Mycophenolate Dose Adjustment Calculator
Manage GI Side Effects
Based on article findings: Reducing dose by 1/3 often resolves diarrhea while maintaining therapeutic levels (1-3.5 μg/mL).
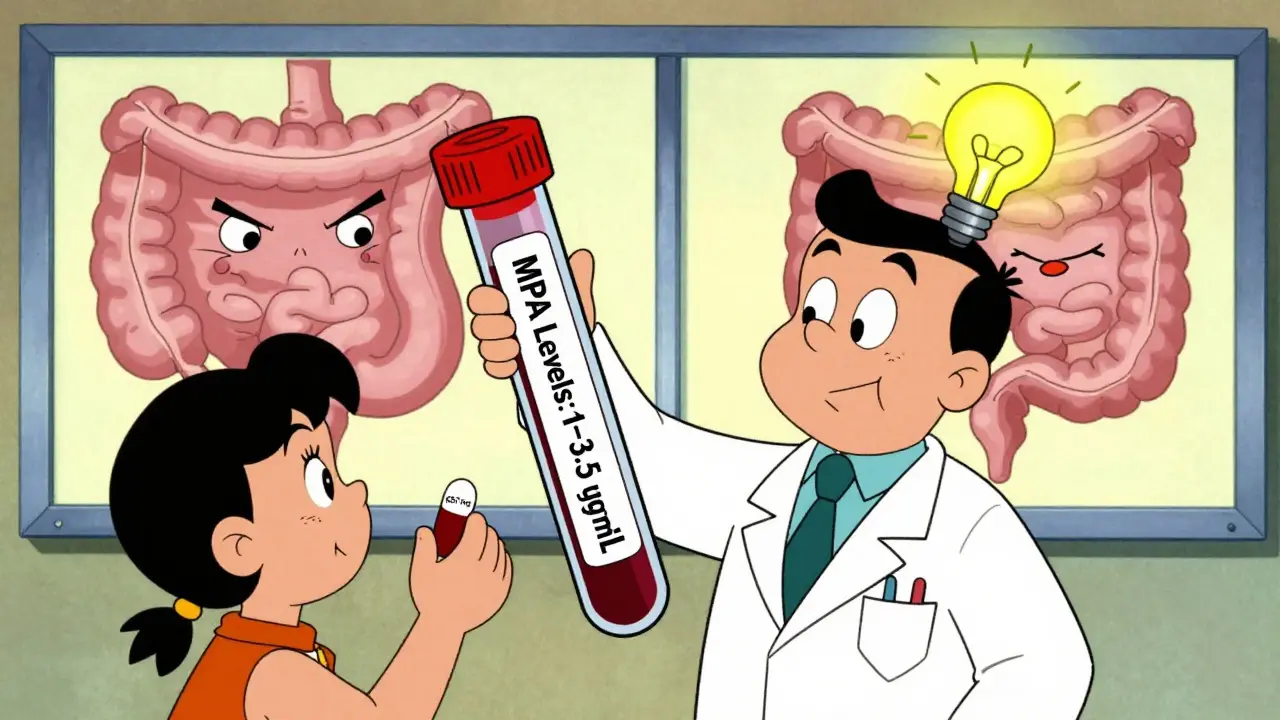
Therapeutic Monitoring
Based on Johns Hopkins study: 78% of patients resolved diarrhea with 1/3 dose reduction while maintaining safe levels.
Your Adjusted Dose
mg/day
Estimated MPA Levels
Typical range: 1-3.5 μg/mL
Key Recommendations
- 1 Always adjust doses under medical supervision
- 2 Take with small bland snack if nausea persists
- 3 Consider Myfortic formulation if CellCept causes issues
- 4 Monitor for colitis symptoms (bloody diarrhea, fever)
More than half of people taking mycophenolate for a kidney transplant or autoimmune disease will experience nausea or diarrhea. It’s not rare - it’s expected. And if you’re one of them, you’re not alone. These side effects don’t mean the drug isn’t working. They mean your body is reacting to it. The good news? You can manage them without stopping the medication - if you know how.
