Metronidazole Cumulative Dose Calculator
Dose Calculator
Calculate your cumulative dose of metronidazole to check if you're approaching the 42-gram threshold for neuropathy risk.
Results
Enter your treatment details above to see your cumulative dose.
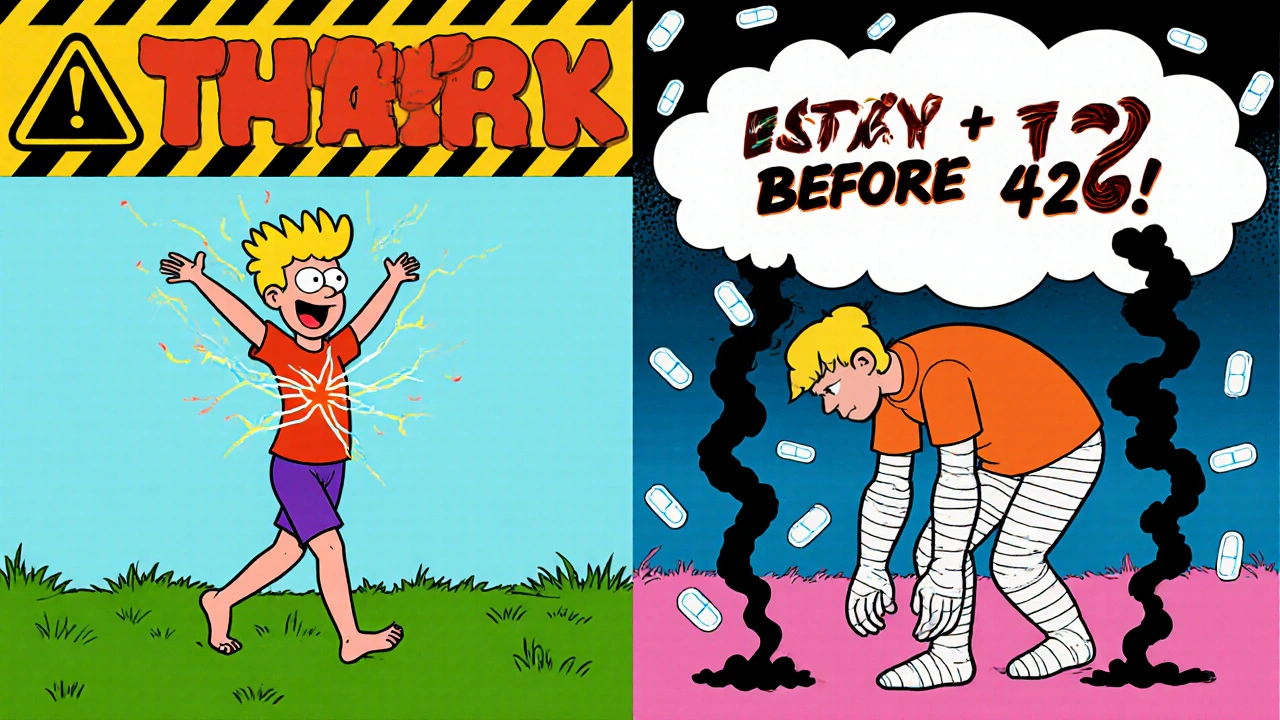
It starts quietly. A tingling in your toes. A dull numbness in your feet that doesn’t go away after a few days. You chalk it up to standing too long, or maybe your shoes are tight. But then it spreads-up your legs, into your hands. Burning. Electric shocks. A feeling like your skin is crawling. And you’re still taking the antibiotic your doctor prescribed.
That’s metronidazole neuropathy. And it’s not rare. It’s just ignored.
