Most people think hemorrhoids are just an embarrassing nuisance - something you get if you sit too long or eat too little fiber. But here’s the truth: hemorrhoids are a common, normal part of human anatomy that only become a problem when they swell. About 75% of us will deal with them at least once in our lives. And while they’re not dangerous, they can be painfully disruptive - especially when you can’t sit comfortably or see blood on the toilet paper.
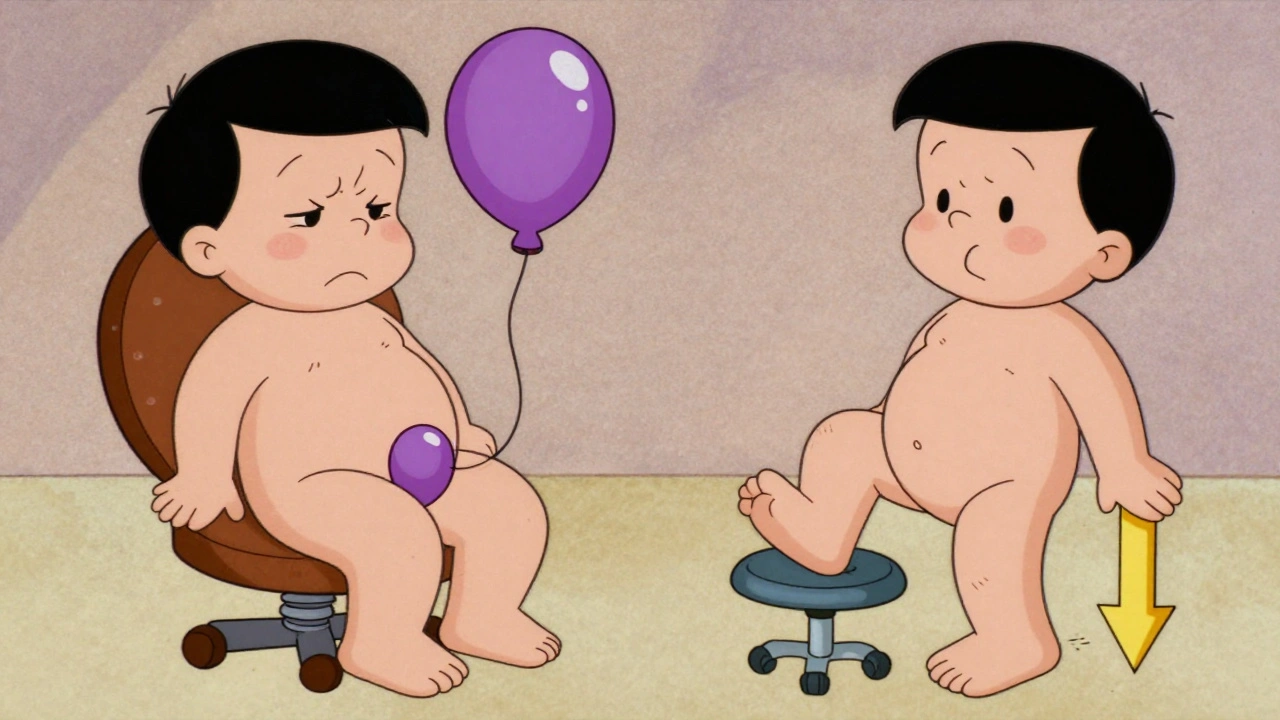
What’s the Difference Between Internal and External Hemorrhoids?
It all comes down to location. Hemorrhoids are swollen veins, but where they form makes all the difference.Internal hemorrhoids sit inside the rectum, above a line called the dentate line. This area has no pain receptors, so even when they’re swollen, you often won’t feel pain. That’s why many people don’t even know they have them - until they notice bright red blood on the toilet paper, in the bowl, or on their stool. These are graded from I to IV:
- Grade I: Bleeds but doesn’t prolapse (protrude)
- Grade II: Prolapses when you strain but pops back in on its own
- Grade III: Prolapses and needs to be pushed back in manually
- Grade IV: Stays outside permanently and can’t be pushed back
External hemorrhoids form under the skin around the anus. This area is packed with nerves, so even a small swelling can feel like a tender, itchy lump. You can see and feel them. They often cause discomfort when sitting, and if a blood clot forms inside (called a thrombosed hemorrhoid), the pain can be sudden and intense. These look like firm, purple or blue bumps - like a bruise that won’t go away.
