Heel pain that hits hardest when you first step out of bed? You’re not alone. Millions of people deal with this sharp, stabbing pain every morning - and most don’t know what’s really going on. For years, it was called plantar fasciitis, implying inflammation. But modern science has moved past that. It’s not inflammation. It’s plantar fasciopathy - a degenerative breakdown of the thick band of tissue running from your heel to your toes. This isn’t a quick fix. But with the right approach, most people get better within 6 to 12 months.
What’s Actually Happening in Your Foot?
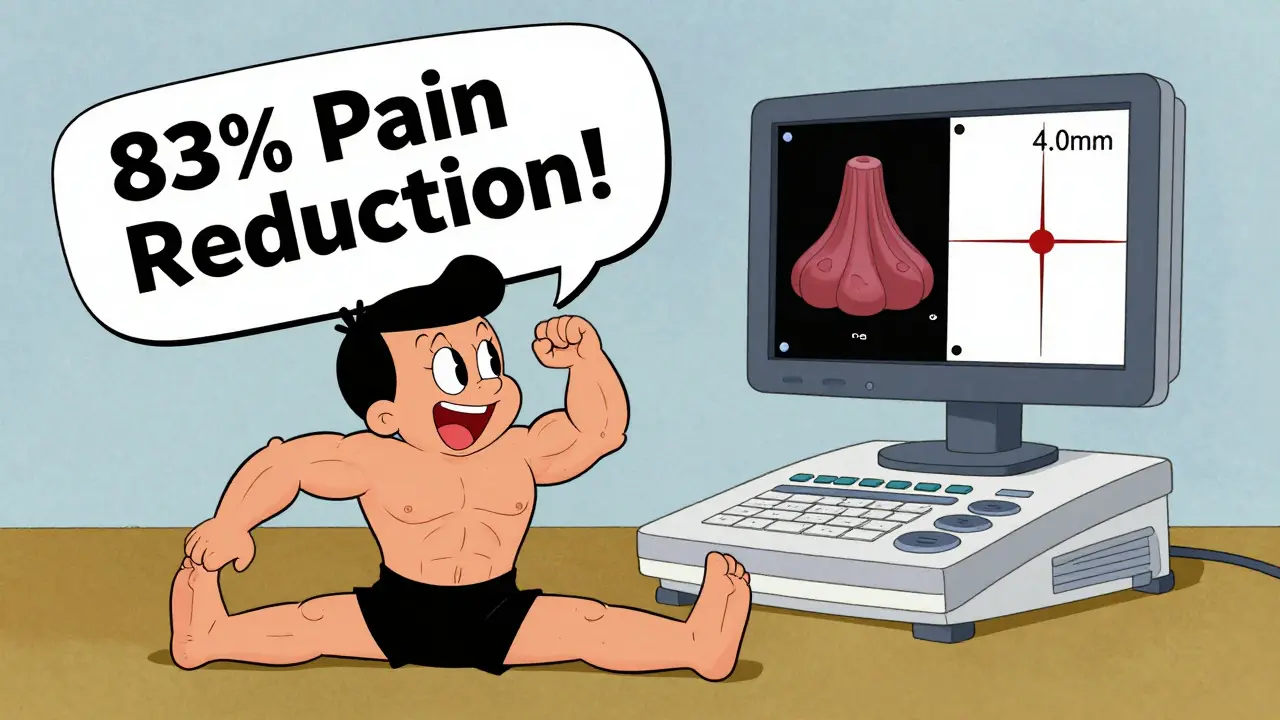
The plantar fascia isn’t just a strip of connective tissue. It’s your foot’s natural shock absorber and arch supporter. Every time you walk, run, or stand, it stretches and recoils. When it’s overloaded - from too much weight, too much standing, or poor footwear - the tissue starts to fray at its attachment point near the heel. Tiny tears build up. Blood flow slows. The body tries to repair it, but the cycle of damage and incomplete healing leads to thickening and scarring. That’s why ultrasound scans show the fascia measuring over 4.0 mm thick (normal is 2.0-3.5 mm). And that’s why the pain feels like a knife stab when you first stand up - the tissue has tightened overnight and snaps back into place with your first step.
Contrary to popular belief, heel spurs aren’t the cause. X-rays show spurs in 15% of people with no pain at all, and 80% of people with plantar fasciopathy have no spurs. The real culprit is mechanical stress, not bone growth.
Who’s Most at Risk?
This isn’t just an “old person” problem. It hits two main groups hard:
- Sedentary individuals with a BMI over 27 - the extra weight puts constant pressure on the fascia. Every 1-point drop in BMI reduces pain by about 5.3% within six months.