Why Mycophenolate Causes Nausea and Diarrhea
Mycophenolate, sold as CellCept or Myfortic, works by slowing down your immune system. It blocks a key enzyme called IMPDH that immune cells need to multiply. But that same enzyme is also found in the lining of your gut. When it’s suppressed, your intestinal cells can’t repair themselves as quickly. That leads to inflammation, slower digestion, and irritation - which shows up as nausea, cramping, and loose stools.
Studies show up to 49% of patients have some kind of gastrointestinal issue on mycophenolate. Nausea hits about 31%, diarrhea about 30%. These aren’t just mild discomforts. For many, they’re severe enough to make people skip doses or quit the drug entirely. And that’s dangerous. Stopping mycophenolate without medical advice increases your risk of organ rejection by up to 12% in the first year.
Dose Matters - Less Can Be More
Most people start on 1,000 mg twice a day. But you don’t always need that much. A 2021 study from Johns Hopkins found that reducing the dose by one-third - say, from 1,000 mg to 667 mg twice daily - resolved diarrhea in 78% of patients within three days. Their mycophenolic acid (MPA) levels stayed in the safe, effective range: 1 to 3.5 μg/mL.
This isn’t cutting corners. It’s precision medicine. Your doctor can check your MPA levels with a simple blood test. If your levels are above 3.5 μg/mL, you’re at higher risk for side effects. The European Renal Association says patients with levels over that threshold are more than three times as likely to have diarrhea. Lowering the dose doesn’t mean less protection - it means fewer side effects and better adherence.
Switching Formulations: Myfortic vs. CellCept
If nausea and diarrhea stick around even after a dose tweak, switching from mycophenolate mofetil (CellCept) to mycophenolate sodium (Myfortic) might help. Myfortic has an enteric coating that delays release until it leaves the stomach. That means less direct irritation to your upper GI tract.
A 2022 trial with 120 kidney transplant patients showed that 65% of those who switched from CellCept to Myfortic saw their nausea and diarrhea improve significantly. The total amount of active drug (MPA) stayed the same - just the delivery changed. It’s not a magic fix, but for many, it’s enough to make the difference between tolerating the drug and quitting it.
When and How You Take It Makes a Big Difference
Timing isn’t just about convenience - it’s about control. The Cleveland Clinic recommends taking mycophenolate on an empty stomach: at least one hour before or two hours after food. Why? Because food can slow absorption and cause unpredictable spikes in drug levels, which can worsen nausea.
But here’s the twist: if you’re still getting sick, try taking it with a small, bland snack - like a few crackers or half an apple. A Reddit thread with nearly 300 transplant patients found that 62% of those who took their pill with applesauce reported less nausea. It’s not science fiction. A little food can buffer the stomach without wrecking absorption.
Also, split your doses. Instead of two big pills at once, try taking one in the morning and one in the late afternoon. That keeps drug levels steadier and gives your gut time to recover between doses.
Probiotics and Diet: What Actually Helps
Not all supplements work. But some do. Lactobacillus GG, a specific strain of probiotic, showed benefit in nearly half of patients who tried it in the same Reddit survey. Look for products with at least 10 billion CFUs per dose. Take it at least two hours away from your mycophenolate - otherwise, the drug might kill the good bacteria before they can help.
Diet-wise, avoid spicy, greasy, or high-fiber foods during flare-ups. Stick to the BRAT diet: bananas, rice, applesauce, toast. Stay hydrated. Diarrhea can lead to dehydration fast, especially if you’re also on other meds like steroids. Drink water, broth, or oral rehydration solutions. Avoid caffeine and alcohol - they irritate the gut and make things worse.
When to Worry: Mycophenolate Colitis
Most GI issues are mild. But some are serious. If you have bloody diarrhea, severe cramping, fever, or weight loss, don’t wait. This could be mycophenolate-induced colitis - a rare but dangerous inflammation of the colon. It happens in about 2% of transplant patients.
It looks like an infection, but it’s not. A colonoscopy with biopsy will show damaged, dying cells in the gut lining - the fingerprint of mycophenolate toxicity. The American Society of Transplantation says any diarrhea lasting more than seven days needs this test. You need to rule out C. diff or CMV, which are common in immunosuppressed people.
If it’s mycophenolate colitis, you’ll need to stop the drug completely. Most people recover within weeks. But if you try restarting it later, there’s a 42% chance the colitis comes back. That’s why doctors often switch you to another immunosuppressant like azathioprine or leflunomide if this happens.
