Calcium Needs Calculator for Celiac Patients
Your Recommended Daily Calcium Intake
Based on your profile, you should aim for approximately 0 mg of calcium per day.
Important Notes for Celiac Patients:
- People with celiac disease may need up to 1,200 mg daily due to reduced absorption.
- Consider taking calcium supplements with vitamin D for optimal absorption.
- Choose gluten-free certified supplements to avoid cross-contamination.
- Include calcium-rich foods like fortified plant milks, leafy greens, and sardines in your diet.
Top Calcium-Rich Foods for Celiac Patients
- Fortified soy milk (300 mg per cup)
- Cheddar cheese (lactose-free) (720 mg per 100g)
- Tofu (calcium-set) (350 mg per 100g)
- Cooked kale (150 mg per 100g)
- Sardines (with bones) (380 mg per 100g)
Key Takeaways
- People with celiac disease often struggle to absorb calcium, raising the risk of bone loss.
- Testing blood calcium, vitamin D, and bone density gives a clear picture of your status.
- Gluten‑free dairy, fortified plant milks, leafy greens, and canned fish are top calcium sources.
- Choose calcium supplements that are low in gluten and contain vitamin D for better absorption.
- Regular weight‑bearing exercise and sunlight exposure boost bone health alongside nutrition.
When you hear Calcium deficiency is a condition where the body doesn’t get enough calcium to maintain strong bones and proper muscle function, it can feel scary, especially if you also manage celiac disease - an autoimmune disorder that damages the small‑intestine when gluten is eaten, impairing nutrient absorption. The good news? With the right food choices, supplements, and monitoring, you can keep your calcium levels in check and protect your bones.
Why Calcium Matters for Anyone, and Even More for Those with Celiac Disease
Calcium is the most abundant mineral in the body, making up about 99% of the body's calcium stores in bones and teeth. The remaining 1% participates in nerve transmission, blood clotting, and muscle contraction. When intake falls short, the body pulls calcium from bone, weakening the skeleton over time.
For people with celiac disease, the risk shoots up because the damaged villi in the duodenum-where most calcium is absorbed-can’t do their job efficiently. Studies from the Celiac Disease Center at Columbia University in 2023 showed that 40% of newly diagnosed adults had low serum calcium or vitamin D levels, compared with just 12% of the general population.
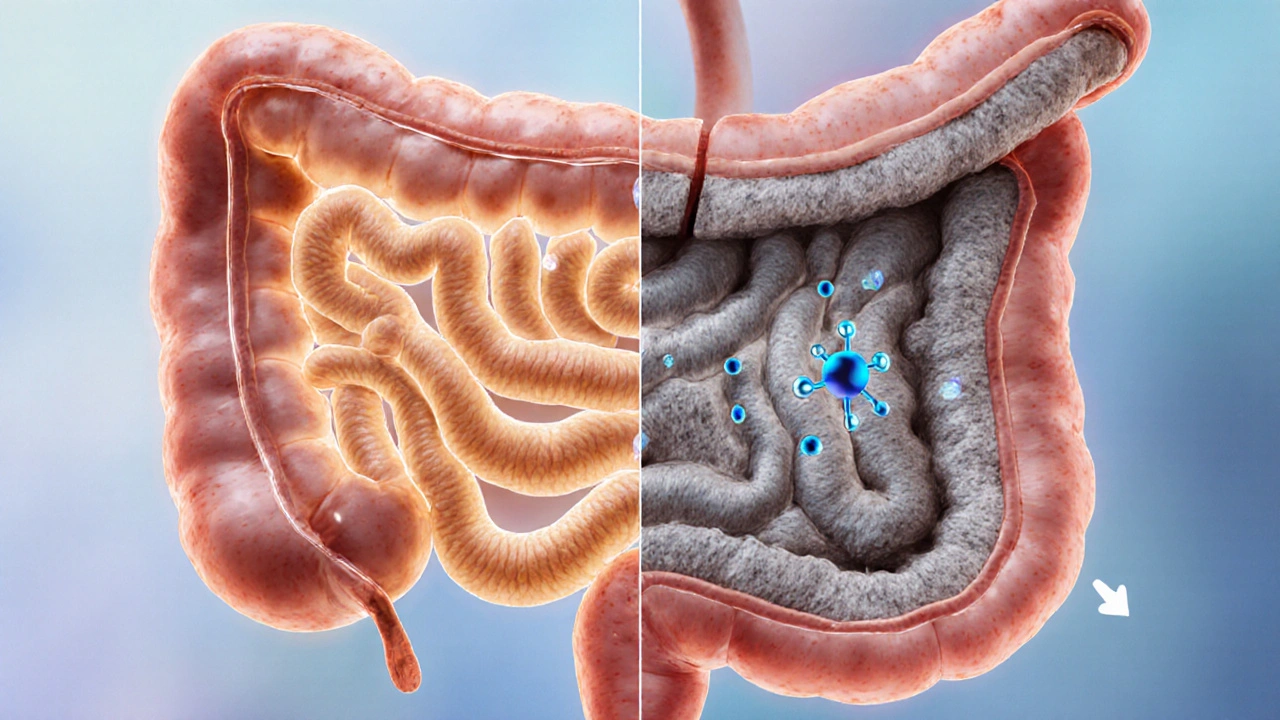
How Celiac Disease Disrupts Calcium Absorption
The small intestine is lined with finger‑like villi that increase surface area for nutrient uptake. Gluten triggers an immune response that flattens these villi, a condition called villous atrophy. With fewer villi, calcium (and vitamin D) absorption drops dramatically.
