When you start taking an SGLT2 inhibitor for type 2 diabetes, you might not expect to feel dizzy or unusually thirsty. But these side effects aren’t rare-they’re built into how the drug works. SGLT2 inhibitors like empagliflozin, dapagliflozin, and canagliflozin aren’t just sugar-lowering pills. They act like mild diuretics, pulling extra glucose, sodium, and water out of your body through your urine. That’s why they help your heart and kidneys, but also why some people feel lightheaded, dry-mouthed, or even faint after starting them.
How SGLT2 Inhibitors Work Like Diuretics
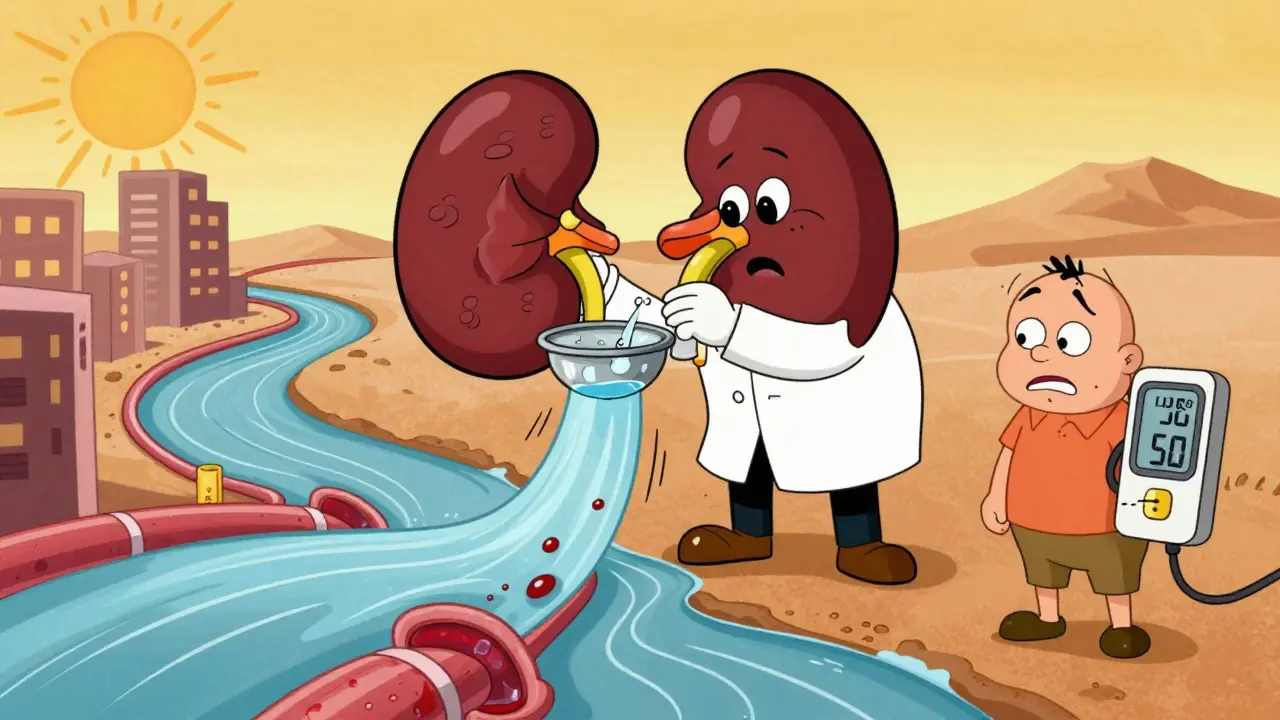
Your kidneys normally reabsorb almost all the glucose your blood filters. SGLT2 proteins in the proximal tubules are responsible for 90% of that reabsorption. When you take an SGLT2 inhibitor, those proteins get blocked. Glucose that would’ve been recycled back into your bloodstream now flows out in your urine-about 70 to 100 grams per day. That’s roughly 300 calories lost daily, which helps with weight loss. But here’s the catch: glucose doesn’t leave alone. It drags sodium and water with it. For every gram of glucose excreted, you lose about 3.4 mL of water. That’s why people on these drugs often lose 1.5 to 2.5 kg (3-5 lbs) in the first week-not from fat, but from fluid.