What If Nothing Works?
Some people just can’t tolerate mycophenolate. About 14% of patients end up switching permanently. That’s not failure - it’s smart adaptation. Alternatives exist. Azathioprine is older and less effective, but much gentler on the gut. Leflunomide is newer and shows promise in trials, with fewer GI side effects. There’s even a new extended-release version of mycophenolate (MPA-ER) approved in 2023 that cuts diarrhea rates by 37%.
If you’re struggling, ask your transplant team about therapeutic drug monitoring. Measuring your MPA area-under-the-curve (AUC) - not just a single blood level - gives a clearer picture of how your body handles the drug. Early data suggests this can reduce GI toxicity by nearly 30% without increasing rejection risk.
Don’t Quit Without a Plan
Mycophenolate saves lives. It cuts rejection rates in half compared to older drugs. But it’s not easy. The first three to six months are the hardest. Side effects peak early and often fade with time. Many patients say their nausea and diarrhea get better after 90 days.
Don’t let fear make you stop. Talk to your doctor. Adjust the dose. Switch formulations. Change when you take it. Try probiotics. Eat better. Get tested. There are options. And if one doesn’t work, there’s another. You don’t have to choose between survival and comfort. With the right approach, you can have both.





Tony Du bled
December 23, 2025 AT 09:45Mycophenolate made me feel like my insides were being reassembled by a drunk mechanic. Took me three months to figure out applesauce was my secret weapon. No joke. Half a jar before bed, no more vomiting at 3 a.m.
Still on the drug. Still alive. Still not dead.
Charles Barry
December 24, 2025 AT 12:10They don't want you to know this, but mycophenolate is just a Trojan horse for Big Pharma to sell you more anti-nausea meds. You think they care about your gut? They care about your insurance premiums. The 'dose reduction' study? Funded by Roche. The 'switch to Myfortic' trial? Same sponsors. Wake up.
They’re selling you a slow poison and calling it precision medicine. I stopped cold turkey. My kidneys are fine. My liver? Better than ever.
Rosemary O'Shea
December 25, 2025 AT 08:28Oh, darling, you’re all just so... *casual* about this. Mycophenolate isn’t just a drug-it’s a lifestyle recalibration. The gut is the second brain, after all, and when it’s screaming, you must listen with the elegance of a Parisian soprano, not the grunts of a gym bro chugging protein shakes.
And please, for the love of all that is holy, do not take it with applesauce. That’s peasant medicine. Try a chilled chamomile infusion with a single drop of organic lavender tincture, served on a porcelain spoon. That’s how the Viennese manage transplant regimens.
Also, probiotics? Only Lactobacillus rhamnosus GG, and only if it’s from a Swiss lab with a 20-year pedigree. Otherwise, you’re just feeding your microbiome chaos.
Sam Black
December 25, 2025 AT 12:54Man, I’ve been on this stuff for 8 years. Started at 1000mg twice, felt like I was digesting sand. Dropped to 667mg after my MPA came back at 4.1-boom, life changed. No more midnight bathroom marathons.
Switched to Myfortic after a year. Less nausea, but still got the cramps. Then I started taking it with a spoonful of banana and a glass of water-no food, no coffee, no alcohol. Just simple. No magic, just consistency.
Probiotics? Yeah, I use Renew Life Ultimate Flora, 10 billion CFUs. Took it at 8 a.m. and 8 p.m., two hours away from the pill. Worked better than anything else.
Don’t quit. Just tweak. Your body’s not broken-it’s just learning a new rhythm.
Jamison Kissh
December 26, 2025 AT 00:32It’s funny how we treat this drug like it’s the enemy. Mycophenolate doesn’t attack the gut-it’s just doing its job too well. The gut lining regenerates every 3–5 days. The drug slows that. So we get inflammation. Not a defect. A side effect of survival.
But here’s the deeper question: why do we assume the body’s reaction to immunosuppression is always pathological? Maybe it’s not a flaw-it’s feedback. A signal that the system is trying to rebalance.
Maybe we need to stop trying to 'fix' the side effects and start listening to what the body’s telling us about dosage, timing, even diet. The real precision medicine isn’t in the pill-it’s in the dialogue between patient and physiology.