Two extra hurdles appear:
- Secondary lactose intolerance - many celiac patients lose the enzyme lactase, making dairy harder to digest.
- Increased risk of other deficiencies - low magnesium or vitamin K can also impair bone health.
Understanding these mechanisms helps you target the right fixes.

Assessing Your Calcium Status
Before you overhaul your diet, get a baseline. Ask your doctor for these simple tests:
- Serum calcium - measures calcium floating in the blood.
- 25‑hydroxy vitamin D - the best indicator of vitamin D stores.
- Parathyroid hormone (PTH) - tells if your body is trying to pull calcium from bone.
- Bone density test (DXA scan) - shows if bone loss has started.
If any values are low, your doctor may recommend a tailored supplement plan.
Gluten‑Free Foods That Pack a Calcium Punch
Here’s a quick cheat‑sheet of naturally gluten‑free foods rich in calcium. The numbers are per 100g serving unless noted.
| Food | Calcium (mg) | VitaminD (IU) | Notes |
|---|---|---|---|
| Fortified soy milk | 300 | 100 | Check label for gluten‑free certification |
| Cheddar cheese (lactose‑free if needed) | 720 | 0 | High calorie - portion control matters |
| Plain yogurt (Greek, low‑fat) | 110 | 0 | Probiotic benefit for gut health |
| Tofu (calcium‑set) | 350 | 0 | Great for vegans |
| Cooked kale | 150 | 0 | Also high in vitaminK |
| Sardines (with bones) | 380 | 270 | Omega‑3 boost |
| Almonds | 260 | 0 | Good snack, watch portion size |
| Broccoli (steamed) | 47 | 0 | Low calcium but excellent fiber |
Pair these foods with a source of vitaminD-sunlight, fortified milks, or fatty fish-to maximize absorption.
Choosing Calcium Supplements That Won’t Trigger Gluten
Supplements can fill the gap, but not all are created equal. Look for these criteria:
- Gluten‑free certification - check the label or manufacturer's website.
- Calcium type - calcium citrate is easier on the stomach and absorbs well even with low stomach acid.
- Combined vitaminD - the two work hand‑in‑hand; aim for 800-1,000IU per day if you’re low.
- Avoid unnecessary fillers - some binders contain wheat starch.
For most adults with celiac, 1,000mg of elemental calcium split into two doses (morning and evening) works well. If you have kidney disease or are on certain medications, talk to your doctor before starting.

Lifestyle Moves That Boost Bone Health
Nutrition is only half the battle. Bones need mechanical stress to stay strong.
- Weight‑bearing exercise - brisk walking, jogging, or resistance training for 30minutes most days.
- Sunlight exposure - 10‑15minutes of midday sun on face and arms a few times a week helps the skin make vitaminD.
- Limit caffeine and soda - excess caffeine can raise calcium loss in urine.
- Avoid smoking and excess alcohol - both erode bone density over time.
These habits, together with a gluten‑free, calcium‑rich diet, form a solid defense against osteoporosis.
When to Seek Professional Help
If you notice any of these signs, schedule a check‑up:
- Frequent bone or joint pain
- Muscle cramps or tingling
- Unexplained fatigue
- History of fractures after minor falls
Your healthcare team may order a repeat bone density scan, refer you to a dietitian experienced with celiac disease, or adjust your supplement dosage.
Frequently Asked Questions
Can I get enough calcium from a dairy‑free diet?
Yes. Fortified plant milks, calcium‑set tofu, canned fish with bones, and leafy greens together can meet the 1,000mg daily recommendation for most adults.
Is calcium citrate better than calcium carbonate for me?