This isn’t accidental. It’s the same mechanism that lowers blood pressure. Less sodium in the bloodstream means less fluid volume. Less fluid means less pressure on artery walls. Studies show systolic blood pressure drops by 4-6 mmHg within two weeks, even in people without diabetes. That’s why these drugs are now recommended for heart failure, even if the patient doesn’t have high blood sugar.
Why Dehydration Happens-and Who’s at Risk
Dehydration from SGLT2 inhibitors isn’t just about drinking less water. It’s about losing more than you replace. In clinical trials, 1.3% to 2.8% of users experienced volume depletion symptoms like dizziness, low blood pressure, or fainting. That’s higher than placebo. The risk jumps significantly in certain groups:
- People over 65-reduced thirst sensation makes them less likely to drink enough
- Those with kidney impairment (eGFR below 60)-their kidneys can’t compensate as well
- Patients already on diuretics like furosemide or hydrochlorothiazide-double diuretic effect
- Anyone with systolic blood pressure below 120 mmHg-less room to drop before symptoms kick in
Canagliflozin has the highest reported rate of dehydration-related side effects, likely because it’s the most potent at glucose excretion. In the CANVAS trial, users had a 70% higher risk of volume depletion than those on placebo. Hospitalizations for dehydration were nearly twice as common in older adults. The problem often flares up during heatwaves, illness, or after intense exercise-times when fluid loss increases but intake doesn’t.
Dizziness: More Than Just a Nuisance
Dizziness is the most common complaint tied to SGLT2 inhibitors. In clinical trials, 3.5% to 5.8% of users reported it, compared to just 2.5% to 3.2% on placebo. But here’s what most patients don’t realize: it’s not random. About 63% of dizziness episodes are linked to orthostatic hypotension-your blood pressure drops when you stand up. That’s why people feel woozy getting out of bed or standing up from the couch.
It usually shows up in the first 4 weeks. That’s when fluid loss peaks and your body is still adjusting. Older adults, especially those over 75, are 2.4 times more likely to experience it. The risk doubles if you’re also taking blood pressure meds like ACE inhibitors or beta-blockers. One study found that patients with baseline systolic pressure under 130 mmHg were nearly three times more likely to get dizzy than those with higher readings.
Real-world data from patient forums like Reddit and Drugs.com confirm this. Many users report: “I started Jardiance and got dizzy standing up-my doctor said it’s normal for the first month.” Others say, “I felt so dehydrated I had to stop after three weeks.” These aren’t isolated stories. They’re predictable outcomes of the drug’s mechanism.
How Blood Pressure Drops-And Why That’s Actually Good
The blood pressure drop from SGLT2 inhibitors isn’t a bug. It’s a feature. Lowering blood pressure by 4-6 mmHg systolic reduces stroke risk by about 15% and heart attack risk by 10%. But the benefit goes beyond just pressure numbers. These drugs improve arterial stiffness, reduce inflammation, and lower intraglomerular pressure in the kidneys. That’s why they slow kidney disease progression by 30-50% in trials.
What’s surprising is that this effect happens even in non-diabetic patients. In the DAPA-HF trial, patients with heart failure but no diabetes still saw a 17% drop in cardiovascular death. The blood pressure effect was consistent across all groups. That’s why guidelines now recommend SGLT2 inhibitors for heart failure regardless of diabetes status.
But here’s the balance: the same mechanism that protects your heart can make you feel unwell. If your blood pressure drops too far-below 90 mmHg systolic-you risk fainting, falls, or injury. That’s why monitoring matters.