Vikrant Sura
December 27, 2025 AT 05:53Why are you even reading this? Just take the pill. If you can’t handle it, don’t get a transplant. Simple. No one cares about your stomach problems. You’re lucky you’re alive at all.
Candy Cotton
December 28, 2025 AT 21:47It is imperative to note that the referenced studies, while seemingly credible, lack the rigorous, federally mandated, double-blind, placebo-controlled, multi-center validation required for any legitimate medical protocol in the United States of America. The notion that applesauce can mitigate pharmaceutical side effects is not only scientifically unsound, it is an affront to American medical integrity.
My husband, a retired FDA senior auditor, would have a coronary if he saw this. You must consult a board-certified transplant specialist-preferably one who graduated from Johns Hopkins, not some Reddit thread written by a man in his pajamas.
Jeremy Hendriks
December 29, 2025 AT 22:08They say the gut is where the soul resides. Maybe that’s why mycophenolate feels like betrayal. We’re told to suppress the immune system to live-but in doing so, we’re betraying the very thing that keeps us whole. The nausea? The diarrhea? They’re not side effects. They’re the body’s last scream before surrender.
And yet-we keep taking it. Because we’ve been taught that survival isn’t about comfort. It’s about sacrifice. The gut doesn’t lie. But we’ve learned to ignore it.
Is that wisdom? Or just the quiet horror of choosing life over peace?
jenny guachamboza
December 31, 2025 AT 01:35ok so i just found out mycophenolate is linked to the illuminati and also the 5g network?? like i swear my diarrhea started right after i got my new iphone 15?? and my doctor is totally hiding the truth!! 🤫💀
also i took the probiotic but it made me fart like a chainsaw?? is that normal?? 🤔💩
someone pls help i think im being monitored by big pharma and also my toilet is judging me
Tarun Sharma
January 2, 2026 AT 00:32Thank you for sharing this comprehensive overview. The clinical data presented is both accurate and valuable. I would only add that adherence to scheduled dosing and regular monitoring of MPA levels remain the cornerstones of safe long-term management. Patients should be encouraged to maintain open communication with their nephrologists.
Gabriella da Silva Mendes
January 3, 2026 AT 14:05Okay but have you considered that maybe the real issue is that we’re all just too damn stressed? Like, my gut was fine until I started working from home and my cat started sitting on my lap during Zoom calls and now I’m eating gluten-free muffins while crying over my tax returns?
Also, I think mycophenolate is just a placebo and the real reason I feel better is because I started doing yoga and drinking kombucha and now my aura is aligned.
Also, I’m pretty sure the FDA is controlled by aliens and they put the diarrhea in there to keep us docile. 🛸👁️
Also, I took a pill with a banana and now I’m a spiritual being who communicates with my colon. I don’t need doctors. I need crystals.
Kiranjit Kaur
January 5, 2026 AT 01:25Hey, I’ve been on this for 5 years. First 3 months? Hell. Diarrhea every hour. Felt like I was losing my life. But I kept going. Tried the dose drop, switched to Myfortic, took probiotics with my morning coffee (oops, wrong timing), then finally started taking it with a tiny bit of mashed sweet potato. Changed everything.
It’s not about being perfect. It’s about being persistent. You’re not broken. You’re adapting. And you’re not alone. I’ve talked to 12 other transplant folks on Instagram and we all have our weird little hacks.
Keep going. The nausea fades. The diarrhea calms. And one day, you’ll realize-you’re not just surviving. You’re living. 🌱❤️
Jim Brown
January 5, 2026 AT 04:33The paradox of modern pharmacotherapy lies not in the drug’s mechanism, but in our epistemological framework: we demand biological precision while simultaneously rejecting the phenomenological reality of the patient’s lived experience. Mycophenolate’s gastrointestinal toxicity is not merely a pharmacokinetic artifact-it is a hermeneutic event, a bodily testimony to the tension between systemic control and organic autonomy.
When we reduce nausea to a dosage adjustment, we silence the voice of the gut. When we substitute applesauce for clinical wisdom, we risk commodifying suffering. Yet-when we listen, when we attend to the rhythm of the body’s rebellion-we may discover not a flaw in the drug, but a flaw in our assumptions about healing.
Perhaps the truest form of therapeutic intervention is not the pill, but the patience to allow the body to speak.