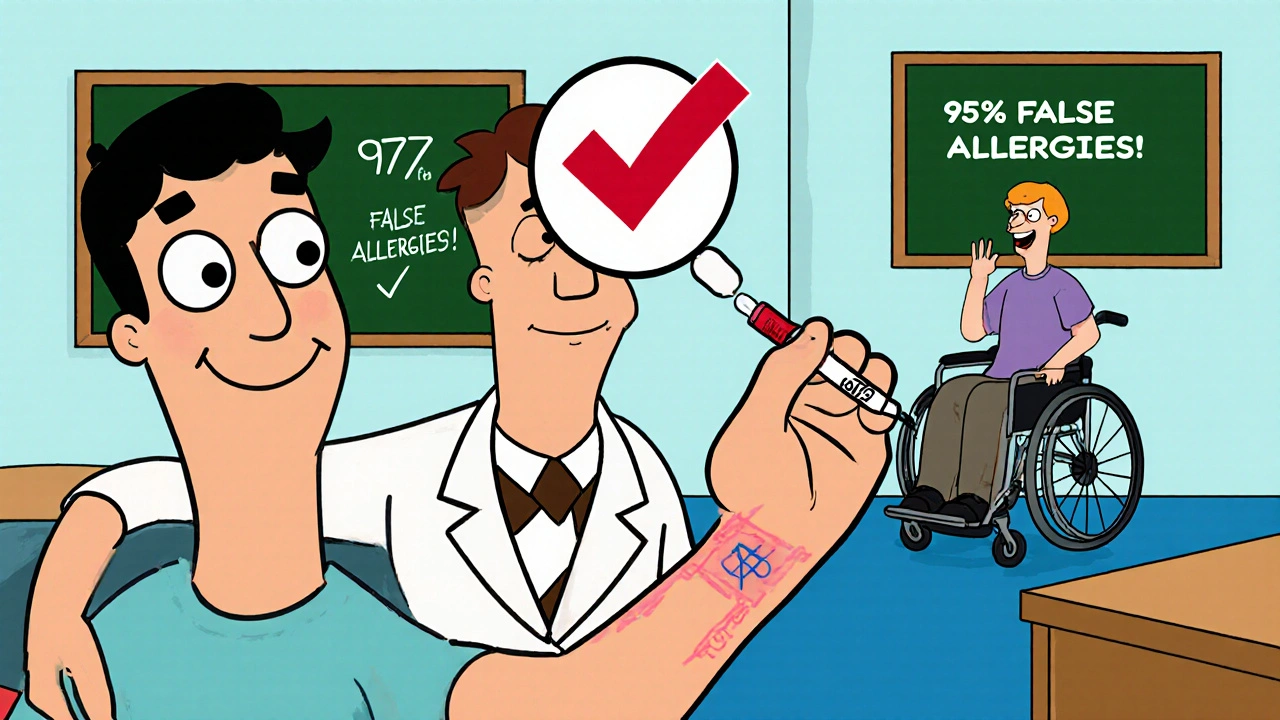
Penicillin is the number one drug people say they’re allergic to. About 1 in 10 Americans claim a penicillin allergy. But here’s the twist: more than 95% of them aren’t truly allergic. That’s not a typo. Studies from Massachusetts General Hospital show that after proper testing, almost everyone who thinks they’re allergic to penicillin can take it safely. Why does this matter? Because when doctors avoid penicillin due to a false label, they reach for stronger, pricier antibiotics like vancomycin or clindamycin. These drugs are less effective against common infections, more likely to cause side effects like C. diff diarrhea, and contribute to antibiotic resistance.The real danger? Anaphylaxis. Penicillin causes around 400 deaths each year in the U.S. from severe allergic reactions. But here’s the good news: if you’ve been told you’re allergic to penicillin, you can get tested. Skin testing with Pre-Pen and an oral amoxicillin challenge is 97-99% accurate. It takes a few hours. It’s safe. And it can change your entire medical future.
