Nasal Decongestants: What They Are, How They Work, and When to Avoid Them
When your nose is stuffed up, nasal decongestants, medications that shrink swollen blood vessels in the nasal passages to open airways. Also known as decongestant sprays, they’re one of the most common OTC remedies for colds and allergies. But what feels like a quick fix can turn into a long-term problem if you use them for more than three days. That’s because these sprays don’t treat the cause—they just temporarily silence the symptoms. And when they wear off, your nose often swells back even worse. This cycle is called rebound congestion, a condition where the nasal passages become dependent on the spray to stay clear. Doctors call it rhinitis medicamentosa, a drug-induced inflammation caused by overusing nasal decongestants. It’s not rare—it’s surprisingly common, and most people don’t realize they’re stuck in it until they can’t breathe without the spray.
Why does this happen? Nasal decongestants work by tightening blood vessels. That reduces swelling and lets you breathe. But your body adapts. Over time, the vessels become less responsive, so you need more spray to get the same result. Then, when you stop, the vessels dilate hard, causing even more swelling than before. It’s like turning up the volume on a speaker until it blows out. And once you’re in this cycle, quitting isn’t easy. Cold turkey can mean days of severe congestion, headaches, and even trouble sleeping. That’s why breaking the habit often needs a plan—like switching to saline rinses, using a steroid spray under a doctor’s care, or gradually reducing use instead of stopping all at once.
Not everyone who uses nasal decongestants ends up with rebound congestion, but the risk goes up fast after day three. People with chronic allergies, sinus issues, or those who use them daily for months are especially vulnerable. And it’s not just sprays—oral decongestants like pseudoephedrine carry their own risks, like high blood pressure and insomnia. What’s worse, many don’t realize they’re using multiple products that contain the same active ingredient. A cold medicine, a sinus tablet, and a nasal spray might all have phenylephrine or oxymetazoline. You could be overdosing without knowing it.
There are better ways to manage congestion long-term. Saline sprays hydrate without dependency. Humidifiers help thin mucus. Antihistamines work better for allergy-related stuffiness. And if your congestion won’t quit, it might not be allergies at all—it could be a deviated septum, polyps, or even a reaction to another medication. The posts below cover exactly these scenarios: how to recognize when your nasal spray is causing more harm than good, what to do when you’re stuck in the cycle, and how to find relief without going back to the bottle. You’ll find real stories, medical insights, and practical steps that actually work—not just quick fixes that promise the world but deliver nothing but more congestion.
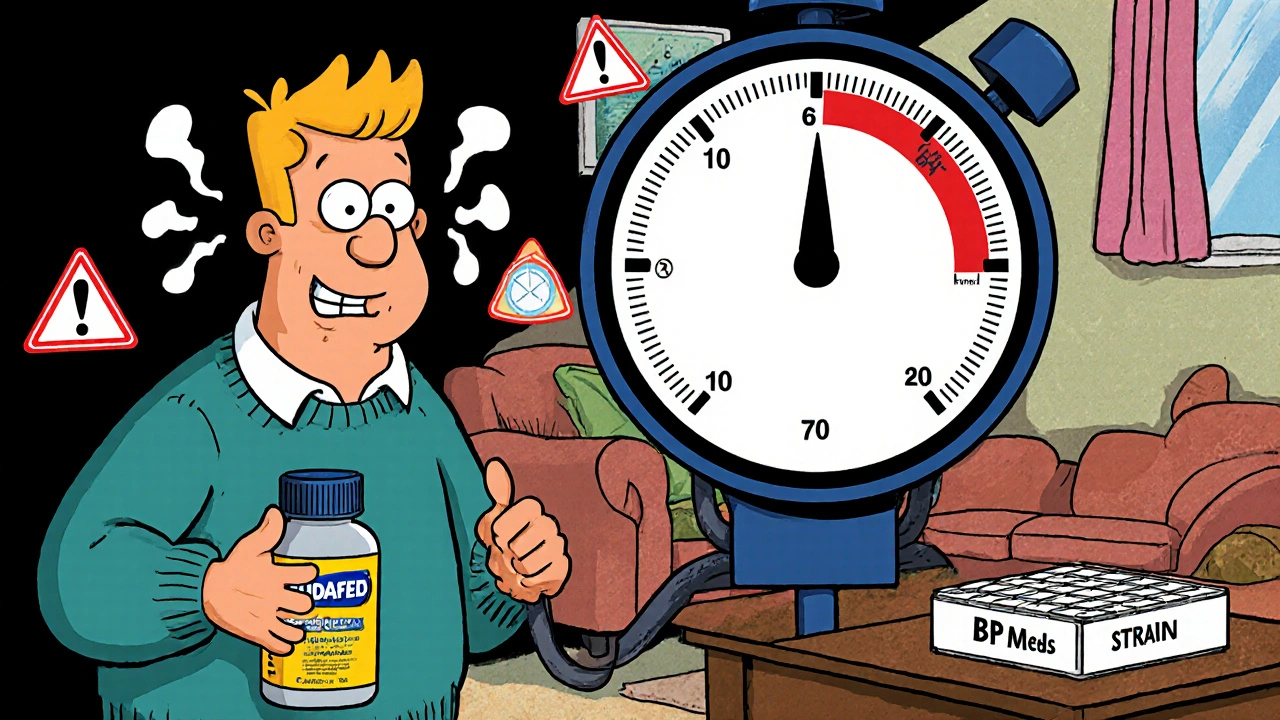
Nasal Decongestants and Blood Pressure Medications: What You Need to Know for Safe Use
Nasal decongestants can dangerously raise blood pressure, especially when taken with hypertension medications. Learn which ingredients to avoid, safe alternatives, and how to protect your heart when you have a cold.