When your kidneys aren’t working right, what you eat matters more than you might think. Especially protein. Too much can overload your kidneys. Too little can leave you weak, tired, and at risk for muscle loss. The truth? There’s no one-size-fits-all number. Your protein goal depends on how far your kidney disease has progressed - and whether you’re eating the right kinds of protein.
What Protein Does to Your Kidneys
Your kidneys filter waste from your blood. When you eat protein, your body breaks it down into nitrogen waste - mostly urea. Healthy kidneys handle this just fine. But when they’re damaged, that waste builds up. That’s why doctors have long advised cutting back on protein for people with chronic kidney disease (CKD). It’s not about starving yourself. It’s about reducing the workload so your kidneys don’t wear out faster.
Studies show that keeping protein intake in the right range can slow the decline of kidney function. One major 2022 Cochrane Review found that people who stuck to a lower-protein diet delayed starting dialysis by 6 to 12 months on average. That’s not just a number - it’s more time living without needles, machines, and hospital visits.
Protein Targets by CKD Stage
CKD is divided into five stages, based on how well your kidneys filter blood (measured by GFR). Your protein needs change with each stage.
- Stages 1-2 (GFR ≥60): Your kidneys are still working fairly well, but early damage is there. The Kidney Health Initiative a collaborative group that sets evidence-based guidelines for kidney care recommends no more than 0.8 grams of protein per kilogram of body weight per day. For someone weighing 150 pounds (68 kg), that’s about 54 grams of protein daily. That’s roughly the amount in two chicken breasts or three eggs. Don’t go higher than 1.3 grams/kg - studies link that to faster kidney decline.
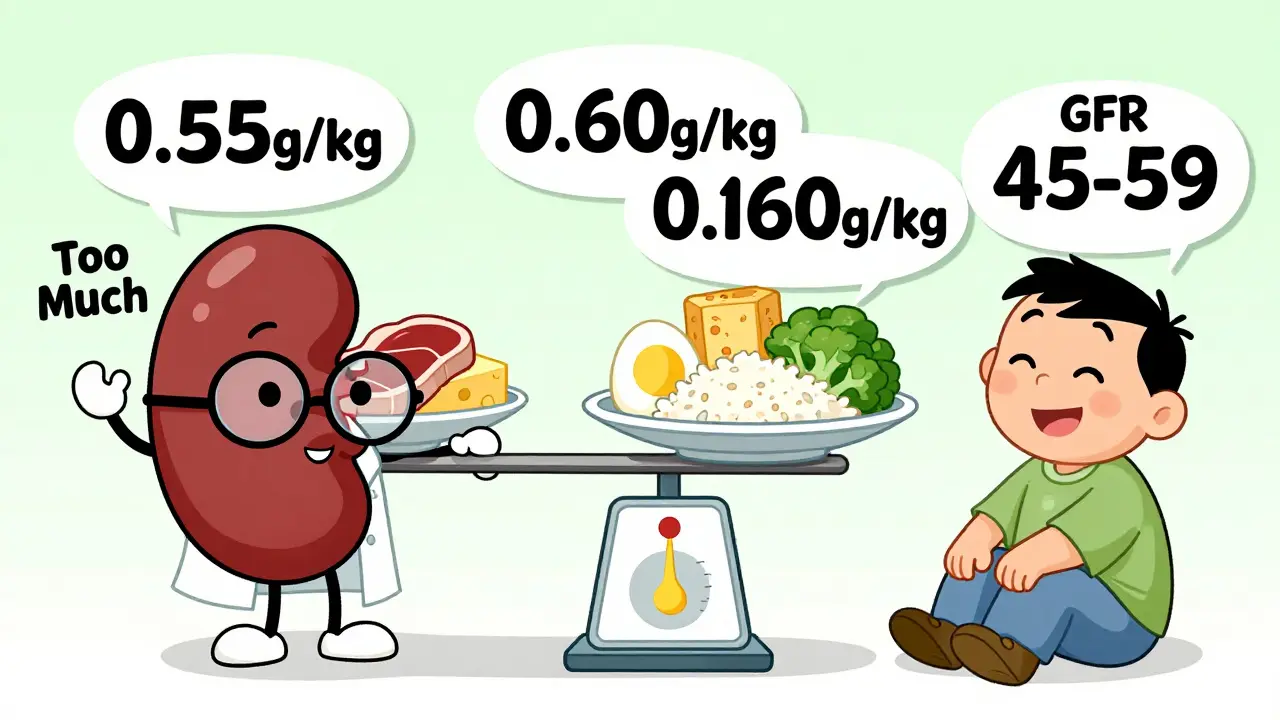
- Stages 3a-3b (GFR 45-59): Kidney function is starting to drop. The target drops to 0.55-0.60 grams/kg/day. For a 150-pound person, that’s 40-54 grams. This is where many people start feeling confused. You’re not eating enough to feel full, but you’re still not on dialysis. That’s why working with a renal dietitian becomes critical.
