Generic Switching: When and How to Switch Between Brand and Generic Medications
When you hear generic switching, the process of replacing a brand-name drug with a chemically identical generic version. Also known as drug substitution, it’s a routine part of modern prescribing—but not always as simple as it sounds. Most of the time, it works fine. Your blood pressure pill, your antidepressant, your thyroid med—all of them can swap out without a hitch. But sometimes, that switch causes problems you didn’t expect: weird side effects, loss of control over symptoms, or even a return of the original condition. It’s not because generics are bad. It’s because biology isn’t always predictable, and your body might notice subtle differences—even when the label says they’re the same.
That’s where therapeutic equivalence, the official standard that says two drugs work the same way in the body comes in. The FDA says generics must match brand drugs in strength, dosage, and how fast they enter your bloodstream. But what if your body reacts to the fillers, the coating, or the way the tablet breaks down? People with epilepsy, thyroid disease, or mental health conditions often report changes after switching. One study found that nearly 1 in 5 patients on certain antiseizure meds had breakthrough seizures after a generic switch—even though the active ingredient was identical. That’s why some doctors avoid switching unless absolutely necessary, and why others insist on sticking with what’s working.
Then there’s the flip side: brand medications, the original drugs developed by pharmaceutical companies before generics enter the market. These are often more expensive, but sometimes they’re the only option that keeps symptoms under control. If you’ve been stable on a brand drug for years, switching to a generic might feel like a gamble. And if you’ve had a bad experience with a generic before, you’re not alone. Many patients request to stay on brand—not because they’re being difficult, but because their health depends on consistency. Insurance companies push for generics to save money, but your doctor can appeal if there’s a medical reason to stick with the original.
What you need to know is this: generic switching isn’t just a cost-saving trick. It’s a medical decision. It matters who you are, what you’re treating, and how your body responds. If you’ve ever felt off after a pharmacy switch, you’re not imagining it. There are real cases where switching caused fatigue, mood swings, or even hospital visits. And if you need to go back to the brand, it’s possible—but you’ll need documentation, a note from your doctor, and sometimes a fight with your insurer.
Below, you’ll find real stories and clear guides from people who’ve been through this. Whether you’re trying to save money, dealing with unexpected side effects, or wondering if you should switch back, the posts here give you the facts—not the hype. You’ll learn how to spot when a generic isn’t working for you, how to talk to your doctor about it, and what alternatives actually exist. No fluff. No jargon. Just what you need to make the right call for your body.
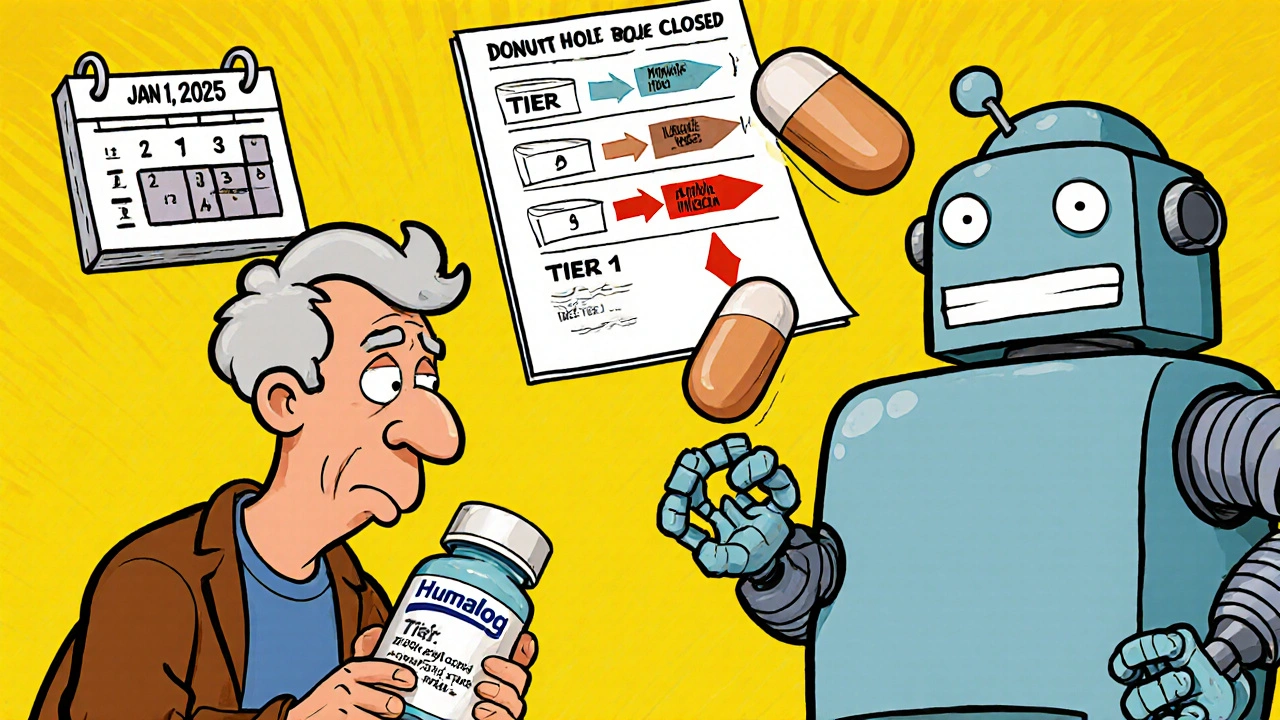
Insurance Changes and Generic Switching: How Formulary Updates Affect Your Prescription Costs in 2025
Understand how 2025 Medicare formulary updates are pushing patients toward generics and biosimilars, what it means for your prescription costs, and how to protect yourself from unexpected drug switches and price hikes.





