High Eye Pressure Risk Factor Checker
Your Risk Profile
Select all factors that apply to you to assess your risk for high eye pressure.
Your Risk Assessment
Quick Summary / Key Takeaways
- High eye pressure, also called ocular hypertension, often has no symptoms but can lead to glaucoma.
- Age, genetics, diabetes, steroid eye drops, cataract surgery, and lifestyle choices are the biggest risk factors.
- Regular eye exams, a balanced low‑salt diet, daily exercise, and managing systemic health can keep pressure in check.
- If you use prescription steroid drops, ask your doctor about the lowest effective dose or alternative treatments.
- Early detection and simple lifestyle tweaks can prevent long‑term vision loss.
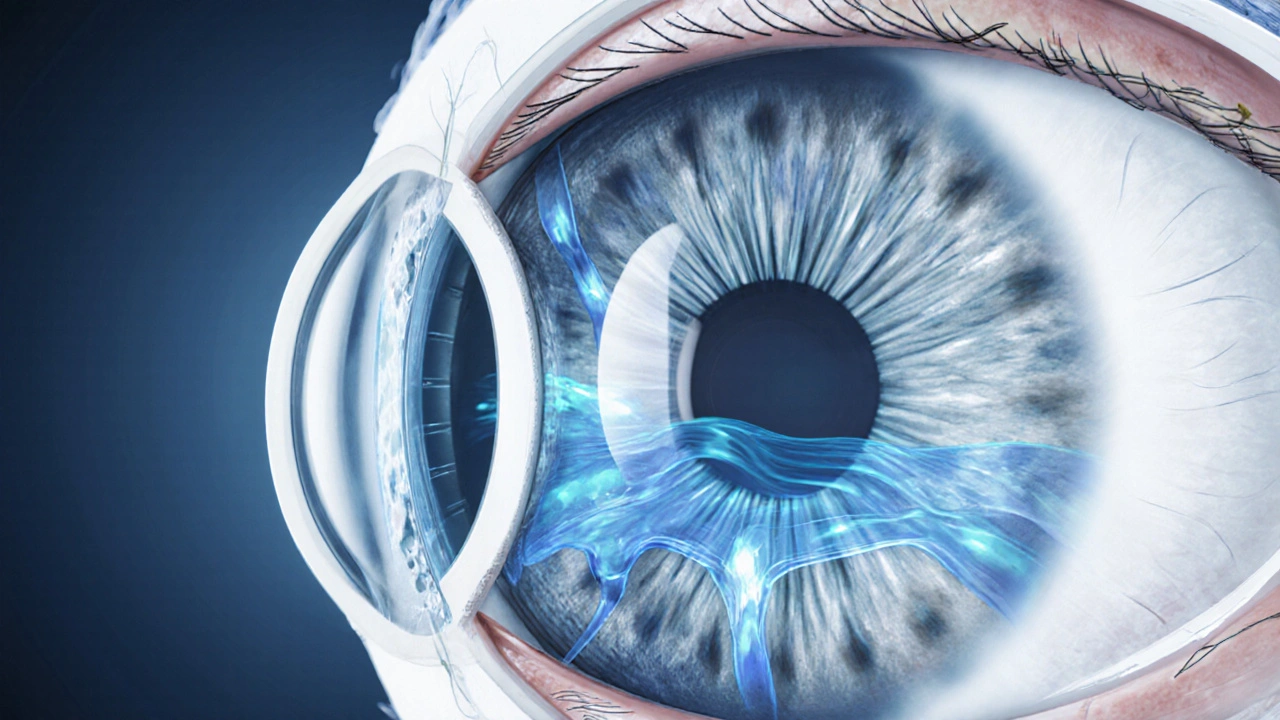
What Is High Eye Pressure?
When fluid builds up inside the eye faster than it can drain, the pressure inside the eyeball rises. This measurement is called high eye pressure (also known as ocular hypertension) - a condition where intraocular pressure exceeds the normal range of 10‑21 mmHg. Unlike many health issues, it rarely causes pain or blurry vision early on, which is why routine checks are crucial.
Why It Matters - The Link to Glaucoma
Persistent pressure damages the optic nerve, the bundle of nerve fibers that carries visual information to the brain. Over time, the nerve fibers thin out, leading to irreversible vision loss. The most common form of this damage is glaucoma a group of eye diseases characterized by progressive loss of optic nerve fibers, often driven by elevated intraocular pressure. Not everyone with high eye pressure develops glaucoma, but the risk increases markedly.