Metronidazole, sold under brand names like Flagyl, is one of the most common antibiotics in the world. It’s used for bacterial vaginosis, stomach ulcers caused by H. pylori, C. diff infections, and even dental abscesses. It works. It’s cheap. And for most people, it’s safe-if taken for a week or two. But when treatment stretches beyond 4 to 6 weeks, or the total dose hits 42 grams, the risk of nerve damage spikes dramatically. A 2017 study found patients who took more than 42 grams were over 10 times more likely to develop serious nerve problems than those who stayed under that limit.
What Does Metronidazole Neuropathy Feel Like?
The symptoms don’t come on suddenly. They creep in. First, it’s just a strange sensation-like pins and needles in your toes or fingertips. Then it becomes constant. People describe it as:
- Walking on broken glass
- Feet wrapped in thick, numb socks
- Hands that feel like they’ve fallen asleep for days
- Burning pain that gets worse at night
- Electric shocks shooting up your arms or legs
This isn’t just discomfort. It’s nerve damage. And it follows a pattern: it starts in the feet and hands, then moves upward in what doctors call a “stocking-glove” distribution. That means your fingers and toes go first, then your ankles, wrists, and sometimes even your knees and elbows. It’s symmetric-both sides of your body are affected equally.
Some patients also report trouble with balance, clumsiness, or feeling like their feet don’t belong to them. One case study from Duke University described a teenager who had to soak her legs in ice water just to dull the pain. Another patient, a 52-year-old carpenter, said the tingling in his hands made it impossible to hold tools. He lost his job.
Why Does This Happen?
Metronidazole isn’t just killing bacteria-it’s also interfering with your nerves. The drug crosses into your nervous system easily. Once inside, its chemical structure breaks down into reactive molecules that attack nerve cells. Think of it like rust eating through metal. The nerves swell. Their ability to send signals gets damaged. Sensory nerves go first, which is why numbness and tingling are the earliest signs.
It’s dose-dependent. That means the longer you take it, and the more you take, the higher the risk. A 500mg pill three times a day for 28 days equals 42 grams. That’s the threshold. Past that, your risk jumps from 1.7% to nearly 18%. And it doesn’t matter if you’re young and healthy. Even a 15-year-old on metronidazole for a stubborn infection developed severe neuropathy.
It’s not the same as diabetic neuropathy. It’s not vitamin B12 deficiency. It’s not chemotherapy. This is a direct chemical attack on your nerves by the drug itself. And the damage can be permanent if you wait too long to stop.
How Long Until You Notice Symptoms?
Most people don’t realize they’re at risk until it’s too late. Symptoms usually appear after 4 to 6 months of continuous use. But here’s the catch: some cases have shown up in as little as 10 days-especially if someone is on a high dose for a severe infection like a liver abscess or brain infection.
That’s why many doctors miss it. They assume neuropathy only happens after months. They look for diabetes. They check for arthritis. They think it’s aging. But if you’ve been on metronidazole for more than 3 weeks and you’re feeling odd sensations in your hands or feet, it’s time to ask: could this be the antibiotic?
One Reddit user shared how he was on metronidazole for C. diff prophylaxis for 12 weeks. His feet went numb. He went to three doctors. Two told him it was stress. The third said he was “too young” for neuropathy. He lost six months before someone finally connected the dots. By then, his nerve damage was advanced.

How Is It Diagnosed?
There’s no single blood test for metronidazole neuropathy. Doctors rely on:
- Your history: How long have you been on metronidazole? What’s your total dose?
- Your symptoms: Numbness? Tingling? Burning? Worse at night?
- A neurological exam: Testing reflexes, sensation, muscle strength
- EMG/NCS (nerve conduction studies): These show if the nerves are firing properly. In metronidazole cases, sensory nerves show reduced signals.
The Total Neuropathy Score is a simple questionnaire doctors can use to track changes over time. It asks about pain, numbness, weakness, and how much it affects daily life. Studies show it catches early signs in 89% of cases.
But here’s the problem: most primary care doctors don’t know the 42-gram threshold. A 2023 survey found only 38% could identify it. That’s why so many cases are missed.
