Medication-induced anaphylaxis is a severe, life-threatening allergic reaction triggered by drugs. It happens when your immune system overreacts to a medication, causing symptoms that can develop within minutes. Without immediate treatment, it carries a mortality rate of 0.65% to 2%. Every year in the US, over 38,000 emergency department visits result from this condition. Knowing the signs and acting fast can save lives.
What is medication-induced anaphylaxis?
Medication-induced anaphylaxis occurs when your body mistakes a drug for a harmful invader. This triggers a massive release of chemicals like histamine and tryptase. These chemicals cause blood vessels to widen, fluids to leak into tissues, and muscles to contract. The result? Multi-system symptoms that can escalate rapidly. According to the American Academy of Allergy, Asthma & Immunology (AAAAI), antibiotics like penicillin cause 69.3% of drug-induced cases. NSAIDs (such as ibuprofen) and monoclonal antibodies (like rituximab) are also common triggers. The key difference between medication-induced anaphylaxis and other reactions is speed and severity. Symptoms often appear within 5 to 30 minutes of taking the drug. Unlike milder allergies, this reaction affects multiple body systems at once.
Recognizing the symptoms
Knowing the warning signs is critical. The AAAAI 2023 guidelines define anaphylaxis as likely if you see any of these three patterns:
- Sudden skin or mucosal symptoms (like hives, swelling, or flushing) plus trouble breathing or low blood pressure
- Two or more body systems affected (skin, respiratory, heart, or gut) after exposure to a likely allergen
- Low blood pressure alone after contact with a known allergen
Use the ABCD mnemonic to quickly assess symptoms:
- Airway: Swelling of the throat, hoarseness, or trouble swallowing
- Breathing: Wheezing, shortness of breath, or chest tightness
- Circulation: Dizziness, fainting, or rapid heartbeat
- Dermatologic: Hives, itching, or facial swelling
For example, a 2022 study in the Journal of Allergy and Clinical Immunology found that medication-induced cases show higher rates of cardiovascular issues (58% have low blood pressure) compared to food-induced reactions (39%). Respiratory distress is also more common-71% of medication-triggered cases involve wheezing versus 54% for food reactions. These distinctions help differentiate it from less severe allergic responses or non-allergic reactions like "red man syndrome" from vancomycin infusions.
Immediate steps to take
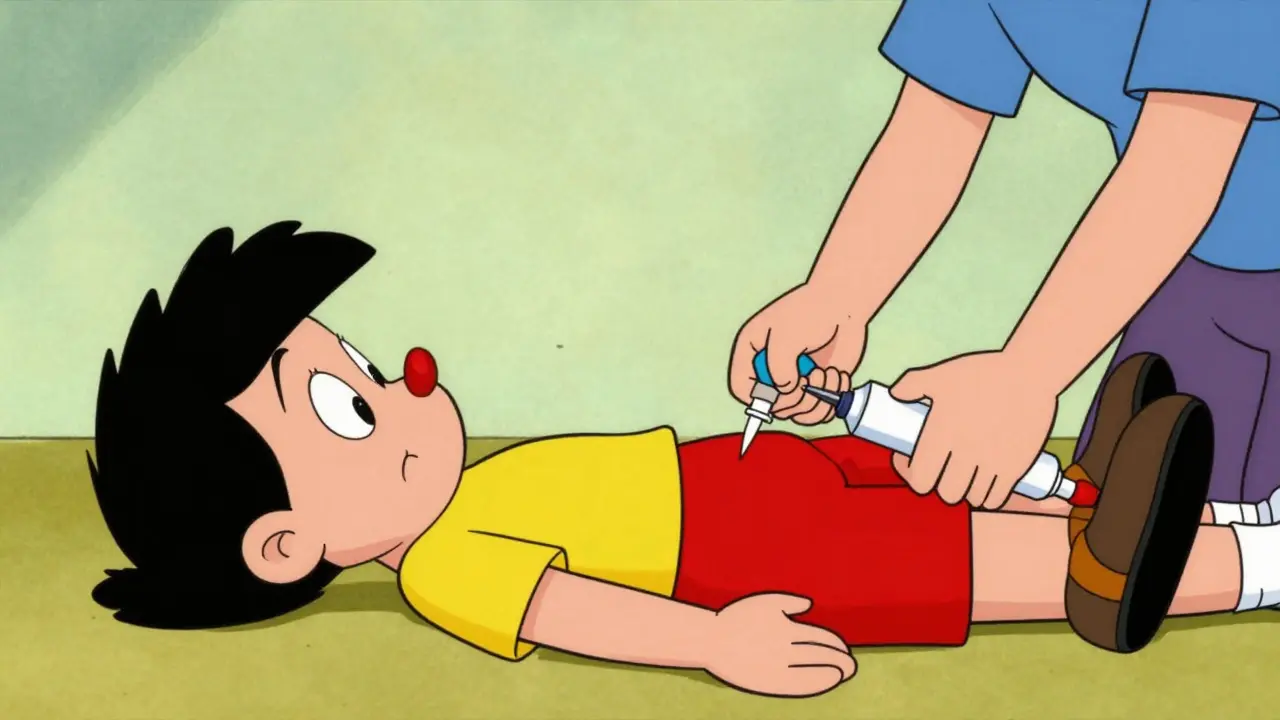
Time is everything. The Merck Manual states that 78.3% of fatal anaphylaxis cases involve delayed epinephrine administration. If you suspect anaphylaxis:
- Call emergency services immediately. Even if symptoms seem mild at first, they can worsen rapidly.