Major Causes of Elevated Intraocular Pressure
Understanding the root causes helps you target prevention. Below are the top contributors, each explained in plain language.
1. Age‑Related Changes
As we get older, the tiny drainage channels (the trabecular meshwork) become less efficient. This natural aging process can push the intraocular pressure the fluid pressure inside the eye, measured in millimeters of mercury (mmHg) upward. Most people notice a gradual rise after age 40.
2. Genetics and Family History
If a close relative has glaucoma or ocular hypertension, your odds of developing high eye pressure rise to about 2‑3 times the general population. Specific genes linked to the structure of the drainage system have been identified, making genetics a powerful predictor.
3. Systemic Health - Diabetes and Hypertension
Both diabetes a chronic condition characterized by high blood sugar levels that can affect blood vessels throughout the body and high blood pressure impact the tiny vessels in the eye. Poor glucose control thickens the lens and can obstruct fluid flow, while systemic hypertension elevates overall vascular pressure, both contributing to higher ocular pressure.
4. Steroid Eye Drops
Prescription steroid drops are essential for treating inflammation after eye surgery or severe allergies. However, they can cause a sudden spike in pressure, especially with prolonged use. Even short courses may affect people who are already prone.
5. Eye Injuries or Inflammation
Trauma, infections, or chronic inflammatory conditions (like uveitis) can scar or swell the drainage pathways, leading to pressure buildup.
6. Cataract Surgery (Post‑Operative)
Modern phacoemulsification is safe, but a small percentage of patients develop pressure spikes weeks after the procedure. Residual lens material or inflammation are typical culprits.
7. Lifestyle Factors - Diet, Caffeine, and Exercise
High‑salt diets increase fluid retention, which can subtly raise eye pressure. Excessive caffeine (more than 300 mg per day) triggers a temporary pressure rise. Conversely, regular aerobic exercise improves fluid outflow and can lower pressure by a few mmHg.
How to Prevent High Eye Pressure
Prevention blends medical monitoring with everyday habits. Here’s a roadmap you can follow.
1. Schedule Regular Eye Exams
Even if you feel fine, get a comprehensive check‑up every 1‑2 years after age 40, or annually if you have risk factors. An optometrist will measure your intraocular pressure using a painless tonometer.
2. Adopt a Low‑Salt, Nutrient‑Rich Diet
Aim for less than 2,300mg of sodium daily. Foods high in omega‑3 fatty acids (salmon, walnuts) support vascular health, while leafy greens provide antioxidants that protect the optic nerve.
3. Stay Physically Active
At least 150 minutes of moderate aerobic exercise each week (brisk walking, cycling, swimming) can lower pressure by 1‑3mmHg on average.
4. Manage Systemic Conditions
Keep blood sugar and blood pressure under doctor‑supervised targets. Lifestyle changes, medication adherence, and regular monitoring are key.
5. Use Steroid Drops Wisely
If you’re prescribed steroids, follow the shortest duration possible and ask about non‑steroidal alternatives for allergies or inflammation.
6. Protect Your Eyes
Wear safety goggles during sports or high‑impact work. This reduces the chance of trauma‑related pressure spikes.
7. Limit Caffeine and Alcohol
Moderate caffeine to one cup of coffee per day and keep alcohol intake within recommended limits (no more than two standard drinks daily).
Quick Prevention Checklist
- Book an eye exam-once a year after age40 or as advised.
- Check sodium intake-read labels, aim for <2,300mg.
- Exercise-150min/week moderate cardio.
- Monitor blood sugar & blood pressure-use home devices, keep records.
- Ask your eye doctor about steroid alternatives if you need long‑term drops.
- Wear protective eyewear when needed.
- Limit caffeine to ≤300mg per day.

Causes vs. Prevention Strategies
| Cause | How It Raises Pressure | Prevention / Management |
|---|---|---|
| Age‑related drainage loss | Trabecular meshwork becomes less permeable | Regular tonometry checks; aerobic exercise to boost outflow |
| Genetic predisposition | Inherited structural quirks in drainage pathways | Early screening for family members; monitor pressure more frequently |
| Diabetes / systemic hypertension | Vascular changes obstruct fluid channels | Maintain HbA1c<7%; keep BP<130/80mmHg |
| Steroid eye drops | Inflammatory response narrows outflow | Use lowest effective dose; discuss non‑steroidal options |
| High‑salt diet & excess caffeine | Increases fluid retention & transient pressure spikes | Limit sodium to 2,300mg; cap caffeine at 300mg |
| Post‑cataract surgery inflammation | Residual lens debris or swelling blocks drainage | Follow post‑op regimen; attend follow‑up IOP checks |
| Eye trauma or chronic inflammation | Scar tissue forms in the trabecular meshwork | Wear protective eyewear; treat inflammation promptly |
Frequently Asked Questions
Can I have high eye pressure without any symptoms?