- Stages 4-5 (GFR ≤30): Your kidneys are failing. Protein needs are tight: 0.55-0.60 grams/kg/day, but some experts suggest up to 0.8 if you’re losing muscle or have diabetes. The DaVita a leading provider of kidney care services and nutrition resources guidelines say that when GFR falls below 25, aim for exactly 0.6 grams/kg - and make sure half of that comes from high-quality sources like eggs, fish, chicken, or soy.
Here’s the catch: these numbers are starting points. If you’re older, underweight, or have diabetes, your needs shift. A 75-year-old with stage 3 CKD might need more protein than a 40-year-old with the same stage, simply because they’re at higher risk of wasting away.
Animal vs. Plant Protein: Which Is Better?
Not all protein is created equal - especially for your kidneys.
Animal proteins (meat, dairy, eggs) are called "high-quality" because they contain all the essential amino acids your body can’t make. But they also produce more urea and phosphate - the waste your kidneys struggle to clear. Red meat, in particular, generates up to 50% more harmful compounds called advanced glycation end products (AGEs), which increase inflammation and oxidative stress in damaged kidneys.
Plant proteins (beans, lentils, tofu, nuts) are gentler. They create 20-30% less urea per gram. A 2021 meta-analysis found that swapping just 30% of animal protein with plant protein cut the risk of kidney disease worsening by 14% and lowered death risk by 11%. That’s huge.
But here’s the trade-off: plant proteins often lack key amino acids like lysine and methionine. You can’t just eat beans all day and call it good. You need to combine them - rice and beans, hummus and whole wheat pita - to get a complete profile. And if you’re in stage 4 or 5, many plant foods are high in potassium. A banana, potato, or spinach salad might be fine for a healthy person but dangerous for someone with advanced kidney disease.
Special Cases: Diabetes, Older Adults, and Muscle Loss
If you have both diabetes and CKD, balancing protein and blood sugar is tricky. The American Diabetes Association recommends 0.8-0.9 grams/kg/day - slightly higher than standard CKD guidelines. Why? Because too little protein can make blood sugar harder to control and increase muscle breakdown.
Older adults with CKD face another dilemma. A 2024 JAMA Network Open study found that seniors with early-stage CKD who ate more protein (up to 0.8-1.0 g/kg/day) lived longer. Why? Because many die from heart disease before their kidneys fail completely. For them, preserving muscle and strength might matter more than slowing kidney decline.
And then there’s protein-energy wasting - a silent killer in late-stage CKD. Up to half of people with stage 3-5 CKD lose muscle and weight without meaning to. That’s not aging. That’s malnutrition. If you’re losing weight, feeling weak, or your clothes are getting looser, your protein target may need to go up - not down.
How to Actually Do This
Knowing the numbers is one thing. Eating by them is another.
Most people struggle. A 2024 survey of over 1,200 patients found that 74% felt constantly hungry on a low-protein diet. 62% reported muscle weakness. 58% said they avoided social meals because they couldn’t eat what everyone else was having.
But those who worked with a renal dietitian? 82% said their quality of life improved. Why? Because dietitians don’t just give you a number. They teach you how to build meals.
Here’s what works:
- Use a protein calculator. The National Kidney Foundation’s free app (downloaded over 47,000 times since 2023) lets you log meals and see your protein total in real time.
- Choose high-biological-value proteins. Eggs, fish, chicken, and soy give you the most protein per gram with the least waste. A single egg has 6 grams of protein - and only 1.5 grams of phosphorus.
- Meal prep. The Kidney Kitchen website gets 1.2 million visits a month. Why? Because people need simple recipes: egg white omelets, grilled chicken with cauliflower rice, tofu stir-fry with low-potassium veggies.
- Track mixed dishes. Pasta with meat sauce? A slice of pizza? These are the hardest to count. Use apps like MyFitnessPal with renal databases, or ask your dietitian for a cheat sheet.