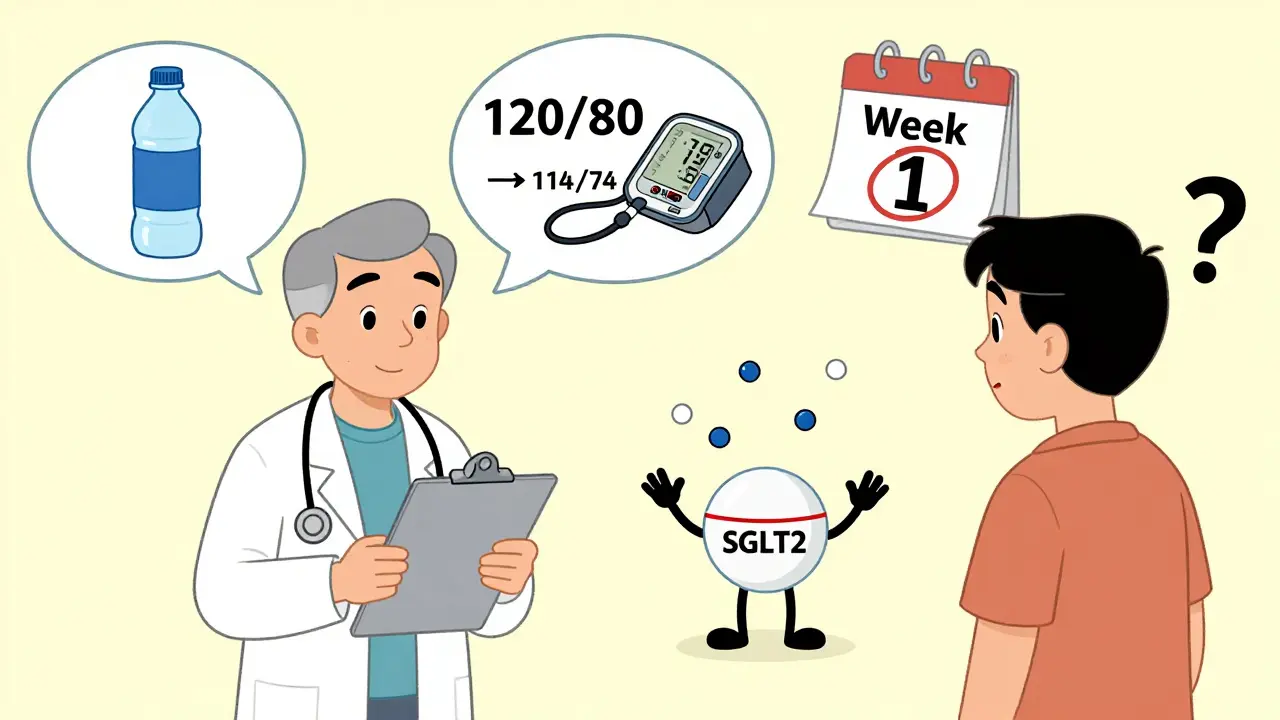
What Doctors Do to Keep You Safe
Most endocrinologists and cardiologists don’t just prescribe these drugs and walk away. They follow a clear protocol:
- Check your blood pressure and weight before starting
- Start with a lower dose-10 mg of empagliflozin instead of 25 mg
- Ask about other meds you’re on, especially diuretics
- Schedule a follow-up in 7-10 days to check for dizziness or weight loss
- Measure orthostatic blood pressure-lying down, then standing
If you feel dizzy, your doctor might reduce your other blood pressure meds by 25-50% instead of stopping the SGLT2 inhibitor. Why? Because the long-term benefits-fewer hospitalizations, lower risk of heart failure, slower kidney decline-usually outweigh the short-term side effects.
Patients are often told to drink an extra 500-1000 mL of water per day, especially in hot weather or during illness. But there’s no magic number. The key is listening to your body. Dark urine? Dry mouth? Feeling faint? Those are signals to pause, hydrate, and call your doctor.