- Administer epinephrine without delay. Inject it into the outer thigh muscle-no need to remove clothing. The standard dose for adults is 0.3-0.5mg. Epinephrine works by tightening blood vessels, relaxing airway muscles, and reducing swelling.
- Stay lying down with legs elevated unless breathing is difficult, in which case sit up. Do not stand or walk.
- Monitor symptoms and be prepared to give a second epinephrine dose if symptoms return or worsen after 5-15 minutes.
Real-world evidence shows how critical speed is. Dr. Sarah Chen, an emergency physician at Massachusetts General Hospital, shared a case where a patient receiving IV contrast developed hypotension. Initially mistaken for a vasovagal response, it wasn’t until stridor (a high-pitched breathing sound) appeared that they recognized anaphylaxis. Epinephrine reversed symptoms within 4 minutes. The American Heart Association reports that 87.2% of successful outcomes correlate with correct epinephrine injection technique.
Common medication triggers
Not all drugs carry equal risk. Penicillin and related antibiotics cause 70-80% of antibiotic-related anaphylaxis cases. NSAIDs like aspirin or ibuprofen account for 15.2% of medication-induced reactions. Monoclonal antibodies (used in cancer and autoimmune treatments) trigger 5.8% of cases, while chemotherapy drugs like platinum compounds make up 4.1%. The European Journal of Allergy and Clinical Immunology found that fluoroquinolone antibiotics (e.g., ciprofloxacin) have the highest risk among antibiotics-12.7 cases per 100,000 prescriptions.
What makes medication triggers tricky? They often mimic other conditions. For instance, rapid infusion of vancomycin can cause "red man syndrome," which looks like anaphylaxis but lacks true allergic mechanisms. It typically causes flushing and itching without low blood pressure or breathing issues. The Infectious Diseases Society of America notes this is mistaken for anaphylaxis in 38.7% of cases. Distinguishing between true anaphylaxis and non-allergic reactions is crucial-using epinephrine unnecessarily can cause harm, but withholding it for a real reaction is deadly.
Prevention and management
Many medication-induced anaphylaxis cases are preventable. Johns Hopkins Hospital reduced hospital anaphylaxis incidents by 47% through their Allergy Alert System, which flags high-risk patients during medication orders. Key prevention steps include:
- Documenting all drug allergies clearly in medical records
- Asking about allergies before prescribing new medications
- Using premedication protocols for high-risk drugs (e.g., corticosteroids and antihistamines before monoclonal antibody treatments)
- Ensuring patients with known allergies carry epinephrine auto-injectors
The FDA’s 2023 Safety Communication now requires stronger anaphylaxis warnings for biologic medications. Meanwhile, the Joint Commission’s new standard (effective January 2024) mandates anaphylaxis recognition protocols in all accredited healthcare facilities. For patients, always carry an epinephrine auto-injector if you’ve had a prior reaction. The American Academy of Family Physicians reports that 52.6% of patients don’t receive this prescription after an episode, leaving them unprotected. Regularly check expiration dates-epinephrine degrades over time, especially when exposed to heat or light.
Frequently Asked Questions
Can anaphylaxis happen from a medication I’ve taken before without issues?