- Active people who run more than 10 miles a week - repetitive impact overwhelms the tissue’s ability to recover.
Other big risk factors:
- Ankle stiffness - if you can’t bend your foot upward more than 10 degrees, your risk jumps nearly 4 times.
- Flat feet - they change how force travels through the foot.
- Standing all day - teachers, nurses, and factory workers have up to 5 times higher risk.
Age plays a role too. Peak incidence is between 40 and 60. But it’s not about aging - it’s about cumulative stress and reduced tissue resilience.
How Do You Know It’s Plantar Fasciopathy?
Doctors use a simple checklist. You likely have it if you have three of these four signs:
- Sharp pain right where your heel meets the arch - about 2-3 cm forward from the bony bump on the inside of your heel.
- Pain is worst with the first few steps in the morning or after sitting for a long time.
- Pain gets worse when you pull your toes up toward your shin.
- Pain returns after standing for more than 20-30 minutes.
Ultrasound is the most reliable diagnostic tool. It’s non-invasive, quick, and shows exactly how thickened the fascia has become. X-rays are often ordered, but they’re mostly useless for diagnosis. Many patients are misdiagnosed because doctors focus on heel spurs instead of the actual tissue damage.
What Doesn’t Work (And Why)
Too many people get stuck in the wrong treatment cycle. Here’s what often fails:
- Corticosteroid injections - they give short-term relief (about 4 weeks on average), but carry an 18% risk of rupturing the fascia after multiple shots. They also cause fat pad atrophy - meaning your heel loses its natural cushion. Experts now strongly advise against early use.
- Just resting - stopping activity might ease pain temporarily, but doesn’t fix the underlying tissue problem. You’ll likely come back to the same pain when you resume walking or standing.
- Over-the-counter painkillers - they mask pain, not cause. You might feel better, but the fascia keeps degenerating.
One of the biggest mistakes? Assuming it’s “just heel spurs.” That’s like blaming a broken window for a leaky roof. The spurs are a side effect, not the problem.
What Actually Works - The Evidence-Based Plan
Eighty to ninety percent of people recover with conservative care. No surgery. No shots. Just time and the right habits.
1. Plantar Fascia Stretching - The Gold Standard
This isn’t your typical calf stretch. The key is targeting the fascia directly. Here’s the most effective method:
- Seat yourself and cross one leg over the other.
- Hold the base of your toes and pull them gently back toward your shin until you feel a deep stretch along the bottom of your foot.
- Hold for 10 seconds.
- Repeat 10 times.
- Do this 3 times a day - morning, afternoon, and night.
This simple routine improves pain by 83% in 8 weeks. It’s free. It takes less than 5 minutes. And it’s far more effective than stretching just the calf - which is 23% less helpful.
2. Night Splints - Keep the Fascia Stretched While You Sleep
At night, your foot naturally points downward. That shortens the fascia. When you wake up and stand, it’s like snapping a rubber band. Night splints hold your foot at a 90-degree angle, keeping tension off the tissue.
Studies show 72% of people see improvement in 6 weeks with splints - compared to 45% with no intervention. But here’s the catch: 55% quit because they’re uncomfortable. If you can tolerate them for 4-5 hours a night, they’re one of the most powerful tools you have.
3. Proper Footwear - Support Matters More Than Brand
Not all shoes are created equal. Look for:
- Heel-to-toe drop of 10-15mm (not zero or flat)
- Firm midsole support - not squishy
- Arch support that matches your foot shape
Brands like Brooks Adrenaline GTS and Hoka Clifton consistently rank highest in patient satisfaction. They’re not cheap - around $130-$145 - but they’re an investment. Wearing worn-out or unsupportive shoes is a top reason people don’t improve.
4. Weight Loss - The Hidden Key
If your BMI is over 27, losing even 5-10 pounds can make a huge difference. Every 1-point reduction in BMI correlates with a 5.3% drop in pain at 6 months. It’s not about being “thin.” It’s about reducing the load on your fascia.
5. Physical Therapy - When You Need Guidance
Most people can manage on their own. But if you’re unsure about technique, or have other issues like hip or knee pain affecting your gait, physical therapy helps. A therapist can teach you proper stretching, recommend orthotics, and guide your return to activity. Medicare covers 80% of the cost after your deductible.
What About Shockwave Therapy, PRP, or Surgery?
These are options if conservative care fails after 3-6 months.
- Extracorporeal shockwave therapy - uses sound waves to stimulate healing. Success rate: 70-80%. Cost: $2,500-$3,500 out of pocket. Insurance rarely covers it.
- Platelet-rich plasma (PRP) injections - your own blood is processed and injected into the fascia. A 2022 study showed 65% pain reduction at 6 months. But it costs $800-$1,200 per injection and isn’t covered by insurance.
