Diabetes Medication Decision Tool
Your Health Profile
Recommendations
Metformin has been the go‑to first‑line treatment for type 2 diabetes for decades, but a growing toolbox of newer agents means many patients wonder if switching could help them reach their goals faster. This guide walks through the most common alternatives, compares them on key criteria, and shows how to decide which pill-or injection-fits your lifestyle and health profile.
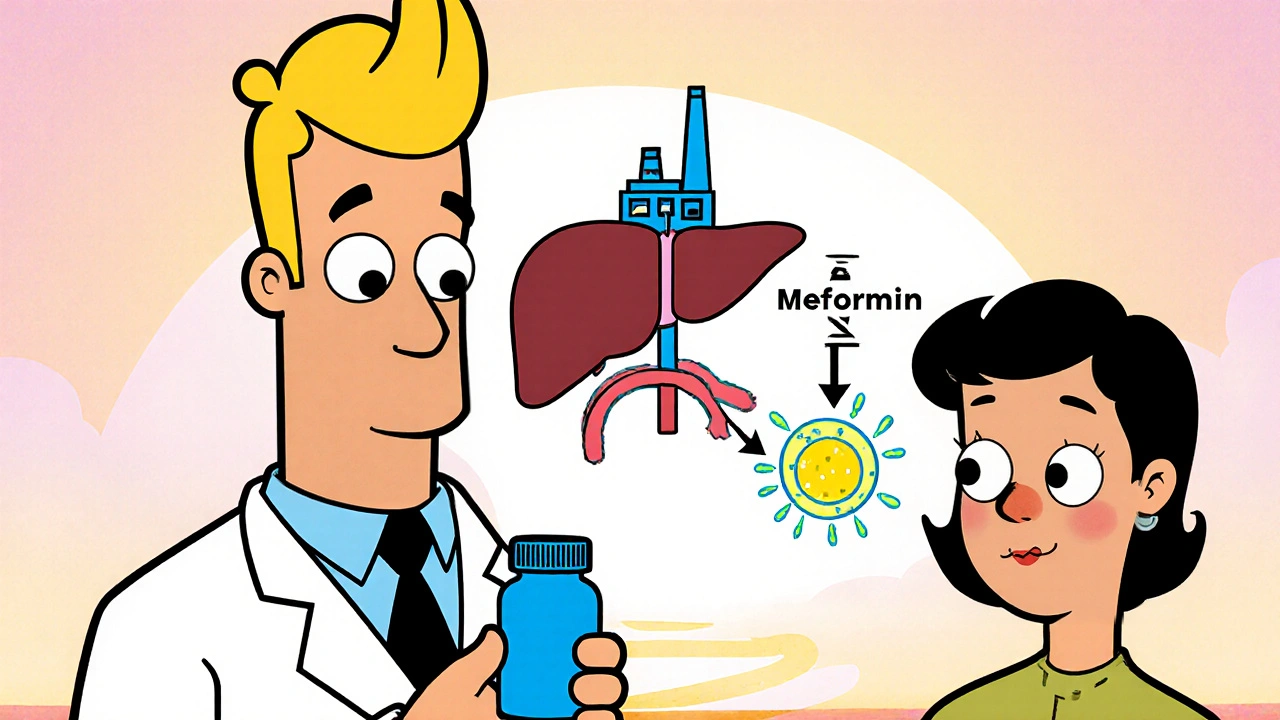
How Metformin Works
When you first hear about Metformin is an oral biguanide that reduces hepatic glucose output and improves peripheral insulin sensitivity, the science sounds complex, but the bottom line is simple: it helps your body use the sugar already in circulation more efficiently. It’s taken once or twice a day, costs a few dollars a month, and doesn’t usually cause weight gain. Common side effects are stomach‑related-nausea, diarrhea, or a metallic taste-often easing after a few weeks.
Why Look at Alternatives?
Even though Metformin works for most people, several scenarios push clinicians to consider other drugs:
- Inadequate HbA1c reduction after 3-6 months.
- Gastrointestinal intolerance that doesn’t improve with dose titration.
- Renal function that drops below the safety threshold (eGFR <30mL/min/1.73m²).
- Need for weight loss, cardiovascular protection, or low hypoglycaemia risk.
