When a woman is pregnant and dealing with chronic pain, anxiety, or seizures, the question isn’t just what to take-it’s how safe it is for the baby. Gabapentin and pregabalin, two drugs commonly called gabapentinoids, have become go-to options for many pregnant women. But recent research is painting a more complicated picture than doctors once thought.
These drugs were never designed for pregnancy. Gabapentin was first made in 1974 to treat epilepsy. Pregabalin came along in the early 2000s as a stronger version. Over time, doctors started prescribing them for back pain, fibromyalgia, nerve pain, and even anxiety-conditions that don’t always go away when you’re pregnant. In the U.S., prescriptions for gabapentin during pregnancy jumped from 0.2% of all pregnancies in 2000 to nearly 4% by 2023. That’s a 19-fold increase. And yet, we’re only now starting to understand what this means for babies.
How Gabapentinoids Reach the Baby
Gabapentin and pregabalin are small, water-soluble molecules. That means they slip easily through the placenta. A 2022 study in Frontiers in Pharmacology found gabapentin in fetal brain tissue. That’s not just passing through-it’s getting inside.
When a pregnant woman takes a 300 mg dose, the drug peaks in her blood within two to three hours. It stays in her system for about five to seven hours, meaning if she’s taking it three times a day, her baby is getting a steady drip of the drug. At therapeutic levels (2-20 μg/mL in mom’s blood), the drug reaches the same concentration in the fetus. There’s no natural filter that blocks it.
This isn’t like some medications that break down before reaching the baby. Gabapentinoids cross over cleanly. And because fetal organs are still forming and developing, even small changes in drug exposure can have lasting effects.
Major Birth Defects: The Numbers
The biggest fear for any parent is a major birth defect. So what does the data say?
A massive 2020 study in PLOS Medicine tracked over 1.7 million pregnancies. It found that gabapentin use during pregnancy didn’t raise the overall risk of major birth defects. The baseline risk in the general population is about 3%. With gabapentin, it went up to 3.21%. That’s a 0.21% absolute increase. In simple terms: out of 1,000 babies exposed, maybe one extra might have a major defect.
That sounds low. But here’s the catch: not all defects are created equal.
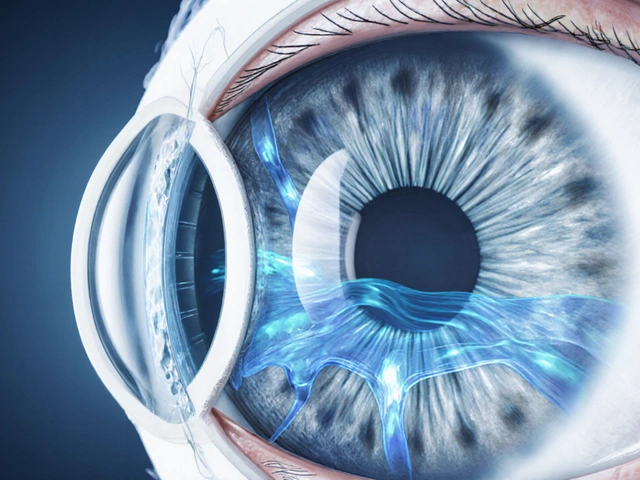
When researchers looked closer, they found a spike in conotruncal heart defects-problems with how the heart’s main chambers and vessels form. The risk went up by 40% (relative risk of 1.40). That’s not huge in percentage terms, but for a developing heart, even a small increase matters. The absolute risk? About 0.82% in exposed babies versus 0.59% in unexposed. That’s roughly 2 extra cases per 1,000 births.
Compare that to valproic acid, a seizure drug linked to a 10-11% risk of major defects. Gabapentin isn’t anywhere near that dangerous. But it’s not harmless either. And unlike lamotrigine (another epilepsy drug), which shows no such heart defect signal, gabapentin carries this specific red flag.
Preterm Birth, Low Birth Weight, and NICU Admissions
The most consistent finding across multiple studies isn’t about birth defects-it’s about what happens after birth.
When women took gabapentin in the third trimester, their babies were:
- 34% more likely to be born preterm
- 22% more likely to be small for gestational age
- 33% more likely to need NICU care
A 2018 study in Neurology followed 209 women who took gabapentin until delivery. Of the 61 babies exposed right up to birth, 23 (37.7%) ended up in the NICU. In the control group-pregnant women not taking gabapentin-only 2.9% needed NICU care. That’s more than 12 times higher.
What happened in the NICU? Babies showed signs of neonatal adaptation syndrome: jitteriness, poor feeding, trouble sleeping, high-pitched crying, and in some cases, seizures. These aren’t withdrawal symptoms like with opioids, but they’re still real, distressing, and sometimes require days of monitoring and IV fluids.
