When you walk into a pharmacy and can’t find the insulin your child needs, or your doctor tells you the generic version of your blood pressure medication is out of stock, you’re not just dealing with bad luck. You’re feeling the direct impact of pricing pressure and shortages in the healthcare system. These aren’t temporary hiccups-they’re structural problems that have been building for years and exploded during and after the pandemic. And they’re making essential care harder to get and more expensive to afford.
Why Medications Keep Disappearing from Shelves
Shortages of medicines aren’t random. They happen when the supply chain breaks down at one or more points: raw materials don’t arrive, manufacturing plants shut down, shipping routes get blocked, or distributors can’t afford to carry certain drugs because the prices don’t cover their costs. Between 2020 and 2023, the U.S. Food and Drug Administration recorded over 1,500 active drug shortages. Many of these involved generic drugs-things like antibiotics, IV fluids, and heart medications-that are supposed to be cheap and widely available. Why? Because manufacturers stopped making them. Why did they stop? Because the prices paid by insurers and government programs hadn’t kept up with rising costs for ingredients, labor, and energy. Take IV saline, for example. In 2022, hospitals across the U.S. faced critical shortages. One major supplier shut down its plant due to contamination, and other manufacturers couldn’t ramp up fast enough. Why? Because the price of saline hadn’t changed in over a decade. Even as energy costs jumped 40% and shipping fees doubled, companies couldn’t raise prices to cover expenses without risking losing contracts with big buyers like Medicare and Medicaid. So they cut production. The result? Patients waited hours in emergency rooms for fluids they needed to survive.How Pricing Pressure Turns Into Patient Risk
Pricing pressure doesn’t just mean higher bills. It means harder choices. When a drug becomes too expensive for a hospital to stock, they either ration it or switch to a more costly alternative. That switch often means patients get less effective treatments or face new side effects. A 2023 study in the Journal of the American Medical Association found that when the generic version of the antibiotic cefazolin went out of stock, hospitals switched to vancomycin. It worked-but it cost 12 times more and carried a higher risk of kidney damage. Patients who needed simple surgery started getting complications because the cheaper, safer option wasn’t available. This isn’t just happening in the U.S. The European Medicines Agency reported a 30% increase in medicine shortages across EU countries between 2021 and 2023. In Australia, where public drug subsidies cover most prescriptions, the PBS (Pharmaceutical Benefits Scheme) had to temporarily restrict access to 17 common drugs in 2022 because suppliers couldn’t meet demand at the set price. The real cost? Lives. Delayed treatments. Worse outcomes. And more people skipping doses or going without because they can’t afford the alternatives.Who’s Behind the Bottlenecks?
