Multiple Sclerosis: Causes, Treatments, and Medication Management
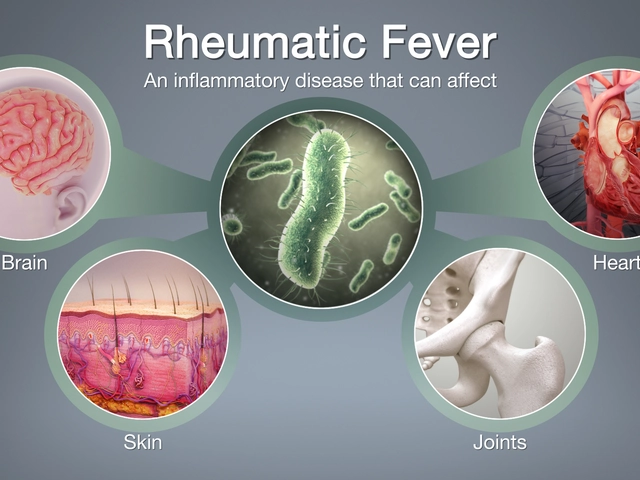
When you have multiple sclerosis, a chronic autoimmune condition where the immune system attacks the protective covering of nerves. Also known as MS, it disrupts signals between your brain and body, leading to fatigue, muscle weakness, vision problems, and sometimes loss of balance or coordination. Unlike temporary nerve issues, MS is lifelong—but it doesn’t have to control your life. Many people manage it well with the right mix of medication, lifestyle changes, and monitoring.
The brain and spinal cord damage from MS happens slowly, often in waves. That’s why disease-modifying therapies, medications designed to reduce flare-ups and slow progression are so important. Drugs like interferons, glatiramer acetate, and newer oral options such as fingolimod or dimethyl fumarate help calm the immune system’s attack. But they’re not risk-free. Some can lower white blood cell counts, raise liver enzymes, or increase infection risk. That’s why regular blood tests and doctor visits aren’t optional—they’re part of staying in control.
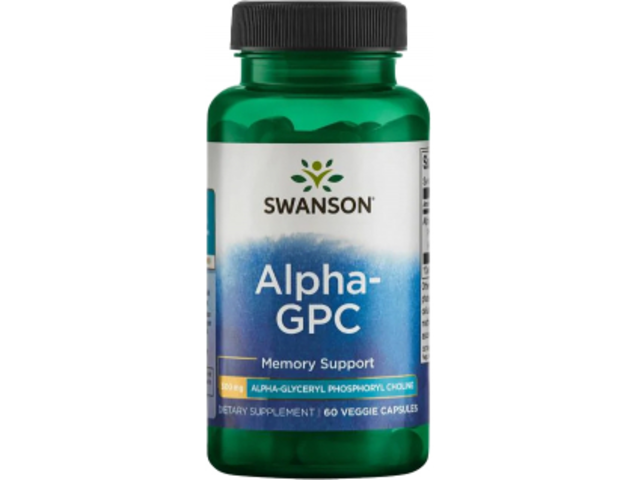
Side effects from MS meds can be just as frustrating as the disease itself. Nausea, flu-like symptoms, or sudden dizziness might make you want to quit. But stopping without guidance can lead to worse flare-ups. And here’s something most people don’t talk about: some MS treatments interact with common drugs like painkillers, antibiotics, or even herbal teas. For example, if you’re on an immunosuppressant and take high-dose vitamin D or turmeric supplements, you could be accidentally weakening your body’s defenses. It’s not about avoiding supplements—it’s about knowing what’s safe with your specific regimen.
Many with MS also deal with secondary issues like bladder problems, muscle stiffness, or depression. These aren’t just side effects—they’re part of the full picture. That’s why treatments often involve more than one drug. You might take a muscle relaxant for spasms, an antidepressant for mood, and a diuretic for fluid retention—all at the same time. That’s polypharmacy, using multiple medications at once, common in chronic conditions. It works—but only if you track everything. Missing a dose, mixing up pills, or not telling your doctor about an OTC painkiller can cause serious problems. A simple shared calendar or pill organizer isn’t just helpful—it’s essential.
There’s no cure yet, but research keeps moving forward. New drugs are being tested every year, and many people find relief through physical therapy, diet tweaks, or stress management. Yoga and meditation, for instance, aren’t just wellness trends—they’ve been shown to help with fatigue and mental clarity in MS patients. The key is finding what works for you, without letting fear or misinformation steer you wrong.
What you’ll find below are real, practical guides written for people living with MS—not doctors or researchers. You’ll read about how to spot early signs of nerve damage from meds, how to switch treatments safely, what to do when side effects hit hard, and how to avoid dangerous drug interactions. These aren’t theoretical articles. They’re based on what people actually experience—and what works when you’re trying to stay healthy, not just survive.
How Amantadine Helps Manage Multiple Sclerosis Symptoms
Amantadine helps manage MS-related fatigue by boosting brain chemicals involved in energy and alertness. It’s not a cure, but many people find it improves daily function with fewer side effects than stronger stimulants.