And here’s something disturbing: the risk went up the longer and more consistently the drug was taken. Women who filled two or more prescriptions during pregnancy had the highest rates of NICU admission and heart defects. It’s not just a single dose-it’s ongoing exposure that matters.

What About Pregabalin?
Pregabalin is stronger, more potent, and more expensive. But it’s not safer.
Animal studies show clear signs of developmental harm-reduced fetal weight, skeletal changes, and nervous system disruptions. Human data is more limited, but it’s enough to trigger alarms. In June 2022, the European Medicines Agency issued a safety warning specifically for pregabalin in pregnancy. They now recommend it be avoided unless absolutely necessary.
The British National Formulary (2023) says pregabalin should be avoided in pregnancy. The FDA still labels both drugs as Category C-meaning “risk cannot be ruled out.” But many doctors now treat pregabalin as riskier than gabapentin. In fact, by 2027, experts predict pregabalin use in pregnancy will drop by 25-35% as more data emerges.
What Does This Mean for Real Women?
Let’s be clear: not every woman on gabapentin will have a baby with problems. Most do not. But the risks are real, measurable, and not evenly distributed.
Most women taking gabapentin during pregnancy aren’t taking it for epilepsy. In fact, only 34% are. The majority-43%-are taking it for chronic pain. Many have back pain, sciatica, or fibromyalgia. These are debilitating conditions. For some, gabapentin is the only thing that works.
So what’s the answer? Stop taking it? Maybe not. But don’t keep taking it without thinking.
The American College of Obstetricians and Gynecologists (ACOG) says gabapentin should only be used if:
- Non-drug treatments have failed (physical therapy, acupuncture, nerve blocks)
- The condition is severe enough to justify the risk
- The lowest effective dose is used
- The drug is stopped as early as possible in the third trimester
That last point is critical. If you’re taking gabapentin for pain, consider tapering off by week 32. That’s when the risk of NICU admission and preterm birth spikes. If you’re taking it for anxiety or seizures, talk to your neurologist and OB-GYN about alternatives like lamotrigine or non-drug therapies.
What Should You Do If You’re Taking Gabapentin and Pregnant?
Don’t stop cold turkey. That can trigger seizures, worsen pain, or cause rebound anxiety. Instead:
- Get a full review with your OB-GYN and prescribing doctor. Bring your pill bottles or a list of doses.
- Ask if you’re on the lowest effective dose. Can you cut it in half?
- Request a fetal echocardiogram between weeks 20-22 if you’ve taken gabapentin consistently. It’s not routine, but it’s worth it if you’ve been on it for more than a few weeks.
- Plan to taper off by week 32 if your condition allows.
- Track your baby’s movement closely in the third trimester. Less movement can be a sign of fetal distress.
And if you’re planning to get pregnant? Talk to your doctor before conception. Switching medications takes time. You don’t want to be caught off guard.
The Future: What’s Coming Next
The FDA just mandated a new study in January 2024. Drugmakers must track 5,000 pregnancy outcomes by 2027. That’s a big step. But we’re still waiting on long-term data.
A study called NCT04567891 is tracking 1,200 children exposed to gabapentin in the womb. They’re being followed until age 5. Preliminary results are expected in late 2025. Will they show learning delays? Behavioral changes? Motor skill issues? We don’t know yet.
Meanwhile, researchers are digging into how gabapentin affects brain development at a cellular level. A 2022 lab study found that at therapeutic doses, gabapentin reduced the length of nerve branches in developing brain cells by over 40%. It also lowered levels of key genes like Nurr1, En1, and Bdnf-genes that help neurons grow, connect, and survive. These are the same genes linked to Parkinson’s and autism. It’s early science, but it suggests gabapentin doesn’t just affect the heart or lungs-it might be quietly reshaping the brain.
One thing is certain: gabapentin is not going away. It’s too useful. But we’re entering a new era where its use in pregnancy will be tightly controlled. More doctors will refuse to prescribe it unless there’s no other option. More women will ask for alternatives. And more babies will be born without unnecessary exposure.




Philip Blankenship
February 16, 2026 AT 12:01Man, I’ve been on gabapentin for fibromyalgia for years and just found out I’m pregnant last month. I’m not panicking, but I’m definitely rethinking this. My doc just shrugged and said ‘it’s fine’-like it’s a vitamin. But reading this, I realize how little we’re told. I’m scheduling a consult with a high-risk OB this week. No more autopilot.
James Lloyd
February 16, 2026 AT 13:23Important context missing: the absolute risk increase for conotruncal defects is 0.23% (0.59% → 0.82%). That’s less than the risk from maternal obesity or advanced maternal age. We’re talking about a statistical blip, not a catastrophe. The NICU stats are more concerning-but even then, 33% increased risk doesn’t mean 33% of babies are sick. It’s a relative increase from a low baseline. Stop screaming ‘baby danger’ and start talking real numbers.