Yes. The first exposure to a drug often sensitizes your immune system, so reactions may occur on subsequent doses. For example, penicillin allergies can develop after multiple courses of the antibiotic. Always inform healthcare providers of any past reactions, even if they seemed minor.
Why is epinephrine the only treatment for anaphylaxis?
Epinephrine is the only medication that reverses all life-threatening symptoms of anaphylaxis. Antihistamines and steroids may help with milder symptoms but don’t address airway swelling, low blood pressure, or breathing difficulties. Delaying epinephrine increases mortality risk by 300% after 30 minutes, according to Dr. Elina Jerschow of the AAAAI.
How do I know if it’s anaphylaxis or something else like a panic attack?
Panic attacks typically cause shortness of breath and dizziness but lack physical signs like hives, swelling, or low blood pressure. Anaphylaxis involves multiple body systems (skin, breathing, circulation) and develops rapidly after medication exposure. If you’re unsure, treat it as anaphylaxis-epinephrine is safe to use even if it’s not an allergic reaction.
What should I do if I don’t have an epinephrine auto-injector?
Call emergency services immediately. While waiting, try to stay calm and lie down with legs elevated. Avoid any further medication exposure. Do not take antihistamines or steroids as substitutes-they won’t stop the reaction. Emergency responders carry epinephrine and can administer it en route to the hospital.
Can I use an expired epinephrine auto-injector?
Yes, but only as a last resort. Expired epinephrine loses potency over time, but it’s better to use an expired dose than no dose at all. The FDA extended expiration dates for some auto-injectors during shortages due to evidence of remaining effectiveness. Store your injector at room temperature and replace it before expiration.







Natasha Bhala
February 7, 2026 AT 11:27always carry epinephrine its a lifesaver
Gouris Patnaik
February 8, 2026 AT 15:44in india we take this seriously. healthcare is better prepared. you americans always ignore these things until it's too late
Jesse Lord
February 9, 2026 AT 10:15i've seen this happen before. always have epinephrine on hand. it's not just for allergies it's for emergencies. people need to know this
AMIT JINDAL
February 10, 2026 AT 01:57hey bro you know what? in india they don't even have proper hospitals like us. i mean i've traveled there and seen the conditions.
but seriously epinephrine is key. but you need to have it in your pocket always.
like even if you're just walking around. and also don't forget to check the expiration date. 😂
it's not just about having it but knowing how to use it.
the first time i had to use it i was scared.
but once you do it once it's easy.
also, make sure to store it properly. heat can mess it up.
and don't forget to replace it when it's expired.
it's not just a pill you take. it's a life-saving tool.
you have to be prepared for anything.
i've had friends who didn't carry it and it was bad.
so yeah, always have it.
and check the date.
i know it's annoying but it's worth it.
trust me.
i've been through it.
it's scary but being prepared makes all the difference.
you don't want to be that person who didn't have it when they needed it.
it's not just for allergies.
it's for any severe reaction.
so yeah, carry it.
always.
and check it.
and replace it.
and know how to use it.
that's the key. 🤷♂️
Catherine Wybourne
February 11, 2026 AT 01:51it's funny how we all think we're safe until it happens. but seriously carrying epinephrine is a no-brainer. i've seen people panic when they don't have it. always be prepared. it's like wearing a seatbelt - you hope you never need it but you're glad it's there
Ashley Hutchins
February 12, 2026 AT 14:07people need to stop being lazy and carry epinephrine. it's not hard. you can get it at any pharmacy. but no one do. they just wait until it's too late. i'm so tired of seeing this. it's not rocket science. just carry it. duh
Lakisha Sarbah
February 13, 2026 AT 18:20this is such important info. i had no idea abt the stats. always good to have epinephrine on hand. thanks for sharing. it's good to know what to do in case of emergency
Niel Amstrong Stein
February 14, 2026 AT 01:48so many people don't know about this. but it's crazy how a simple thing like epinephrine can save lives. 🌍 we need to spread awareness. also check your meds for allergies. it's a small step for a big impact. 🤔 sometimes i think we take too much for granted. but yeah, always be prepared. 🙌
Paula Sa
February 15, 2026 AT 01:05it's really important to have this info. i think everyone should know about epinephrine. it's not just for allergies but for any severe reaction. being prepared can make all the difference. we should all carry it. it's a small effort for a huge benefit