Glucose-Lowering Drugs: What Works, What to Avoid, and How to Choose
When your body struggles to manage blood sugar, glucose-lowering drugs, medications designed to reduce high blood sugar levels in people with type 2 diabetes. Also known as antihyperglycemic agents, they’re not one-size-fits-all—what helps one person might do little for another. These drugs don’t cure diabetes, but they help you stay in control, reduce long-term risks like nerve damage or kidney issues, and give you more energy day to day.
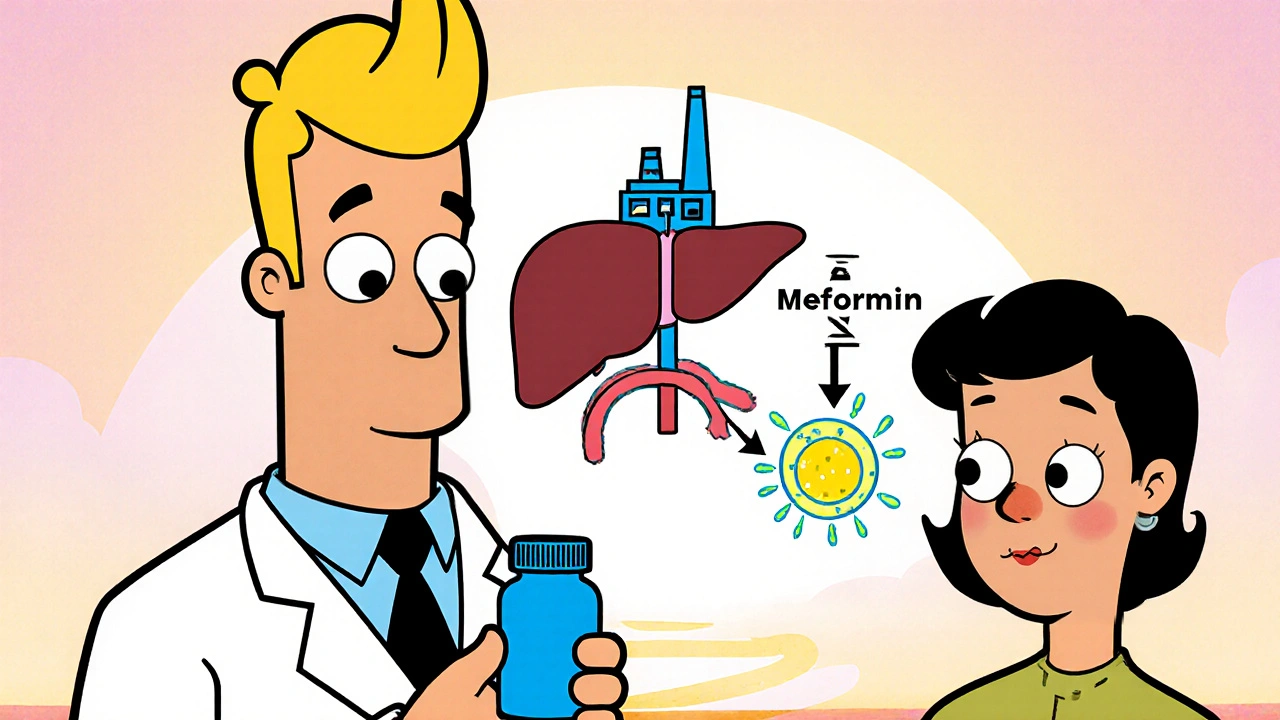
There are several main types, each with a different job. Metformin, the most common first-choice drug, works by making your liver produce less sugar and helping your muscles use insulin better. It’s usually well-tolerated, doesn’t cause weight gain, and is cheap. Then there’s sulfonylureas, older drugs that push your pancreas to release more insulin. They work fast but can drop your blood sugar too low and may lead to weight gain. Insulin, a hormone your body should make naturally, is used when other drugs aren’t enough. It’s powerful but requires careful dosing and frequent monitoring. Newer options like SGLT2 inhibitors and GLP-1 agonists help your kidneys flush out sugar or slow digestion, and some even protect your heart.
Choosing the right one isn’t just about what’s on the list—it’s about your weight, kidney function, risk of low blood sugar, cost, and even how many pills you’re willing to take. Some drugs help you lose weight, others don’t. Some need daily shots, others are pills. Some cost a few dollars a month, others hundreds. Your doctor won’t just pick one—they’ll test, adjust, and sometimes try two or three before finding the fit.
What you’ll find here aren’t just drug names. You’ll see real comparisons: how metformin stacks up against newer options, why some people switch from sulfonylureas, what to watch for with insulin, and how lifestyle changes can make these drugs work better. No fluff. No marketing. Just what works, what doesn’t, and what you need to ask your doctor next time you’re in the office.
Metformin vs Alternative Diabetes Medications: Pros, Cons & When to Switch
Compare Metformin with popular diabetes drug alternatives, weighing efficacy, side effects, cost, and when a switch makes sense for type 2 diabetes management.