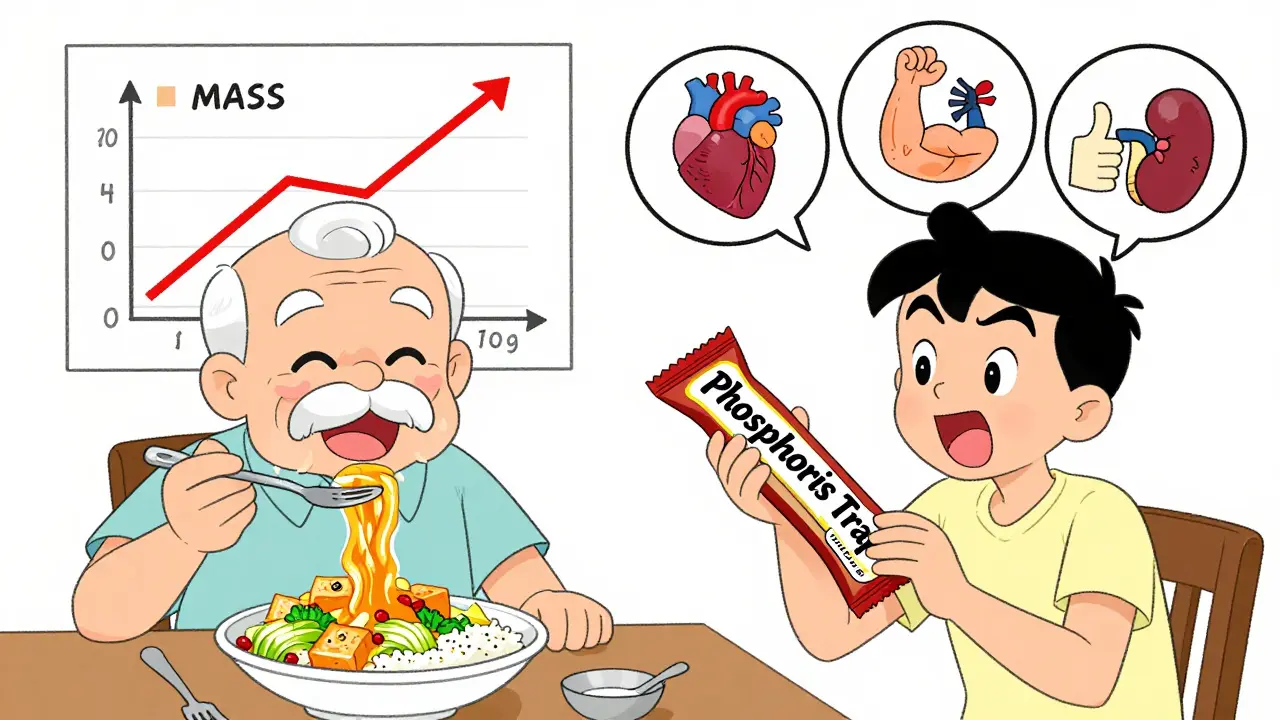
Some patients use keto acid analogues - supplements like Ketosteril - that provide the building blocks for protein without the waste. They’re prescribed to about 15% of stage 4-5 patients in Europe. They’re not magic, but they help when you’re struggling to hit targets without overloading your kidneys.

What’s Changing in 2025
The field is shifting. It’s no longer just about how much protein you eat - it’s about what kind, and who you are.
The American Society of Nephrology just launched a new algorithm that uses your blood tests, genetics, and eating habits to predict your ideal protein target. It’s still in trials, but early results show it’s more accurate than using weight alone.
Researchers are also developing new plant-based protein powders with reduced potassium. Imagine a soy protein shake that gives you 15 grams of protein but only 100 mg of potassium - perfect for stage 4 patients.
And insurance is catching up. Since January 2023, Medicare covers 3 hours of nutrition counseling in the first year, then 2 hours each year after. That’s a big deal. But only 35% of nephrologists refer patients to dietitians. That gap is costing people time, health, and quality of life.
Bottom Line: It’s Personal
There’s no perfect number for everyone. Your protein target isn’t just about your GFR. It’s about your age, muscle mass, activity level, blood sugar, and how you feel day to day.
If you’re in early CKD, don’t panic. Stick to 0.8 g/kg. Avoid junk protein - processed meats, fried chicken, protein bars with hidden phosphorus. Eat more plants, but watch your potassium.
If you’re in stage 4 or 5, work with a renal dietitian. Don’t guess. Don’t follow random blogs. Get a plan that fits your body - not a textbook.
And if you’re losing weight or feeling weak? Speak up. Protein restriction isn’t a punishment. It’s a tool. And tools need to be adjusted when they stop working.
The goal isn’t to live on a diet. It’s to live well - longer, stronger, and with fewer hospital visits.
How much protein should I eat if I have stage 3 CKD?
For stage 3 CKD, aim for 0.55 to 0.60 grams of protein per kilogram of body weight per day. For example, if you weigh 150 pounds (68 kg), that’s about 40 to 54 grams daily. If you’re older, underweight, or have diabetes, your dietitian may adjust this slightly higher - up to 0.8 g/kg - to protect your muscle mass.
Can I eat plant-based protein with kidney disease?