And yes, you can have both at the same time. Many people do. That’s why symptoms can get confusing. Is the burning from external swelling? Is the bleeding from an internal one? Or both?
What Causes Hemorrhoids to Flare Up?
It’s not just about being constipated - though that’s a big one. Hemorrhoids happen when pressure builds up on the veins in your rectum and anus. Common triggers include:- Straining during bowel movements (especially if you’re holding it in or pushing too hard)
- Sitting on the toilet for more than 5 minutes - scrolling, reading, or just zoning out
- Chronic diarrhea or constipation
- Pregnancy - up to one in three pregnant women get them
- Obesity
- Lifting heavy weights regularly
- Genetics - if your family has a history, you’re more likely to get them
Here’s something most people don’t realize: your posture matters. Sitting with your knees level with your hips puts extra pressure on your rectal veins. But if you put your feet on a small stool while you poop, you angle your pelvis just right - reducing pressure by about 30%. It’s simple, free, and surprisingly effective.
What Else Could It Be? Don’t Assume It’s Hemorrhoids
Rectal bleeding sounds like hemorrhoids - but it’s not always. You could have an anal fissure - a small tear in the lining of the anus. Fissures cause sharp, tearing pain during bowel movements, often followed by a burning sensation that lasts for hours. They don’t usually cause lumps or swelling, just pain and a little blood.Even worse, bleeding can be a sign of something more serious - like colorectal cancer, inflammatory bowel disease (Crohn’s or ulcerative colitis), or polyps. That’s why if you’re over 45, have a family history of colon cancer, or notice changes in your bowel habits (like new constipation, narrow stools, or unexplained weight loss), you need to see a doctor. Don’t self-diagnose. Hemorrhoids are common, but they’re also a red flag that needs checking.
Home Treatments That Actually Work
For mild cases, you don’t need surgery. Start here:- Eat more fiber - aim for 25-30 grams daily. Think beans, lentils, oats, apples with skin, broccoli, chia seeds. Most people get less than half that.
- Drink water - 8-10 glasses a day. Fiber without water just makes things worse.
- Sitz baths - sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation. No fancy gadgets needed - just a clean tub or a special basin.
- Avoid straining - if you don’t have a bowel movement after 5 minutes on the toilet, get up. Try again later.
- Use over-the-counter creams - hydrocortisone for itching, witch hazel pads for cooling relief. Don’t use them for more than a week without checking with a doctor.
One thing that helps a lot: don’t wipe too hard. Use unscented, alcohol-free wipes or damp cotton cloths. Harsh toilet paper can turn a minor irritation into a raw, painful mess.
When You Need More Than Home Care
If your symptoms don’t improve in a week or two, or if you’re in real pain, it’s time for medical treatment.For internal hemorrhoids:
- Rubber band ligation - a tiny band is placed around the base of the hemorrhoid, cutting off its blood supply. It falls off in a few days. It’s 90% effective for Grades I-III. You might feel pressure or mild cramping for a day or two.
- Sclerotherapy - a chemical is injected to shrink the vein. Less painful than banding, but may need repeat treatments.
- Infrared coagulation - heat is used to seal the blood vessels. Quick, outpatient, minimal downtime.
For thrombosed external hemorrhoids:
- If the clot is fresh (within 72 hours), a doctor can make a tiny cut to drain it. This gives almost instant pain relief.
- After 72 hours, the body usually starts absorbing the clot on its own. Ice, pain relievers, and sitz baths help until then.
For severe or recurring cases:
- Hemorrhoidectomy - surgical removal. It’s the most effective long-term solution (95% success rate) but requires 2-4 weeks of recovery. Pain is significant for the first week, and you’ll need prescription pain meds.
- Stapled hemorrhoidopexy - repositions prolapsed tissue instead of removing it. Less pain than traditional surgery, but higher chance of recurrence.
What Doesn’t Work - and What to Avoid
There’s a flood of online products promising “miracle cures” for hemorrhoids: herbal ointments, detox teas, unregulated supplements. Most are useless. Some are dangerous.The American Gastroenterological Association and the American Society of Colon and Rectal Surgeons agree: stick to science-backed treatments. Don’t waste money on unproven remedies. If it sounds too good to be true - it is.