It’s easy to blame pharmaceutical companies. But the real problem is a system that rewards low prices over reliability. Most generic drugs are made in just a few countries-India and China supply over 80% of the world’s active pharmaceutical ingredients. When a single factory in India shuts down for regulatory violations, or a port in Shanghai closes due to lockdowns, it ripples across the globe. There’s no backup. No redundancy. No buffer. Add to that the fact that most drug makers operate on razor-thin margins. The average profit margin on a generic antibiotic is less than 5%. Compare that to brand-name drugs, which can have margins over 70%. So companies invest in the profitable stuff. The cheap, essential ones? They’re treated like commodities-until they disappear. Even logistics are broken. The cost to ship a container of medicine from Asia to North America jumped from $3,000 in 2019 to $22,000 in 2021. Insurance companies and government programs didn’t raise their reimbursement rates to match. So suppliers stopped shipping. And patients paid the price.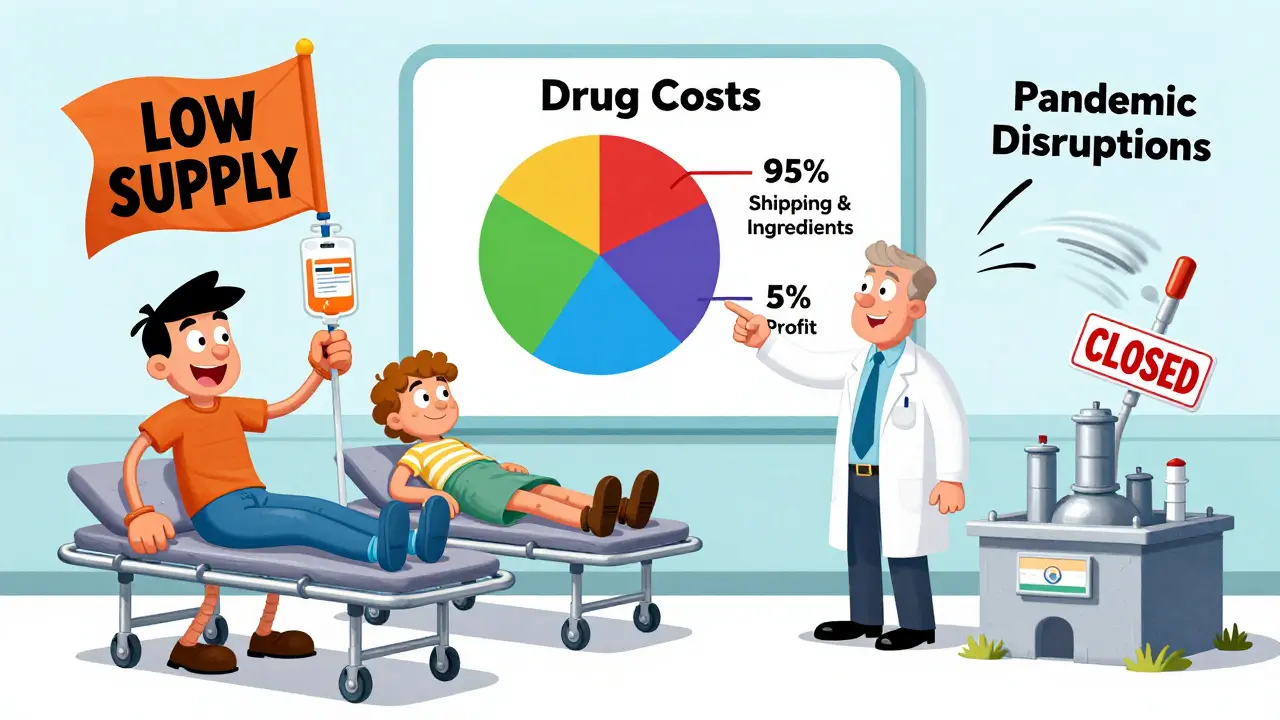
What Happens When Prices Are Frozen
Governments often try to fix high prices by capping them. But in healthcare, that can make shortages worse. In the UK, the government imposed a price cap on insulin in 2021 to keep it affordable. It worked-for a while. But manufacturers couldn’t cover rising production costs. Within 18 months, two major suppliers pulled out of the UK market. The result? A national shortage. Patients had to switch brands, sometimes with dangerous side effects. The same thing happened in Canada with the antibiotic azithromycin. When the government refused to raise the price despite soaring ingredient costs, distributors stopped importing it. Hospitals had to ration doses. Emergency rooms started turning away patients with pneumonia. Economists call this the “price ceiling paradox.” When you force prices down below what it costs to produce something, you don’t get more of it-you get less. And in healthcare, less means riskier care.Who Gets Hit Hardest?
It’s not just the elderly or the uninsured. It’s everyone. Low-income families are the first to feel it. When a generic drug disappears, the only alternative is often a brand-name version with a $200 co-pay. Many just stop taking it. Rural communities suffer too. Pharmacies in small towns don’t have the buying power to secure scarce drugs. They get whatever’s left after big hospital chains and chain pharmacies have taken their share. Even middle-class patients with good insurance aren’t safe. If your doctor prescribes a drug that’s out of stock, you don’t just wait a week-you wait months. Or you get a different drug that might not work as well. Or you pay out of pocket for an expensive substitute. And it’s not just pills. It’s vaccines. It’s dialysis solutions. It’s anesthetics. It’s insulin pens. Every time one of these disappears, someone’s life gets put on hold.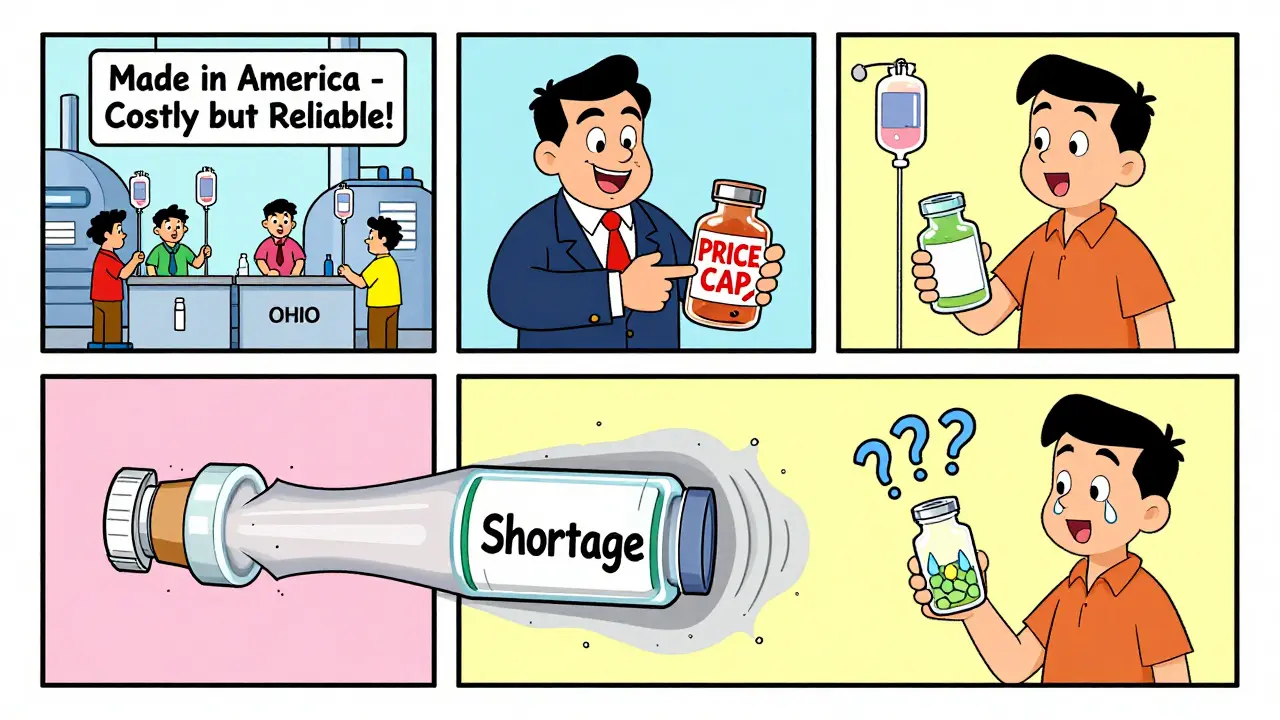