Other Antibiotics That Trigger Reactions
Penicillin isn’t the only culprit. Sulfa drugs like Bactrim (trimethoprim-sulfamethoxazole) cause reactions in about 3% of the general population. But for people with HIV, that number jumps to 60%. These reactions can be mild-itchy rash-or severe, like Stevens-Johnson syndrome, where the skin starts peeling off. It’s not just about the drug itself. Some people react because their immune system mistakes a metabolite (a breakdown product) of the drug as a threat.Cephalosporins, another class of antibiotics, are often avoided in people with penicillin allergies. But cross-reactivity is actually very low-only 1-3%. That’s far less than the old 10% myth. If you’ve had a mild rash from penicillin years ago, you’re probably fine with a cephalosporin today. But if you had anaphylaxis, proceed with caution and get tested.
NSAIDs: More Than Just a Headache
Ibuprofen, naproxen, aspirin-these are the go-to pain relievers for millions. But for some, they’re triggers for something called NSAID-exacerbated respiratory disease. It’s not a classic allergy. It’s a hypersensitivity. People with asthma or nasal polyps are especially at risk. About 7% of adults with asthma and 14% with nasal polyps have this condition. When they take NSAIDs, their airways tighten, their nose swells, and they can struggle to breathe. It’s not IgE-mediated like peanut allergies. It’s caused by how the body processes prostaglandins. The fix? Avoid NSAIDs entirely. Acetaminophen (Tylenol) is usually safe. But if you need an NSAID, your allergist might try a controlled challenge under supervision.Anticonvulsants and the Hidden Genetic Risk
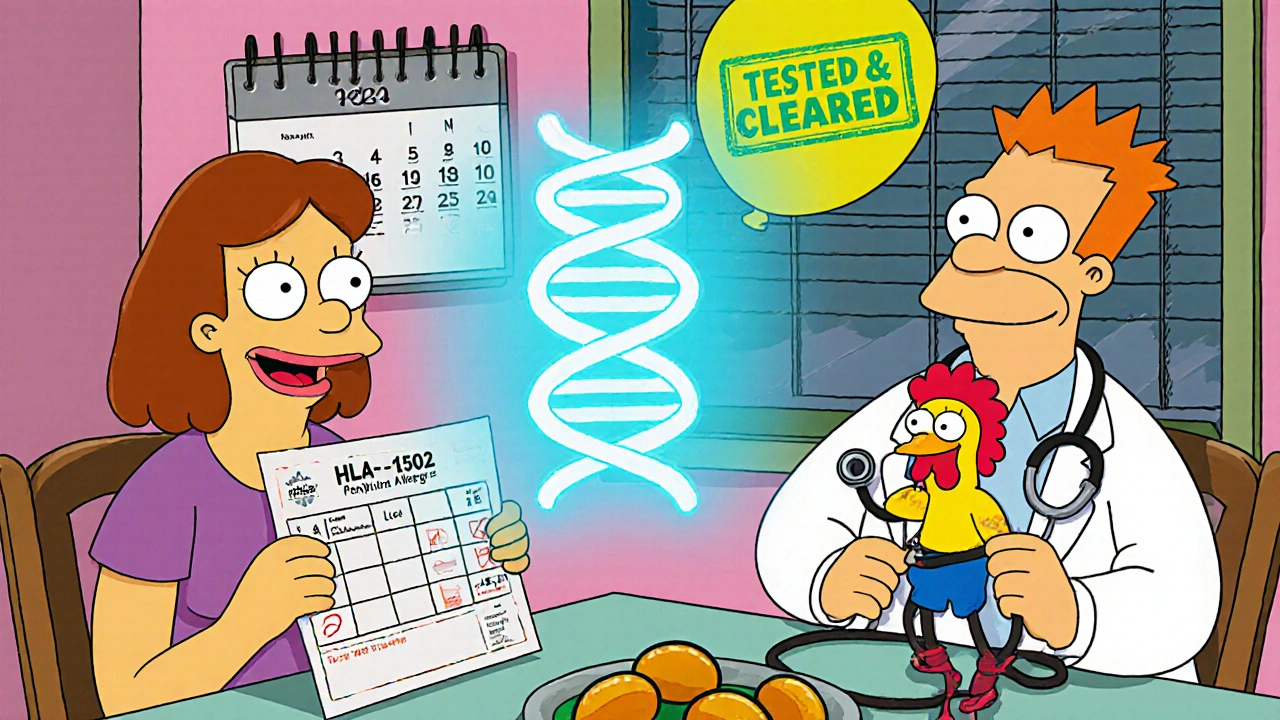
Carbamazepine (Tegretol), lamotrigine (Lamictal), and phenytoin are life-saving for people with epilepsy or bipolar disorder. But they’re also among the most dangerous drugs for certain populations. Carbamazepine can trigger Stevens-Johnson syndrome or toxic epidermal necrolysis-rare but deadly skin conditions. The risk isn’t random. It’s tied to a gene: HLA-B*1502. If you’re of Southeast Asian descent-Thai, Malaysian, Chinese, Filipino-your chance of carrying this gene is 10-15%. In European populations, it’s under 1%. The FDA recommends testing for this gene before starting carbamazepine. In Taiwan, where this became routine, cases of SJS dropped by 90%.Lamotrigine causes rash in 5-10% of users. Most are mild. But in 1 out of every 1,250 people, it turns serious. The rash usually shows up within the first few weeks. If you notice red spots, blisters, or peeling skin, stop the drug immediately and get help. Don’t wait.
