Ocular Hypertension: Understanding, Managing, and Preventing Vision Loss
When talking about ocular hypertension, a condition where the pressure inside the eye is higher than normal without detectable damage. Also known as high eye pressure, it signals a risk zone that many overlook. The good news is that catching it early lets you take steps before it turns into something more serious.
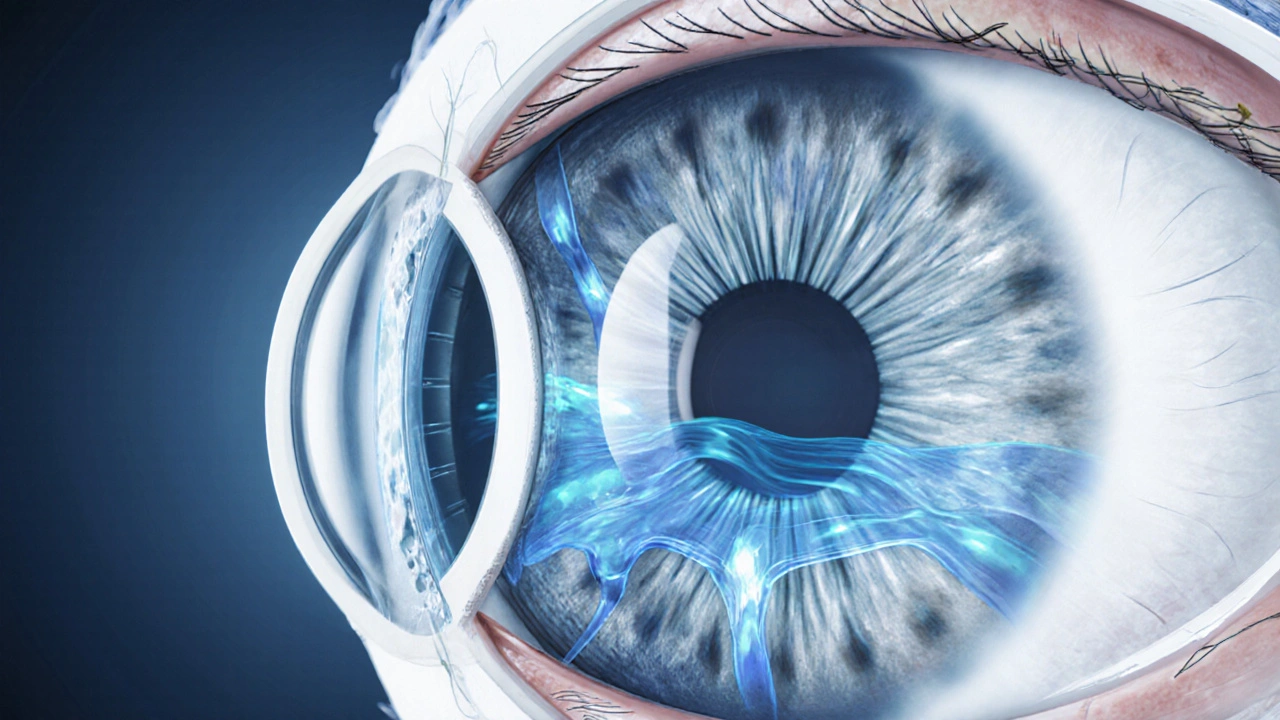
One of the biggest concerns is the link between ocular hypertension and glaucoma, a group of eye diseases that damage the optic nerve and can cause irreversible vision loss. While not every person with high eye pressure develops glaucoma, studies show that untreated ocular hypertension raises the odds dramatically. This relationship means that anyone diagnosed with ocular hypertension should keep a close eye on intraocular pressure, the fluid pressure measured inside the eye, usually in millimeters of mercury (mm Hg). Regular monitoring lets doctors spot creeping rises before they cross the danger threshold.
How Treatment Works and What to Expect
Lowering intraocular pressure is the cornerstone of managing ocular hypertension. The most common class of eye drops does exactly that: prostaglandin analogues. Latanoprost, a once‑daily prostaglandin eye drop that increases outflow of eye fluid is often the first prescription. Clinical data show latanoprost can drop pressure by 25‑30% on average, cutting the chance of progression to glaucoma in half for many patients. If latanoprost doesn’t achieve the target pressure, doctors may add a second agent such as a beta‑blocker or carbonic anhydrase inhibitor.
Medication isn’t the only piece of the puzzle. Lifestyle tweaks help too. Regular aerobic exercise, a balanced diet low in sodium, and staying well‑hydrated can modestly influence eye pressure. Avoiding activities that dramatically increase head‑up pressure—like heavy weight‑lifting or extreme yoga inversions—also helps keep numbers steady. Most importantly, schedule routine visits with your optometrist, eye care professional who can perform pressure checks, visual field tests, and optic nerve imaging. These appointments let you track trends, adjust meds, and address side effects before they become problems.
Understanding the diagnostic process clears up a lot of anxiety. During an eye exam, the doctor uses a tonometer to measure intraocular pressure, often followed by a pachymetry test to gauge corneal thickness—a factor that can affect pressure readings. A quick optic nerve scan, called OCT (optical coherence tomography), shows whether any subtle nerve damage is already present. If the scan reveals early signs, the treatment plan might become more aggressive even if pressure numbers look acceptable.
Insurance coverage and medication cost are real concerns for many. Buying generic versions of prostaglandin drops, where available, can shave off a lot of expense. Some online pharmacies in Australia, for example, offer verified, TGA‑registered options at lower prices. Always check the pharmacy’s credentials, ask for a prescription, and compare a few sources before committing. The savings can be significant, especially if you need a lifetime supply.
Finally, keep an eye on symptoms that could hint at rising pressure: occasional halos around lights, headaches, or a sudden change in vision. These signs don’t replace regular check‑ups but they’re worth reporting right away. Early intervention can prevent permanent damage.
Below you’ll find a curated set of articles that walk you through buying eye‑care meds safely, understanding the role of follow‑up appointments, and exploring related eye‑health topics. Each piece aims to give you actionable insights, whether you’re just diagnosed or have been managing ocular hypertension for years.
Top Causes of High Eye Pressure and How to Prevent Them
Learn the top causes of high eye pressure, from age and genetics to steroids and diet, and discover practical steps to prevent damage and protect your vision.