What’s Being Done-and What’s Not
Some changes are starting to happen. The U.S. passed the Drug Supply Chain Security Act in 2013, but it’s still not fully enforced. The FDA now publishes a public shortage list, which helps-but doesn’t fix the problem. A few hospitals have started stockpiling critical drugs. But that’s expensive. And if a shortage lasts a year, you’re stuck with expired inventory. Some companies are moving production closer to home. “Nearshoring” is growing. A few U.S. firms are now making generic antibiotics in Ohio and Texas instead of India. It’s more expensive-but more reliable. The problem? It takes years to build new factories. And without higher prices, it’s not profitable. The European Union tried something bold in 2022: they allowed temporary price increases for essential drugs during shortages. It worked. Within six months, 14 previously unavailable medications returned to shelves. But the policy was only meant to last a year. Now it’s expired. And shortages are creeping back.The Path Forward: Real Solutions, Not Quick Fixes
There are three things that actually work:- Price flexibility for essential drugs-Let manufacturers raise prices slightly during shortages to cover costs. Not to profit. Just to survive. This isn’t about greed. It’s about keeping the lights on.
- Diversify supply chains-Stop relying on one or two countries for 80% of your medicines. Invest in regional manufacturing hubs in North America, Europe, and Australia. It costs more upfront-but it prevents crises.
- Build strategic stockpiles-Governments should maintain a reserve of 6-12 months’ supply of the 50 most critical generic drugs. Not just for pandemics. For everyday shortages.
What You Can Do Right Now
If you’re on a chronic medication:- Ask your pharmacist if there’s a backup brand or formulation available.
- Keep a 30-day supply on hand-don’t wait until you’re out.
- Sign up for FDA or Health Department shortage alerts. They’re free and public.
- If your drug is unavailable, contact your doctor immediately. Don’t skip doses or substitute without advice.
Why are generic drugs suddenly in short supply?
Generic drugs are in short supply because manufacturers can’t make them profitably. The prices paid by insurers and government programs haven’t risen to match soaring costs for raw materials, energy, labor, and shipping. When production costs go up but the selling price stays flat, companies stop making the drug-especially if it’s low-margin. Many generics are made overseas, and disruptions in India or China-like factory shutdowns or port delays-can cut off global supply with no backup.