Chemotherapy and Biologics: When Treatment Itself Becomes a Threat
Cancer treatments are designed to kill fast-growing cells. But sometimes, they also trigger the immune system to attack the drug itself. Taxanes like paclitaxel (Taxol) cause hypersensitivity in up to 41% of patients. Monoclonal antibodies like cetuximab (Erbitux) trigger infusion reactions in nearly 1 in 5 patients. These reactions can happen within minutes: flushing, low blood pressure, wheezing, even cardiac arrest.The good news? These reactions can be managed. Hospitals use premedication-steroids and antihistamines-before giving these drugs. Slow infusion rates help too. Desensitization protocols exist for patients who need the drug but reacted before. They involve tiny, gradually increasing doses over hours. Success rates are 80-90%. It’s not ideal, but it’s often the only way to get life-saving treatment.
Contrast Dyes and Imaging Risks
When you get a CT scan with contrast dye, you’re not allergic to iodine. That’s a myth. The reaction is to the molecule surrounding the iodine. About 1-3% of people have some kind of reaction-itching, nausea, hives. Severe reactions? Only 1 in 2,500 to 1 in 10,000. But if you’ve had one before, your risk goes up. Pre-medication with steroids and antihistamines cuts the chance of a moderate or severe reaction from 12.7% down to just 1%. If you’re scheduled for an MRI or CT scan and have a history of reactions, tell your radiologist. They can adjust the protocol.Why Mislabeling Is a Public Health Crisis
A 2017 study in JAMA Internal Medicine found that people labeled as penicillin-allergic stayed in the hospital half a day longer, got more expensive antibiotics, and spent over $1,000 more per admission. Multiply that across millions of patients, and the U.S. healthcare system loses $1.2 billion a year. But the real cost? Antimicrobial resistance. When we overuse broad-spectrum antibiotics, we create superbugs. Every time a doctor avoids penicillin because of a false allergy, we move one step closer to a world where common infections can’t be treated.And here’s the kicker: 68% of people with a drug allergy label never got tested. They just accepted it. They don’t know they can be cleared. They don’t know they might have outgrown it. Penicillin allergies fade over time. After 10 years without exposure, 80% of people lose their sensitivity.
What You Can Do
If you’ve been told you’re allergic to a drug:- Don’t assume it’s true. Ask: What happened? When? How severe?
- If it was a rash that appeared days later, it might not be IgE-mediated. That’s different from hives or swelling within minutes.
- Ask your doctor for a referral to an allergist. Skin testing and oral challenges are safe, accurate, and covered by most insurance.
- If you’re scheduled for surgery or need antibiotics, bring your allergy list. Don’t let a decades-old label dictate your care.
And if you’re a parent: kids often get labeled with penicillin allergy after a mild rash. But most outgrow it. Don’t let that label follow them into adulthood without verification.
Testing and Diagnosis: The Path Forward
There’s no single blood test for drug allergies. Diagnosis relies on three things:- History: When did the reaction happen? What were the symptoms? Did you get worse with repeated exposure? (Spoiler: you usually don’t.)
- Testing: Skin prick and intradermal tests for penicillin and some other drugs. These are highly predictive.