When any of these flags appear, the American Diabetes Association (ADA) recommends evaluating newer classes such as DPP‑4 inhibitors, GLP‑1 receptor agonists, SGLT2 inhibitors, or even moving to insulin.
Overview of Common Alternatives
Below is a quick snapshot of the most frequently prescribed alternatives, grouped by drug class.
- Sitagliptin - a DPP‑4 inhibitor that boosts endogenous GLP‑1 levels.
- GLP‑1 receptor agonists - injectable agents (e.g., Semaglutide) that mimic the gut hormone GLP‑1.
- Sulfonylureas - older oral agents (e.g., Glipizide) that stimulate insulin release.
- Insulin - injectable therapy ranging from rapid‑acting to long‑acting basal formulations.
- Thiazolidinediones - oral agents like Pioglitazone that improve insulin sensitivity through PPAR‑γ activation.
Key Comparison Criteria
To make an informed switch, weigh each drug against these five pillars:
- Glycaemic efficacy (average HbA1c drop).
- Weight impact (gain, neutrality, or loss).
- Risk of hypoglycaemia.
- Side‑effect profile.
- Cost and insurance coverage.
Side‑by‑Side Comparison Table
| Drug | Mechanism | Typical HbA1c ↓ (% | Weight Effect | Major Side Effects | Cost (US$/month) | Renal Safety |
|---|---|---|---|---|---|---|
| Metformin | Reduces hepatic gluconeogenesis | 0.8-1.5 | Neutral to modest loss | GI upset, lactic acidosis (rare) | 5‑10 | Safe >30mL/min, avoid <30 |
| Sitagliptin (DPP‑4) | Inhibits DPP‑4, ↑ GLP‑1 | 0.5-0.8 | Weight neutral | URIs, nasopharyngitis | 150‑200 | Safe down to 30mL/min |
| GLP‑1 agonist (Semaglutide) | GLP‑1 receptor activation | 1.0-1.5 | 3‑5kg loss | Nausea, vomiting, pancreatitis risk | 900‑1200 | Safe >30mL/min, dose‑adjust if lower |
| Sulfonylurea (Glipizide) | Stimulates pancreatic β‑cells | 0.8-1.2 | Weight gain | Hypoglycaemia, skin rash | 30‑50 | Use with caution, monitor |
| Insulin (Basal glargine) | Exogenous insulin replacement | 1.5-2.5 | Weight gain | Hypoglycaemia, injection site issues | 150‑250 | Not contraindicated; dose adjust |
Deep Dive into Each Alternative
Sitagliptin (DPP‑4 Inhibitor)
Sitagliptin works quietly-by preventing the breakdown of the hormone GLP‑1, it modestly improves post‑meal glucose control without causing weight gain. Its safety profile is appealing for older adults and those with mild renal impairment. However, the HbA1c reduction is modest, and the cost can be a barrier unless covered by insurance.
GLP‑1 Receptor Agonists
Injectable GLP‑1 agonists such as Semaglutide or Dulaglutide have reshaped the treatment landscape. They deliver the biggest weight loss of any diabetes drug and also lower cardiovascular risk, as confirmed by several FDA-approved trials. The downside? Injections, gastrointestinal side effects, and a premium price tag.
Sulfonylureas
Glipizide and its cousins are cheap and effective at dropping blood sugar quickly, but they force the pancreas to release more insulin, raising the chance of hypoglycaemia, especially in the elderly. They also tend to cause weight gain, which is a concern for patients already battling obesity.
Insulin Therapy
When oral agents no longer suffice, basal insulin (e.g., glargine) provides the most potent glucose‑lowering effect. It’s indispensable for people with very high HbA1c or significant beta‑cell failure. The trade‑off is daily injections and a notable risk of hypoglycaemia if doses aren’t carefully titrated.
Thiazolidinediones (Pioglitazone)
Pioglitazone improves insulin sensitivity in muscle and fat, similar to Metformin’s end‑goal but via a different pathway. It’s useful when Metformin isn’t tolerated and can reduce cardiovascular events. Yet, it’s linked to weight gain, fluid retention, and a small increase in heart‑failure risk.
Decision Guide: When to Switch from Metformin
Use the following checklist to see if a switch makes sense:
- Current HbA1c >7.5% after 3‑6months of maximally tolerated Metformin.
- Persistent GI side effects despite gradual dose escalation.