What Happens If You Keep Taking It?
Stopping metronidazole is the only proven way to stop the damage. But if you wait too long, your nerves may not recover fully.
Most patients-about 94%-see improvement after stopping the drug. Some feel better in weeks. Others take months. One case took six months before nerve tests returned to normal.
But in 6% of cases, the damage sticks. Permanent numbness. Chronic pain. Trouble walking. Loss of fine motor skills. That’s why timing matters. The longer you wait, the higher the chance of lasting harm.
And it’s not just the nerves. Some patients develop autonomic symptoms-trouble regulating body temperature, sweating abnormally, or feeling dizzy when standing up. One patient had to sit in ice water just to relieve the burning. That’s not normal. That’s your body screaming for help.
What Should You Do If You’re on Metronidazole?
If you’re taking metronidazole for more than 2 weeks, here’s what you need to do:
- Ask your doctor: “What’s my total cumulative dose so far?”
- Calculate it: 500mg three times a day = 1.5g per day. Multiply by the number of days. If you’re over 42g, you’re in the danger zone.
- Check for symptoms: Are your feet or hands numb, tingly, or burning?
- Don’t wait for the pain to get worse. If you notice any new sensations, stop the drug and call your doctor immediately.
- Ask if there’s an alternative. For many infections, other antibiotics like doxycycline, clindamycin, or tinidazole may work just as well-with less nerve risk.
Some hospitals now have electronic alerts that block metronidazole prescriptions past 28 days unless an infectious disease specialist approves it. That’s good. But if your doctor doesn’t use that system, you have to be your own advocate.
Can It Be Reversed?
Yes-mostly. But only if you act fast.
Stopping metronidazole is step one. Step two is physical therapy. Studies show patients who do structured rehab-balance exercises, strength training, sensory retraining-recover 37% faster than those who don’t.
Some doctors now recommend alpha-lipoic acid (600mg daily) during long-term metronidazole use. It’s an antioxidant that may protect nerves. A clinical trial is currently testing this in the U.S. (NCT04876321). Early results look promising.
But don’t wait for a miracle supplement. The best protection is awareness. And early action.
Why Isn’t This Common Knowledge?
Metronidazole is old. It’s cheap. It’s been around since the 1960s. For decades, doctors assumed it was safe. The neuropathy cases were rare. So they were filed away as oddities.
But now we know better. Over 10 million prescriptions are written in the U.S. every year. That’s millions of people at risk. And with antimicrobial stewardship pushing doctors to use narrow-spectrum drugs like metronidazole instead of broad ones, more people are exposed than ever.
The FDA updated its warning label in 2023 to highlight the 42-gram threshold. The Infectious Diseases Society of America now advises against using metronidazole beyond that amount without clear benefit. But that doesn’t mean every doctor knows.
It’s up to you to know.
Final Warning
If you’re on metronidazole and you feel numbness, tingling, or burning in your hands or feet-stop taking it. Call your doctor. Don’t wait. Don’t assume it’s nothing. Don’t let someone tell you you’re too young or it’s just stress.
This isn’t a side effect you can ignore. It’s a warning sign your nerves are being damaged-and you can still fix it, if you act now.
The sooner you stop, the better your chances of full recovery. The longer you wait, the more likely you’ll live with permanent pain.
Metronidazole saves lives. But it can also steal your mobility-if you don’t pay attention.






Sherri Naslund
November 18, 2025 AT 23:50Ashley Miller
November 20, 2025 AT 14:35Lauren Hale
November 22, 2025 AT 06:56Greg Knight
November 22, 2025 AT 14:25rachna jafri
November 23, 2025 AT 03:03darnell hunter
November 24, 2025 AT 20:41Hannah Machiorlete
November 26, 2025 AT 09:36Bette Rivas
November 28, 2025 AT 02:28prasad gali
November 30, 2025 AT 02:15