- Challenge: A controlled, supervised dose of the drug under medical care. This is the gold standard for confirming or ruling out an allergy.
For high-risk drugs like carbamazepine or abacavir, genetic screening is now standard. HLA-B*57:01 testing before abacavir use cut hypersensitivity from 8% to 0.4%. That’s prevention at its best.
What’s Next?
The future of drug allergy care is moving fast. Point-of-care genetic testing will soon be routine before prescribing high-risk drugs. Telehealth penicillin allergy clinics are cutting wait times from months to days. Electronic health records are being updated to flag suspected false allergies and prompt re-evaluation.But none of this matters if patients don’t speak up. If you’ve been told you’re allergic to a drug, ask: Is this really true? You might be carrying a label that’s holding you back-from better treatments, lower costs, and fewer side effects.
Can you outgrow a drug allergy?
Yes, especially with penicillin. About 80% of people who had a penicillin allergy as a child lose it after 10 years without exposure. Even if you had a reaction in your 20s, you may be fine now. Testing can confirm this.
Is a rash always a sign of drug allergy?
No. Many rashes after taking a drug are not allergic. Viral infections, heat, or even the drug’s side effects can cause rashes. True allergic rashes often come with itching, swelling, or hives. Delayed rashes (appearing days later) are often T-cell mediated, not IgE-driven. A doctor can help tell the difference.
Can you be allergic to NSAIDs but still take Tylenol?
Yes. Acetaminophen (Tylenol) works differently than NSAIDs and doesn’t trigger the same immune response. It’s usually safe for people with NSAID hypersensitivity. But always check with your doctor before switching, especially if you’ve had severe reactions.
Do all drug allergies cause anaphylaxis?
No. Most reactions are mild-rash, itching, hives. Anaphylaxis is rare but serious. It involves breathing trouble, low blood pressure, dizziness, or swelling of the throat. If you’ve ever had a reaction like this, you need to carry an epinephrine auto-injector and see an allergist.
Is penicillin allergy testing safe?
Yes. Skin testing and oral challenges are done under medical supervision with emergency equipment on hand. The risk of a reaction during testing is less than 1%. The benefit-being able to safely use the most effective, cheapest antibiotic-is huge.
Why do some people react to sulfa drugs but not others?
It’s not about sulfa itself-it’s about how your body breaks down the drug. People with HIV have a higher risk because their immune systems are already altered. Some people have genetic differences in how their liver processes sulfonamides, leading to toxic metabolites that trigger immune reactions. It’s unpredictable, which is why doctors monitor closely when starting these drugs.
Can you develop a drug allergy after taking it for years?
Yes. Drug allergies can appear after months or even years of use. Your immune system can suddenly start recognizing the drug as a threat. This is common with antibiotics, anticonvulsants, and chemotherapy. If you develop a new rash, fever, or breathing trouble after starting a drug-even if you’ve taken it before-stop it and contact your doctor.
Are there any drugs that are completely safe for people with drug allergies?
No drug is 100% safe for everyone. But some have very low risk. For example, if you’re allergic to penicillin, acetaminophen, or metformin are generally safe. If you’re allergic to NSAIDs, tramadol or gabapentin may be alternatives. The key is working with an allergist to map out your safe options based on your history.






jim cerqua
November 21, 2025 AT 16:40This is the most important public health issue nobody talks about. I had a penicillin label since I was 5 because I got a rash after amoxicillin. Turned out it was a virus. Now I’m 37 and spent 12 years on vancomycin for sinus infections because doctors were scared. I just got tested last month. Turned out I’m fine. I cried. Not because I was allergic-I was just lied to by the system.
Donald Frantz
November 23, 2025 AT 08:50Let’s be clear: the CDC and FDA have known about this for over a decade. The fact that 68% of people never get tested is not negligence-it’s institutional laziness. Hospitals don’t want to pay for allergists. Insurance won’t cover challenges unless you’re already in crisis. This isn’t about medicine. It’s about profit margins disguised as caution.
Debanjan Banerjee
November 23, 2025 AT 17:29As an infectious disease specialist in Mumbai, I see this daily. Patients come in with documented penicillin allergies and are given azithromycin for pneumonia-despite clear guidelines recommending amoxicillin-clavulanate as first-line. The cost difference? $3 vs $120 per course. And the resistance rates? Skyrocketing. We need mandatory allergy re-evaluation in primary care. Not optional. Mandatory. It’s not just ethical-it’s epidemiological common sense.