- eGFR falls below 45mL/min/1.73m².
- Desire for weight loss or cardiovascular risk reduction.
- Insurance formulary limits Metformin coverage but favors newer agents.
If you tick one or more boxes, discuss alternatives with your endocrinologist. Often, a combination (e.g., Metformin + GLP‑1 agonist) yields the best balance of efficacy, weight control, and tolerability.
Practical Tips for Starting an Alternative
- Start Low, Go Slow: For GLP‑1 agonists, begin with a weekly low dose to tame nausea.
- Monitor Renal Function: Re‑check eGFR 1-2months after initiating Sitagliptin or Metformin.
- Watch for Hypoglycaemia: If you add a sulfonylurea, halve the dose when combined with insulin.
- Track Weight: Record weekly weight changes; many patients see the biggest drop within the first 12weeks of GLP‑1 therapy.
- Insurance Check: Call your pharmacy benefits manager to confirm prior‑authorisation requirements for expensive agents.
Bottom Line
Metformin remains a solid foundation for most type 2 diabetes patients, thanks to its low cost, safety, and modest weight benefit. Yet, the expanding armamentarium means you’re not forced to stay on one pill forever. By comparing efficacy, side effects, cost, and personal health goals, you can pick an alternative that aligns with your lifestyle-whether that’s a once‑weekly injection that sheds pounds or an inexpensive oral combo that keeps glucose steady without extra hassle.
Frequently Asked Questions
Can I combine Metformin with a GLP‑1 agonist?
Yes. The ADA recommends adding a GLP‑1 agonist to Metformin when additional HbA1c reduction, weight loss, or cardiovascular protection is needed. The combination often yields a 1-2% drop in HbA1c without increasing hypoglycaemia risk.
What’s the biggest downside of sulfonylureas?
Their propensity to cause low blood sugar, especially in older adults or those with irregular meals. They also tend to promote weight gain, which can counteract diabetes management goals.
Is insulin only for late‑stage diabetes?
Not at all. Some patients start basal insulin early if their HbA1c is very high or they have contraindications to oral drugs. Early insulin can preserve beta‑cell function in certain cases.
How does kidney health affect drug choice?
Metformin and most GLP‑1 agonists require dose adjustments when eGFR falls below 45mL/min. Sitagliptin stays safe down to 30mL/min, while sulfonylureas need caution because reduced clearance raises hypoglycaemia risk.
Which drug offers the best cardiovascular benefit?
GLP‑1 receptor agonists (e.g., Semaglutide, Dulaglutide) have demonstrated a 10‑15% reduction in major adverse cardiovascular events in large trials, outpacing most other classes.






Rohit Sridhar
October 17, 2025 AT 21:56Hey folks, great rundown on the Metformin landscape! I love how you broke down each class with simple pros and cons – it makes the whole decision feel less intimidating. If you’re still on Metformin and curious about a switch, start by checking your latest HbA1c and kidney numbers – that’s the real compass. Remember, even a modest weight loss from a GLP‑1 agonist can boost insulin sensitivity across the board. Keep the conversation open with your doctor; a collaborative tweak often yields the best results.
Stay motivated and keep tracking those numbers!
Bethany Torkelson
October 24, 2025 AT 03:56Your vague optimism is nothing but a sugar‑coated excuse for ignoring real risks.
Avril Harrison
October 30, 2025 AT 08:56Interesting read, especially the cultural shift towards injectable GLP‑1s – it’s like watching old‑school tea parties turn into high‑tech coffee meetups. The plain‑language tables helped me visualise the trade‑offs without drowning in jargon. I appreciate the nod to renal function; many guides skim over that. For anyone juggling work and meds, the “Start Low, Go Slow” tip is pure gold. Cheers for making a complex topic feel like a chat over a cuppa.
Natala Storczyk
November 5, 2025 AT 14:56Wow!!! This article just lit a fire under my diabetes management!!! The way you laid out the pros and cons is downright theatrical – bravo!!! I can’t believe how many people still think Metformin is the only hero!!! The injection hype is real, and the cardiovascular benefits? Absolutely mind‑blowing!!! Keep the drama alive, because battling sugar needs a stage!!!