Also, avoid these mistakes:
- Delaying care because you’re embarrassed - 68% of people wait over six months before seeing a doctor
- Using steroid creams long-term - they can thin the skin and cause more problems
- Ignoring bleeding - even if you think you know what it is

How to Prevent Them From Coming Back
Treatment helps. Prevention keeps them away. Here’s what works:- Keep eating fiber - 30 grams a day is the sweet spot. Track it with an app if you need to.
- Stay hydrated - your stool should be soft and easy to pass, not hard or pellet-like.
- Move regularly - even a 20-minute walk daily helps your digestion.
- Don’t delay bowel movements - the longer you hold it, the more pressure builds.
- Use a footstool - it’s not a gimmick. It changes your body position and reduces strain.
People who stick to these habits after treatment have only a 5-10% chance of recurrence. Those who don’t? Up to 50% get them again within a year.
When to See a Doctor
You don’t need to suffer in silence. See a doctor if:- Bleeding lasts more than a week or gets worse
- You feel dizzy, weak, or lightheaded - signs of significant blood loss
- Pain is severe and doesn’t improve with home care
- You notice changes in bowel habits - new constipation, diarrhea, or narrow stools
- You’re over 45 and haven’t had a colon cancer screening
There’s no shame in getting help. Hemorrhoids are a medical condition, not a personal failure. Doctors see them every day. They’re not judging you. They’re here to help you feel better.
Can hemorrhoids turn into cancer?
No, hemorrhoids themselves do not turn into cancer. But rectal bleeding - a common symptom of hemorrhoids - can also be a sign of colorectal cancer or other serious conditions. That’s why any new or persistent bleeding should be checked by a doctor, especially if you’re over 45 or have a family history of colon cancer.
Are hemorrhoids more common in men or women?
Hemorrhoids affect men and women equally overall. But women are more likely to get them during pregnancy - up to 35% of pregnant women experience them due to increased pressure on pelvic veins. Constipation from hormonal changes and the weight of the growing baby also play a role.
Can I exercise with hemorrhoids?
Yes - but avoid heavy lifting or straining. Walking, swimming, cycling, and light strength training are great. They help prevent constipation and improve circulation. Avoid exercises that involve holding your breath or pushing hard, like heavy squats or deadlifts, until your symptoms improve.
Is it safe to use over-the-counter hemorrhoid creams long-term?
No. Creams with hydrocortisone or other steroids should not be used for more than a week without medical advice. Long-term use can thin the skin around the anus, cause irritation, or even lead to fungal infections. Stick to short-term relief and focus on long-term fixes like diet and hydration.
How long does it take for hemorrhoids to heal?
Mild cases often improve in a few days with home care. Thrombosed external hemorrhoids can take 7-10 days to resolve on their own, or less if drained by a doctor. Internal hemorrhoids treated with banding or sclerotherapy usually shrink within a week. Surgery recovery takes 2-4 weeks. The key is consistency - keep up with fiber, water, and good bowel habits, or they’ll likely come back.





Gwyneth Agnes
December 7, 2025 AT 10:55Just eat fiber and stop sitting like a lump.
Priya Ranjan
December 9, 2025 AT 05:11Wow. Someone actually wrote something useful for once. Most people think hemorrhoids are a punishment for eating pizza and scrolling TikTok all day. But no - it’s about discipline. Fiber isn’t optional. Water isn’t a suggestion. And sitting on the toilet for 20 minutes while you scroll? That’s not relaxation - that’s self-sabotage. You wouldn’t let your car run on bad fuel, so why let your body rot from bad habits? I’ve seen people cry over this. Not because of pain - because they finally realized they were the problem.
Ashish Vazirani
December 10, 2025 AT 20:59Let me tell you something - in India, we don’t have this problem because we squat! Not sit! Not on some fancy toilet with buttons and bidets - we squat! Our ancestors knew! Our ancestors didn’t have ‘hemorrhoids’ because they didn’t sit like lazy Westerners! Now you people pay $80 for a ‘footstool’? We’ve had the perfect position for 5,000 years - and you call it a ‘gimmick’? This is cultural ignorance! And don’t get me started on those ‘witch hazel pads’ - we use neem leaves and cold water! You think you’re modern? You’re just lost!