Yes, and it’s often better for your kidneys. Plant proteins create less waste and are linked to slower disease progression. But you need to combine them - like rice and beans - to get all essential amino acids. Watch out for high-potassium plants like potatoes, spinach, and bananas if you’re in stage 4 or 5. Choose lower-potassium options like cabbage, cauliflower, and apples.
Why do I feel weak on a low-protein diet?
Feeling weak could mean you’re not getting enough calories or high-quality protein. Many people cut protein too much and end up losing muscle. This is called protein-energy wasting. Talk to your dietitian - you may need to increase protein slightly or add keto acid supplements. Also, make sure you’re eating enough carbs and healthy fats to fuel your body.
Should I use protein supplements for kidney disease?
Most regular protein powders are dangerous for CKD because they’re loaded with phosphorus and potassium. But keto acid analogues like Ketosteril are specially designed for kidney patients - they provide protein building blocks without the waste. These require a prescription and are usually only recommended for stage 4-5 patients who struggle to meet protein goals without overloading their kidneys.
How often should I see a renal dietitian?
Start with a 60-90 minute initial consultation. Then plan for follow-ups every 4 to 6 weeks, especially in the first 3-6 months. Your needs change as your kidney function changes. Once you’ve mastered meal planning, you can space visits out to every 3-6 months. Medicare now covers 3 hours of counseling in the first year - take advantage of it.
If you’re unsure where to start, ask your nephrologist for a referral to a renal dietitian. Don’t wait until you’re exhausted or losing weight. Nutrition isn’t an afterthought - it’s part of your treatment plan.



Austin LeBlanc
December 24, 2025 AT 03:27Bro, I tried going low-protein for my stage 3 CKD and ended up losing 15 pounds in two months. My clothes were hanging off me like a scarecrow. I didn’t realize how much muscle I was burning until I couldn’t lift my damn grocery bags. Now I’m at 0.7g/kg and I actually feel human again. Don’t let some algorithm tell you to starve yourself - your body knows what it needs.
niharika hardikar
December 24, 2025 AT 11:12It is imperative to underscore that the dietary management of chronic kidney disease must adhere strictly to the KDIGO 2022 clinical practice guidelines, which unequivocally recommend protein intake thresholds predicated upon glomerular filtration rate stratification. Deviation from these evidence-based parameters, particularly in the context of protein-energy wasting, constitutes a clinically significant risk factor for accelerated nephron loss and increased all-cause mortality.
EMMANUEL EMEKAOGBOR
December 24, 2025 AT 15:36Respectfully, I’ve seen many people in my community in Nigeria struggle with this. They hear ‘low protein’ and think ‘eat less meat’ - so they just eat rice and yam all day. No protein at all. Then they get weak, get sick, and blame the doctor. The truth is, you need protein - just the right kind. Soy, eggs, fish. Even beans if you soak them long enough to reduce potassium. It’s not about fear. It’s about smart choices.
CHETAN MANDLECHA
December 25, 2025 AT 20:09So… I’m stage 3, 180 lbs. That’s like 45-50g protein a day? I eat two eggs for breakfast, a chicken breast for lunch, and a scoop of whey after gym. That’s already 70g. Am I killing my kidneys? Or is the math wrong? Someone please tell me I’m not doing this wrong.
Ajay Sangani
December 26, 2025 AT 11:58what if the real issue isnt protein but phosphorus? i mean, we focus so much on grams but what about the hidden phosphorus in processed meats, cheese, colas? maybe its not the amount of protein, its the quality and the additives that are actually wrecking kidneys. i think we’re blaming the wrong thing. also, i typo a lot but i think this matters.
Gray Dedoiko
December 26, 2025 AT 18:01I was in stage 4 and just felt like crap all the time. Weak, tired, no energy. My dietitian sat me down and said, ‘You’re not eating enough calories - protein isn’t the enemy, starvation is.’ I started adding olive oil, avocado, and egg yolks. My numbers didn’t tank. I just stopped feeling like a ghost. If you’re losing weight, don’t just lower protein - raise calories. Your body needs fuel.
Joe Jeter
December 27, 2025 AT 09:33Let’s be real - this whole ‘protein restriction’ thing is a myth pushed by pharmaceutical companies to sell keto acid analogues. Look at the data - people in rural India and Africa who eat plant-heavy diets with minimal meat live longer and have lower CKD progression. The ‘high-quality protein’ dogma is just Western bias dressed up as science. Stop listening to DaVita and start listening to your grandmother’s kitchen.
Sidra Khan
December 29, 2025 AT 03:06Just a quick note: I followed all this advice for 6 months. Lost 20 lbs. Couldn’t walk up stairs. My nephrologist said ‘it’s normal.’ My husband said ‘you look like a skeleton.’ I went back to eating chicken, eggs, and tofu - my energy came back. I’m not a statistic. I’m a person. 🍳🥦