Barbara Grzegorzewska
November 11, 2025 AT 20:56Honestly, this piece reads like a textbook written by a robot. The author totally ignores the nuanced pharmacodynamics that seasoned clinicians cherish. Metformin’s mechanism, albeit simple, is elegantly superior to the flash‑in‑the‑pan GLP‑1 hype. And let’s not forget the cost – you can’t afford those pricey injectables unless you’re rolling in cash. The author definitely needs to up their game, cuz this is basic 101 stuff.
Nis Hansen
November 18, 2025 AT 02:56While I respect the desire for depth, it's essential to balance academic rigor with patient accessibility. The pharmacodynamic details you mention are indeed fascinating, yet the average reader benefits from clear, actionable guidance. Moreover, cost considerations are not merely frivolous; they shape adherence patterns dramatically. In practice, a tiered approach-starting with Metformin, then evaluating cardiovascular risk-often harmonises efficacy and affordability. Your critique highlights a valid point: oversimplification can be a disservice, but we must also avoid alienating those less versed in molecular pathways. A synthesis of both perspectives would serve the community best.
nitish sharma
November 24, 2025 AT 08:56Dear fellow reader, I wish to commend the author for providing a comprehensive synopsis of current therapeutic options. The structured checklist, in particular, reflects a methodical approach befitting clinical decision‑making. It is advisable, however, to corroborate these recommendations with individualised renal assessments prior to any regimen alteration. Maintaining rigorous glycaemic monitoring whilst initiating adjunctive therapy will mitigate potential adverse events. I encourage continued adherence to evidence‑based protocols as delineated herein.
Sarah Hanson
November 30, 2025 AT 14:56I understand your concerns, but it’s important to recognise the nuanced risk‑benefit profile of each agent. A balanced view helps patients make informed choices without undue alarm.
Nhasala Joshi
December 6, 2025 AT 20:56Did you know that big pharma hides the truth about GLP‑1 side effects? 🤔💊 They don’t want us to know the real #conspiracy 😱🚨
kendra mukhia
December 13, 2025 AT 02:56Oh, please. Drop the melodrama and stick to the facts. The data on GLP‑1 safety is robust, and the “hidden agenda” narrative is just noise. If you’re looking for drama, you’ll find it in the side‑effects tables, not in baseless theories. Let’s keep the discussion grounded in peer‑reviewed studies, shall we?
Grace Hada
December 19, 2025 AT 08:56Switching from Metformin is not a decision to be taken lightly, and the literature underscores the importance of individualized assessment. Many patients remain on Metformin for years because its safety profile is unparalleled among oral agents. However, when HbA1c stubbornly hovers above target, clinicians must explore adjunctive or alternative therapies. GLP‑1 receptor agonists offer the dual benefit of glycaemic control and meaningful weight loss, which can translate to improved insulin sensitivity. Their cardiovascular outcome trials have demonstrated a reduction in major adverse events, a point that cannot be ignored. On the other hand, the cost barrier remains substantial, and insurance formularies often dictate accessibility. Sulfonylureas provide a cheap and rapid glucose‑lowering effect, yet the risk of hypoglycaemia, especially in the elderly, demands careful dose titration. Pioglitazone improves peripheral insulin sensitivity, but the associated fluid retention and heart‑failure risk limit its use in certain populations. Basal insulin remains the most potent glucose‑lowering agent, suitable for patients with severe hyperglycaemia or beta‑cell failure, but patients must be educated on injection technique and hypoglycaemia monitoring. Renal function is a pivotal factor; agents like Sitagliptin retain efficacy down to an eGFR of 30 mL/min, whereas Metformin requires dose reduction below 45 mL/min. Combination therapy, such as Metformin plus a GLP‑1 agonist, often yields synergistic effects without excessive hypoglycaemia. Lifestyle interventions-dietary modification and exercise-should accompany any pharmacologic change, as they potentiate drug efficacy. Patient preference also plays a role; some may favour an oral regimen over weekly injections despite the latter’s benefits. Shared decision‑making empowers patients, fostering adherence and better outcomes. Ultimately, the choice hinges on a balance of efficacy, safety, cost, and individual health goals. By systematically evaluating these variables, clinicians can tailor therapy that aligns with each patient’s unique circumstances.
Wyatt Schwindt
December 25, 2025 AT 14:56Solid overview, concise and on point. Thanks for the clear breakdown.