Yes. Most people notice nothing until an eye exam reveals elevated intraocular pressure. That’s why regular checks are essential, especially after age 40.
How often should I get my eye pressure checked?
If you’re under 40 and have no risk factors, every 2‑3years is fine. Once you’re 40 or have a family history, aim for at least once a year.
Do over‑the‑counter eye drops raise pressure?
Most OTC lubricating drops are safe. Only steroid‑based drops, even some prescription allergy drops, have a known risk of increasing pressure.
Can lifestyle changes actually lower my eye pressure?
Studies show regular aerobic exercise can drop pressure by 1‑3mmHg, and reducing salt intake can have a modest but consistent effect. These changes are most effective when combined with medical monitoring.
Is high eye pressure the same as glaucoma?
No. High eye pressure (ocular hypertension) is a risk factor. Glaucoma is the actual damage to the optic nerve that may result from sustained pressure.
My doctor prescribed steroid drops after eye surgery. What should I watch for?
Schedule a follow‑up IOP check within a week of starting the drops. If pressure rises above 21mmHg, discuss tapering the steroid or switching to a non‑steroidal anti‑inflammatory.
Can I self‑monitor my eye pressure at home?
Home tonometers exist but are expensive and require training. Most people rely on professional exams for accurate readings.
Next Steps & Troubleshooting
If you’ve discovered elevated pressure during a recent exam, don’t panic. First, ask your eye doctor about the exact mmHg reading and whether it’s borderline or clearly high. Then:
- Schedule a follow‑up within 4‑6 weeks to confirm the measurement.
- Review any medications you’re using - especially steroid eye drops or systemic steroids.
- Start the lifestyle checklist above: cut down salt, add a daily walk, and track blood sugar/BP.
- If pressure stays above 21mmHg, discuss treatment options such as prescription eye drops that improve fluid drainage.
- Keep a written log of your readings, diet, and exercise - it helps the doctor see trends.
Remember, early action can keep your vision sharp for decades.



Sharon Bruce
October 5, 2025 AT 17:04Patriotic eye health matters! 🇺🇸
True Bryant
October 15, 2025 AT 14:03When you dive into intraocular pressure, the biomechanical stress on the trabecular meshwork is a textbook case of fluid dynamics gone rogue. It's not just aging; systemic hypertension and corticosteroid exposure are notorious culprits that hijack ocular homeostasis. The literature is replete with meta‑analyses proving that high‑salt diets exacerbate aqueous humor retention, especially in genetically predisposed cohorts. So, if you're sidestepping risk, start by auditing your caffeine intake and that daily dose of steroid eye drops.
Danielle Greco
October 25, 2025 AT 11:02Honestly, the risk checker is a fun way to spot those sneaky factors that slip through daily habits. 👀 If you’ve got a family history, that’s a red flag, but lifestyle tweaks like cutting back on salty snacks can make a real difference. Also, staying active keeps blood pressure in check, which indirectly supports eye pressure. Keep an eye on those check‑boxes and schedule that yearly exam! 😊
Andy Lombardozzi
November 4, 2025 AT 07:01Yo, folks! High eye pressure isn’t something to shrug off – it’s a wake‑up call. Stay on top of your blood pressure numbers, swap that sugary coffee for green tea, and don’t forget regular eye check‑ups. Small changes pile up, and your eyes will thank you. Let’s keep those numbers low and vision sharp!
Joshua Ardoin
November 14, 2025 AT 04:00Hey everyone, just wanted to add a friendly reminder that a balanced diet and regular exercise can really help keep eye pressure in check. 🌿 Hydration matters too – try to drink plenty of water throughout the day. And if you’re on any meds, talk to your doctor about possible eye‑related side effects. Stay healthy and keep those eyes happy! 😊
Glenn Gould
November 24, 2025 AT 00:59Yo Josh, good vibes! just sayin’ i think ur tipz r solid but maybe cut the caffeine a lil more. also, dont forget to get those eye tests every year – they r super important. stay lit!