Mansi Bansal
December 12, 2025 AT 19:37While the aforementioned content presents a clinically sound overview of hemorrhoidal pathology, it remains critically deficient in addressing the sociopolitical dimensions of pelvic floor dysfunction within late-stage capitalist societies. The normalization of prolonged sedentary behavior, commodification of bodily autonomy via proprietary sitz bath apparatuses, and the pathological individualization of systemic dietary failures - these are not merely medical phenomena, but manifestations of neoliberal bio-power. Furthermore, the implicit endorsement of over-the-counter pharmaceutical interventions as ‘solutions’ perpetuates a pharmaceutical-industrial complex that profits from chronic suffering. A truly radical approach would necessitate structural intervention: universal fiber subsidies, mandatory ergonomic workplace redesigns, and the abolition of the toilet seat as a symbol of bourgeois decadence.
Kay Jolie
December 13, 2025 AT 22:50Okay but have you heard of the new ‘Hemorrhoid Harmony’ protocol? It’s this blend of CBD-infused coconut oil, breathwork during bowel movements, and sacred geometry footstools - I swear, my pelvic floor has never felt more aligned. Also, I got my doula to do a ‘perineal rewilding’ session - it’s like acupuncture but for your butt. And yes, I track my fiber intake via a custom Notion dashboard with mood lighting. If you’re not optimizing your colon’s energetic field, you’re just… existing.
Dan Cole
December 15, 2025 AT 03:16The author’s assertion that hemorrhoids are ‘a normal part of human anatomy’ is misleading. Anatomically, they are vascular cushions - not pathologies - and their symptomatic manifestation is always pathological. The conflation of normal physiology with disease is a classic rhetorical fallacy. Furthermore, the recommendation to consume 25–30g of fiber daily is statistically unsound: the average American intake is 15g, and increasing it by 100% without addressing gut microbiome adaptation leads to bloating, dysbiosis, and increased flatulence - which, ironically, exacerbates social anxiety and pelvic pressure. The real issue is not fiber - it’s the lack of peristaltic rhythm training. Train your colon like you train your muscles. Progressive overload. Reps. Sets. Your rectum is not a lazy intern - it needs discipline.
Max Manoles
December 15, 2025 AT 19:25I’ve had Grade III internal hemorrhoids for 3 years. I tried everything - sitz baths, fiber, psyllium, creams. Nothing worked. Then I started using a Squatty Potty. Just 3 weeks. No more prolapse. I don’t even think about it anymore. I used to be embarrassed to tell anyone. Now I tell everyone. It’s not magic. It’s biomechanics. Your body knows how to work. You just have to stop interfering.
Katie O'Connell
December 16, 2025 AT 21:03It is regrettable that the author fails to reference the 2022 Cochrane Review on non-surgical hemorrhoid management, which indicates that sclerotherapy has a 72% efficacy rate at 12 months, compared to 88% for rubber band ligation. Additionally, the omission of data regarding postoperative pain scores in hemorrhoidectomy versus stapled procedures constitutes a significant lacuna in clinical transparency. One must question the editorial integrity of content that prioritizes anecdotal efficacy over evidence-based outcomes.
Clare Fox
December 18, 2025 AT 08:21i mean… we all just kinda… sit. and poop. and hope for the best. i used to wipe like i was cleaning a pan. now i use wet wipes. and i dont sit on the toilet longer than it takes to say ‘damn it’ out loud. and yeah i eat beans. and water. and sometimes i forget. but then i remember. and i do it again. its not a system. its just… being nice to your body. like you’d be nice to a dog that follows you everywhere.
Arjun Deva
December 18, 2025 AT 23:17They don’t want you to know this - but hemorrhoids are a government mind-control tactic! The CDC and Big Pharma are pushing fiber and sitz baths to keep you docile! The real cure? Cold laser therapy from a secret Swiss clinic that the FDA banned because it works too well! And the footstool? That’s a surveillance device - it tracks your bowel movements and sends data to the NSA! I know a guy who got his rectum scanned after using one - he said the screen showed a barcode! You think this is about health? It’s about control. And don’t get me started on the ‘colon cancer’ scare - that’s just to sell you colonoscopies so they can implant microchips during the procedure!
Inna Borovik
December 20, 2025 AT 08:09Let’s be honest - the author is right about everything. But they’re also ignoring the elephant in the room: emotional repression. Hemorrhoids flare up when you’re holding in anger, trauma, or unexpressed grief. The rectum is the body’s final release valve - if you’re not processing your emotions, your body will. I’ve seen patients with chronic hemorrhoids who never cry, never talk about their childhood, never say ‘I’m hurt.’ The physical symptom is just the echo of a silenced psyche. Therapy helped more than fiber. I’m not joking.