Can price controls cause drug shortages?
Yes. When governments cap drug prices too low, manufacturers can’t cover production costs. This leads them to stop making the drug, reduce output, or pull out of the market entirely. The UK’s insulin price cap and Canada’s azithromycin price freeze both led to national shortages within a year. Price controls don’t fix affordability-they just shift the problem from high prices to no supply.
Are brand-name drugs also affected by shortages?
Yes, but less often. Brand-name drugs have higher profit margins and more pricing flexibility, so manufacturers can absorb cost increases better. However, if a brand-name drug relies on a rare ingredient or a single foreign supplier, it can still be affected. For example, in 2022, a shortage of a key chemical used in the brand-name asthma drug Advair led to global supply delays-even though it’s a high-priced medication.
How do shortages affect hospital care?
Hospitals face tough choices: use a more expensive alternative, delay treatment, or ration the available supply. In 2022, U.S. hospitals reported using riskier, costlier antibiotics when generics ran out, leading to higher rates of complications and longer hospital stays. IV fluid shortages forced emergency rooms to limit treatments. Anesthesia shortages delayed surgeries. These aren’t minor inconveniences-they directly impact survival rates and recovery times.
What’s the long-term outlook for drug availability?
The outlook is mixed. Supply chain pressures have eased since 2022, but the underlying problems remain. Global manufacturing is still concentrated in just a few countries, and most governments haven’t invested in domestic production capacity. Experts predict shortages will continue through 2026, especially for generic drugs, unless there’s policy change. Nearshoring and digital supply chain tools are helping, but they’re slow and expensive to implement. Without price flexibility and strategic stockpiles, the cycle of shortage and scramble will keep repeating.






Stacey Marsengill
January 16, 2026 AT 15:33They keep saying 'affordability' like it's a magic word. But you can't feed a hospital with slogans. I watched my mom die because they ran out of morphine. Not because we couldn't pay. Because the company stopped making it. The price was 'too low.' So they just... vanished. Like she never mattered.
And now they want us to trust the same people who let this happen?
They don't care. They never did.
And if you think price caps are the problem, you're the one who needs to look in the mirror.
It's not about greed. It's about who gets to live and who gets to be a footnote.
They're not shortages. They're decisions.
And we're the ones paying for them.
Every. Single. Day.
Aysha Siera
January 17, 2026 AT 20:31India made 80% of your meds. Now you cry. Funny how you forget who kept your insulin cheap while your politicians stole the money. No one forced you to outsource everything and then act shocked when the pipes broke. You wanted cheap. You got chaos. You wanted the world to work for you. Now it doesn't. Welcome to karma.
China didn't steal your jobs. You sold them for a discount.
And now you want someone else to fix it?
Good luck with that.
Robert Davis
January 19, 2026 AT 07:46Let me break this down for you since the article clearly didn't. The real issue isn't pricing. It's the FDA's ridiculous regulatory delays. They take 7 years to approve a new generic plant. Seven years. Meanwhile, every time a factory in India sneezes, the whole system collapses. Why? Because we don't have a single FDA-approved plant in the continental U.S. that can make IV fluids at scale. Not one.
And no one talks about this because it's inconvenient. The FDA isn't protecting you. They're protecting bureaucracy.
Meanwhile, the EU lets manufacturers raise prices during shortages. They get drugs. We get empty shelves.
It's not capitalism. It's regulatory capture.
And you're all too busy blaming 'big pharma' to notice the real villain: the regulators who sit on their hands while people die.
Go read the FDA's own reports. They admit this. But no one listens.
Because admitting the truth means admitting we're all complicit.
Eric Gebeke
January 21, 2026 AT 07:35People think this is about money. It's not. It's about morality.
You want to know why your child's insulin is gone? Because someone decided that a life-saving drug is just another commodity. Like toilet paper. Like socks. Like a TikTok filter.
And now you're surprised when the system breaks?
It's not a supply chain issue. It's a soul issue.
When you treat human survival like a balance sheet, you don't get efficiency. You get corpses.
And the worst part? The people who profit the most from this mess? They're the ones screaming about 'market freedom.'
They don't want a free market. They want a free pass.
And you're letting them.
Robert Cassidy
January 23, 2026 AT 03:50Let’s be real. This isn’t about drugs. It’s about weakness. We used to make things here. We used to build factories. We used to have pride. Now we outsource everything to countries that don’t care if we live or die. We let China and India run our medicine supply like it’s a Walmart clearance rack.