Poonam Sharma
December 3, 2025 AT 21:58Listen up, comrades! The intersection of genetics and lifestyle in ocular hypertension is a battlefield where only the well‑armed survive. If you hail from a lineage plagued by glaucoma, you must adopt a regimented regimen: low‑sodium meals, limited caffeine, and rigorous monitoring of systemic blood pressure. Any deviation is tantamount to surrendering to an avoidable affliction. This is not a suggestion; it is a patriotic duty to preserve our nation’s visual acuity!
Meigan Chiu
December 13, 2025 AT 18:57While the previous comment paints a dramatic portrait, let us ground the discussion in precise terminology. The correlation between high‑salt intake and intraocular pressure is supported by modest epidemiological data, not the sweeping generalizations presented earlier. Moreover, the use of "commander" rhetoric obscures the nuanced role of genetics versus modifiable risk factors. A balanced perspective acknowledges that while dietary sodium may contribute, it is not the sole determinant. Therefore, claims of "patriotic duty" are hyperbolic at best.
Patricia Hicks
December 23, 2025 AT 15:56What a wonderful opportunity to reflect on how we can collectively nurture our ocular health! First, let us acknowledge that the eye is a marvel of biological engineering, deserving of our utmost care. We can start by incorporating a diet rich in antioxidants-think leafy greens, vibrant berries, and omega‑3 fatty acids found in fish-to protect the delicate retinal tissue. Second, regular physical activity not only supports cardiovascular health but also promotes optimal blood flow to the optic nerve, thereby mitigating pressure spikes. Third, maintaining a realistic caffeine intake-ideally under 300 milligrams per day-can prevent unnecessary stimulation of the ciliary body, which produces aqueous humor. Fourth, anyone using steroid eye drops should consult their ophthalmologist about the safest duration and dosage to avoid iatrogenic pressure elevation. Fifth, reducing stress through mindfulness or yoga can have a subtle yet meaningful impact on intraocular pressure, as stress hormones can influence fluid dynamics in the eye. Sixth, never underestimate the power of routine eye examinations; early detection remains the cornerstone of preventing glaucoma progression. Seventh, safeguarding your eyes from injury by wearing protective eyewear during sports or hazardous activities is essential. Eighth, quitting smoking not only benefits lung function but also improves overall vascular health, indirectly supporting eye health. Ninth, stay vigilant about systemic conditions such as hypertension and diabetes, as these comorbidities often intertwine with ocular pressure regulation. Tenth, keep your eyes well‑lubricated with appropriate artificial tears if you experience dryness, because a comfortable ocular surface contributes to overall eye health. Eleventh, limiting exposure to excessive screen time and ensuring proper lighting can reduce eye strain, which, while not directly linked to pressure, promotes overall comfort. Twelfth, drinking sufficient water throughout the day helps maintain proper fluid balance, yet avoid excessive consumption in a short period. Thirteenth, educate yourself and your loved ones about the signs of glaucoma-such as peripheral vision loss-so that you can act swiftly if symptoms arise. Fourteenth, share this knowledge with your community; collective awareness is a powerful tool in the fight against vision loss. Finally, remember that caring for your eyes is an act of self‑respect and an investment in your future experiences, from reading beloved books to watching sunsets. Let’s embrace these habits with optimism and gratitude, fostering a generation of vibrant sight!
Quiana Huff
January 2, 2026 AT 12:55Thanks for the thorough guide, Patricia! 🙌 I’ll start adding more greens to my meals and schedule that eye check‑up. Also, I appreciate the reminder about caffeine limits. 😊
William Nonnemacher
January 12, 2026 AT 09:54High eye pressure is a clear indicator of systemic dysregulation. Reduce sodium avoid steroids limit caffeine. Regular exams are non‑negotiable.
Alex Ramos
January 22, 2026 AT 06:53Indeed, the correlation between dietary sodium and intra‑ocular tension is well‑documented; consequently, individuals should consider adopting a low‑salt regimen, especially when coupled with regular ophthalmologic assessments, which, as research consistently demonstrates, are essential for early detection and intervention.
mauricio gonzalez martinez
February 1, 2026 AT 03:52Just a quiet reminder that staying consistent with routine eye exams can catch issues early. It's a simple habit that goes a long way.
Jackie Felipe
February 11, 2026 AT 00:51Thnks for the tip – I’ll add an eye check‑up to my calender. Sorry about any typos, my spellig isn’t perfect.
debashis chakravarty
February 20, 2026 AT 21:50From a clinical standpoint, it is imperative to note that sustained intraocular pressure elevation constitutes a primary risk factor for glaucomatous optic neuropathy; therefore, adherence to evidence‑based preventive measures, including dietary moderation and vigilant monitoring, should be universally advocated.