When to Stop-or Pause-SGLT2 Inhibitors
You don’t need to stop forever. But there are times when holding the drug makes sense:
- During acute illness with vomiting or diarrhea
- If you’re admitted to the hospital for any reason
- If you develop severe dizziness or fainting
- If your systolic BP drops below 90 mmHg
- If you lose more than 3 kg (6.5 lbs) in a week without trying
Many patients resume the drug after recovery. The side effects often fade as your body adjusts. In fact, 62% of patients on Drugs.com who reported dizziness said it was mild and went away after a few weeks.
What You Can Do Right Now
If you’re taking or considering an SGLT2 inhibitor:
- Keep a water bottle handy. Sip throughout the day, don’t wait until you’re thirsty.
- Stand up slowly. Give your body time to adjust.
- Check your weight weekly. A sudden drop of more than 2 kg could mean fluid loss.
- Tell your doctor about any other meds you take, especially diuretics or blood pressure drugs.
- Don’t skip follow-ups. The first month is when risks are highest.
These drugs are powerful tools. They reduce heart failure hospitalizations, slow kidney damage, and help you lose weight. But they’re not harmless. Understanding the link between their diuretic action and side effects lets you use them safely-and get the full benefit without unnecessary risk.
Can SGLT2 inhibitors cause serious dehydration?
Yes, but it’s uncommon and usually preventable. About 1.3% to 2.8% of users experience volume depletion symptoms like dizziness, low blood pressure, or fainting. Risk is higher in older adults, people with kidney disease, or those taking other diuretics. Monitoring fluid intake, weight, and blood pressure reduces risk significantly.
Why do I feel dizzy after starting Jardiance or Farxiga?
Dizziness is often caused by orthostatic hypotension-a drop in blood pressure when you stand up. SGLT2 inhibitors reduce fluid volume and sodium, which lowers blood pressure. This effect peaks in the first few weeks. About 63% of dizziness cases are tied to this. Standing slowly and staying hydrated helps. If it persists beyond 4 weeks, talk to your doctor.
Do SGLT2 inhibitors lower blood pressure too much?
They lower blood pressure by 4-6 mmHg systolic on average, which is beneficial for heart and kidney health. But if your baseline systolic pressure is below 120 mmHg, you’re at higher risk of dropping too low. Symptoms like lightheadedness, fainting, or confusion mean you should check your BP and contact your doctor. Dose adjustments or holding the drug temporarily may be needed.
Should I stop taking my SGLT2 inhibitor if I get dehydrated?
Don’t stop without talking to your doctor. In most cases, the side effects are temporary. Increase fluids, monitor your weight, and check your blood pressure. If symptoms are severe-like fainting or very low BP-your doctor may pause the drug for a few days. But many patients resume it safely after recovery, because the long-term benefits are strong.
Are generic SGLT2 inhibitors just as risky as brand names?
Yes. Generic versions like generic empagliflozin or dapagliflozin contain the same active ingredient and work the same way. Side effect profiles are identical. The difference is cost, not safety. Whether brand or generic, the risks of dehydration and dizziness depend on your health status, not the pill’s label.
What Comes Next
As SGLT2 inhibitors become more widely used-especially in heart failure and kidney disease-primary care doctors will see more patients dealing with these side effects. The key isn’t avoiding the drugs, but managing them smartly. Check your blood pressure before starting. Stay hydrated. Watch for dizziness. Report weight loss. These simple steps turn a potentially risky medication into a life-saving one.






Dorine Anthony
December 18, 2025 AT 13:17James Stearns
December 20, 2025 AT 11:18Aadil Munshi
December 20, 2025 AT 20:54Adrienne Dagg
December 22, 2025 AT 07:44Moses Odumbe
December 22, 2025 AT 14:22Meenakshi Jaiswal
December 23, 2025 AT 05:50holly Sinclair
December 23, 2025 AT 07:17Alana Koerts
December 23, 2025 AT 23:27pascal pantel
December 24, 2025 AT 15:15Gloria Parraz
December 26, 2025 AT 12:45Nicole Rutherford
December 27, 2025 AT 19:45Mark Able
December 29, 2025 AT 03:45Nina Stacey
December 30, 2025 AT 17:49