And then we wonder why we’re vulnerable?
It’s not a shortage. It’s a surrender.
We gave up our sovereignty for a few bucks off a prescription. Now we’re begging for IV bags like beggars.
It’s not the manufacturers. It’s not the insurers.
It’s us.
We let this happen.
And now we’re mad because the bill came due?
Pathetic.
Naomi Keyes
January 23, 2026 AT 14:27According to the FDA’s 2023 Drug Shortage Report, 68% of active shortages involve sterile injectables-exactly the category with the lowest profit margins and highest regulatory burden. Furthermore, the average time to bring a new generic manufacturing facility online is 4.7 years, with 83% of those facilities located outside the U.S., primarily in India and China, where regulatory compliance rates have declined by 22% since 2018.
Meanwhile, the median gross margin for generic drugs in the U.S. is 3.8%, compared to 71.2% for brand-name biologics. This is not a market failure-it is a structural misalignment between cost recovery and reimbursement policy.
And yet, the proposed solution-price flexibility-is dismissed as 'corporate greed' while ignoring that the same system that caps prices also caps innovation, investment, and redundancy.
It is not enough to say 'we care.' We must align incentives. Otherwise, the next shortage won’t be insulin. It’ll be epinephrine. Or heparin. Or lidocaine.
And then you’ll be screaming for a solution that was available in 2021.
But no one listened.
Because listening requires accountability.
And accountability is inconvenient.
rachel bellet
January 25, 2026 AT 10:31Let’s not romanticize the 'price flexibility' fantasy. If you give manufacturers a 10% price bump during shortages, they won’t use it to rehire workers or upgrade equipment. They’ll use it to buy another yacht. The profit motive isn’t broken-it’s malignant.
And the idea that we need to 'invest in regional hubs' is laughable without public funding. Private capital won’t touch this. It’s too risky. Too slow. Too low ROI.
So who’s going to pay? Taxpayers?
Then why not just nationalize the production of the top 50 essential drugs? Like the UK does with the NHS. Like Canada does with insulin. Like Germany does with antibiotics.
It’s not socialism. It’s survival.
But no. We’d rather watch people die and call it 'market discipline.'
That’s not capitalism. That’s cruelty with a spreadsheet.
Selina Warren
January 27, 2026 AT 01:17Here’s the truth no one wants to say: We don’t need more factories. We need more courage.
We’ve been lied to for decades. 'Cheap is good.' 'Globalization is progress.' 'Let the market decide.'
But the market doesn’t care if your child breathes. It doesn’t care if your parent gets dialysis. It doesn’t care if your partner survives sepsis.
It only cares about margins.
So we have to care more.
Not with hashtags.
Not with petitions.
But with action.
Boycott the companies that profit from this. Vote for the ones who’ll fund domestic production. Demand that your hospital stockpile. Tell your senator: ‘I don’t want a cheaper drug. I want a working one.’
And if they say it’s too expensive?
Ask them how much a life costs.
Then wait for them to answer.
They won’t.
Because they already know.
And they’re still silent.
Nishant Sonuley
January 27, 2026 AT 02:50Look, I get it. You're angry. I'm angry too. But let's not pretend this is just America's problem. I'm from India. I've seen the factories. I've met the workers. They're not villains. They're people trying to survive too. The same way your neighbor is.
Here's the real issue: We're all trapped in a system designed by people who never had to choose between paying rent and buying insulin.
So yes, we need better supply chains. Yes, we need stockpiles. Yes, we need price flexibility.
But we also need to stop blaming each other.
Stop calling the Chinese 'exploiters.' Stop calling Americans 'greedy.' Stop calling regulators 'incompetent.'
They're all just cogs in a machine we built together.
So let's rebuild it-with everyone at the table.
Not as enemies.
As humans.
Because if we don't, the next shortage won't be a drug.
It'll be trust.
And that's harder to refill.
Emma #########
January 28, 2026 AT 12:39I’m a nurse. I’ve held the hand of someone who couldn’t get their heart medication because the batch was recalled. I’ve watched a teenager cry because her asthma inhaler was out of stock and the ER said, ‘Try again next week.’
I don’t care about politics.
I don’t care about profit margins.
I care that the person in front of me is still breathing.
And if we have to raise prices a little to make sure that happens?
Then raise them.
But don’t let the people who need it most pay for it.
That’s not a fix.
That’s a betrayal.