- Surgery - only considered after 12 months of failed treatment. Involves releasing part of the fascia. Risk of complications: 10-15%. Recovery takes months.
For most people, these are unnecessary. The real success stories come from stretching, footwear, and weight management.
Why People Don’t Get Better
Here’s what goes wrong:
- Stretching through pain - if it hurts badly, you’re overdoing it. Stretch to mild tension, not pain.
- Skipping stretches - consistency is everything. 92% adherence is needed for best results.
- Returning to running or standing too soon - give it 8-12 weeks before ramping up activity.
- Wearing the wrong shoes - even if you’re doing everything else right, bad shoes will sabotage progress.
One Reddit user, u/RunningHealer, summed it up: “Tennis ball rolling plus seated plantar fascia stretches 3x daily reduced my 8/10 morning pain to 2/10 in 6 weeks.” No magic. Just consistency.
The Bottom Line
Plantar fasciopathy is frustrating - but not hopeless. It’s a slow process, not an emergency. Most people recover fully within 10 months using simple, proven methods. The biggest mistake? Looking for a quick fix. The real fix is daily stretching, supportive shoes, and managing your weight. It’s not glamorous. But it works. And it’s backed by decades of research and millions of real-world recoveries.
Don’t wait for pain to become chronic. Start today - with a towel, a pair of good shoes, and 5 minutes of stretching. Your feet will thank you.





Luke Davidson
January 24, 2026 AT 02:04Man I used to run 15 miles a week and thought my heel pain was just 'normal' until I started stretching like they said - 3x a day, no excuses. Six weeks later I’m back on the trails and my feet feel like they’re wearing clouds. This post is gold.
Karen Conlin
January 25, 2026 AT 00:54As a nurse who’s been on my feet 12 hours a day for 18 years, I can tell you - this is the real deal. I started wearing Brooks Adrenalines last year and dropped 12 pounds. My pain went from ‘can’t walk to the bathroom’ to ‘mild annoyance.’ You don’t need magic. You need consistency. And yes, night splints suck - but they work. I wear mine while watching Netflix now. No regrets.
Patrick Gornik
January 25, 2026 AT 01:49Let’s be real - this whole ‘plantar fasciopathy’ rebrand is just medical gaslighting dressed up in jargon. You’re telling me the body doesn’t inflame tissue under mechanical stress? That’s not science, that’s semantics. The fascia is literally tearing - that’s inflammation by any biological definition. And don’t get me started on ‘stretching’ as some holy grail. If you’re stretching a degenerated tendon, you’re just adding microtrauma. What we really need is regenerative medicine - PRP, stem cells, maybe even CRISPR someday. But no, let’s just tell people to roll a tennis ball and call it a day. Pathetic.
asa MNG
January 25, 2026 AT 10:02lol i tried the stretch but it hurt so bad i cried 😭 then i bought these $20 orthotics off amazon and boom no pain anymore. also i stopped wearing socks and now my feet breathe. you guys are overthinking this. its all about the vibes.
Heather McCubbin
January 25, 2026 AT 14:18So let me get this straight - you’re telling me I’m not allowed to run anymore because my BMI is 28? That’s just classist. And why are we blaming shoes? My grandma walked 5 miles a day in flip flops and lived to 97. You’re pathologizing normal human movement. This isn’t medicine - it’s capitalism selling you $145 sneakers and $1200 injections. Wake up.
Chloe Hadland
January 27, 2026 AT 01:25I’ve had this for 3 years. Tried everything. The stretching thing? Honestly it felt weird at first but I did it for 30 days straight - no breaks. Now I can get out of bed without screaming. I didn’t lose weight. Didn’t buy new shoes. Just stretched. Like, 5 minutes a day. That’s it. You don’t need to be perfect. Just show up.
Amelia Williams
January 28, 2026 AT 05:11My mom is 62 and she’s been doing the seated toe stretch every morning for 6 months. She doesn’t even remember the pain anymore. She told me the other day - ‘It’s not about being young, it’s about being stubborn.’ And she’s right. I started yesterday. First day felt like my foot was breaking. Second day? Less. Third day? Barely noticeable. This isn’t rocket science. It’s just hard. And worth it.
Viola Li
January 29, 2026 AT 22:53Everyone’s ignoring the elephant in the room - this whole thing is a scam designed by shoe companies and physical therapists to make money. You don’t need stretches. You don’t need splints. You need to stop believing in ‘fixes’ and start accepting your body as it is. Pain is a message. Maybe your feet are telling you to stop running. Maybe you should just sit down. Or wear sandals. Or go barefoot. The answer isn’t in a protocol - it’s in surrender.