Sheldon Bazinga
November 25, 2025 AT 05:00so like… the government is lying to us? and doctors are just… scared to use penicillin? lmao. i bet they’re all just trying to sell us more expensive drugs. next they’ll say aspirin causes cancer and we should all drink bleach. #BigPharmaLies
Sandi Moon
November 27, 2025 AT 00:32One must wonder: is this ‘penicillin allergy’ misdiagnosis truly an error-or a carefully orchestrated diversion? The pharmaceutical industry profits immensely from broad-spectrum antibiotics. The CDC’s own data shows a direct correlation between penicillin avoidance and increased carbapenem use-a class of drugs that, coincidentally, are patented by the same conglomerates that fund medical education. The timing is too perfect. This is not science. It is economic warfare disguised as public health.
Kartik Singhal
November 28, 2025 AT 02:25Bro… why are we even talking about this? 🤡 I mean, if you're allergic to penicillin, just don't take it. Why make it a whole thing? Also, why are we trusting doctors who can't even spell 'antibiotic' right? 🤷♂️ #TrustTheProcess #PharmaIsTheEnemy
Logan Romine
November 29, 2025 AT 12:46So let me get this straight-we’re supposed to believe that the immune system, the most complex biological system known to man, can be ‘wrong’ about a drug… but somehow, the FDA and Big Pharma are always right? 😏
Maybe the real allergy is to critical thinking. Maybe the drug didn’t make you sick… the system did. You’re not allergic to penicillin. You’re allergic to medical dogma.
Chris Vere
November 30, 2025 AT 07:53This is good information. People need to know that a rash is not always an allergy. In Nigeria we see many children given antibiotics for fever and then get a rash from the virus. Doctors say 'allergy' and the family never gives that drug again. But the child grows up and gets pneumonia and dies because the right drug was never used. We must educate. Not just test. Educate.
Pravin Manani
December 1, 2025 AT 20:29From a pharmacogenomics standpoint, the HLA-B*1502 association with carbamazepine-induced SJS is one of the most robust examples of precision medicine in clinical practice. The fact that Taiwan implemented population-wide screening and reduced SJS incidence by 90% is a textbook case of translational success. We need similar protocols for abacavir (HLA-B*57:01), allopurinol (HLA-B*58:01), and even lamotrigine. The infrastructure exists. What’s missing is political will and reimbursement models.
Daisy L
December 2, 2025 AT 20:19OMG. I just found out my 12-year-old has a ‘penicillin allergy’ because she got a rash after amoxicillin… but she was sick with mono at the time!! I’m so mad. I’ve been avoiding every antibiotic for her since she was 2. Now I’m calling an allergist tomorrow. This is insane. How many families are living like this???
Swati Jain
December 4, 2025 AT 18:02Let’s be real-most ‘drug allergies’ are just bad timing + bad diagnosis. I had a rash after ibuprofen? Probably because I was dehydrated and had a viral exanthem. But now I’m labeled ‘NSAID allergic’ and get acetaminophen for migraines… which doesn’t work. So I suffer. And pay more. And get opioid prescriptions. Thanks, medicine.
Florian Moser
December 6, 2025 AT 14:45If you’ve been told you’re allergic to a drug, don’t just accept it. Push for testing. It’s not a burden-it’s a gift. You’re not being difficult. You’re being smart. And if your doctor pushes back? Find a new one. Your health is not a suggestion. It’s your right. You’ve got this.
Sammy Williams
December 6, 2025 AT 17:41My grandma’s been avoiding penicillin since the 60s. She just found out last year she’s not allergic. Now she’s like ‘why didn’t anyone tell me?’ I’m telling everyone I know now. This needs to go viral.
Julia Strothers
December 8, 2025 AT 02:48They’re lying. They always lie. Penicillin isn’t dangerous-it’s the testing that’s dangerous. They want you to think you’re allergic so you’ll take their expensive, patented, overpriced ‘alternatives.’ And when you get C. diff from vancomycin? That’s just collateral damage. Wake up. This is control. Not care.