Calcium citrate doesn’t require stomach acid for absorption, so it’s gentler on a gut that’s still healing from celiac damage. It’s the preferred choice for most patients.
How much vitaminD do I need?
Adults generally need 800-1,000IU daily if blood levels are low. Your doctor can fine‑tune the dose based on a blood test.
Will a gluten‑free diet automatically fix my calcium levels?
Healing the intestine helps, but you still need to prioritize calcium‑rich foods and possibly supplements. Monitoring labs is essential.
Can exercise replace calcium supplements?
Exercise supports bone strength but can’t replace the mineral building material. Use both for best results.





Andrea Rivarola
October 10, 2025 AT 16:41Calcium absorption can be tricky for anyone, but when the villi are damaged by gluten the challenge becomes even greater. The article does a solid job of breaking down why celiac patients often need more calcium than the general population. It explains the role of vitamin D in helping the gut pull the mineral out of food, which is something many people overlook. I especially liked the part about fortified soy milk because it provides both calcium and a decent amount of vitamin D. The table of calcium‑rich foods is handy, though I wish it had included some low‑sodium options for those watching blood pressure. Remember that secondary lactose intolerance may push you toward dairy‑free sources, so the emphasis on tofu and almond milk is spot on. The suggestion to split supplement doses into morning and evening actually aligns with the body’s natural calcium rhythms. It is also wise to get a baseline lab panel before loading up on supplements, as the article mentions. Regular weight‑bearing exercise is another pillar that complements the dietary advice. If you’re in the healing stage, a slightly higher intake-up to 1,200 mg per day-can compensate for the reduced absorption. The piece also warns about hidden gluten in supplement fillers, which is a crucial reminder for anyone with celiac disease. Pairing calcium‑rich meals with a modest amount of sunlight can boost vitamin D synthesis, a synergy the article highlights nicely. While the content is thorough, a quick summary checklist at the end would make it even more user‑friendly. Overall, the guide strikes a good balance between scientific detail and practical tips, making it accessible for both newly diagnosed patients and those who have been managing celiac for years. Keep an eye on your bone density scans, because prevention is always better than treatment.
Tristan Francis
October 14, 2025 AT 20:29They’re hiding the real calcium numbers behind gluten fear.
Keelan Walker
October 19, 2025 AT 00:16Hey folks 🌟 thanks for sharing this super useful guide it really hits the spot for anyone dealing with celiac and low calcium 😊 the list of foods is crystal clear and the tip about splitting supplements into two doses is pure gold 👍 keep up the good work and remember to get some sunshine for that vitamin D boost 🌞 stay strong and keep those bones happy!
Queen Flipcharts
October 23, 2025 AT 04:03In the grand tapestry of national health, it is incumbent upon each citizen to safeguard the skeletal fortress that supports our industrious endeavors. The exposition presented herein admirably delineates the biochemical imperatives that underpin calcium homeostasis, particularly for those burdened by the scourge of celiac disease. One must recognize that the very strength of our nation is proportional to the vigor of its populace, and calcium, as the essential mineral of bone, is a cornerstone of that vigor. Thus, the encouragement to consume fortified plant milks, calcium‑set tofu, and sardines is not merely dietary advice but a patriotic duty. Moreover, the admonition to verify supplement purity against gluten contamination resonates with the spirit of vigilance that has long defined our great nation.
Yojana Geete
October 27, 2025 AT 06:51Oh the tragedy of broken villi and the silent theft of calcium from our bodies it's like a drama unfolding within the gut each day the battle rages and we must arm ourselves with fortified milks and bold supplements lest the bones crumble beneath us
Hanna Sundqvist
October 31, 2025 AT 10:38i read that article but i think the pharma compaines dont want us to know about natural calcium sources they hide stuff
Jim Butler
November 4, 2025 AT 14:26Your enthusiasm is contagious 😀 let’s all remember that consistency in diet and exercise builds stronger foundations for health 💪 keep sharing these tips and the community will thrive together
Ian McKay
November 8, 2025 AT 18:13While the piece is thorough, it could benefit from clearer headings to guide the reader more effectively.
Deborah Messick
November 12, 2025 AT 22:00I must respectfully dissent from the premise that gluten‑free diets alone guarantee adequate calcium intake; the reality is that many gluten‑free processed foods are calcium‑poor and require deliberate supplementation.
Janice Rodrigiez
November 17, 2025 AT 01:48Spot on! The key is to pair fortified gluten‑free cereals with a calcium‑rich smoothie – think kale, almond milk, and a splash of orange for vitamin C boost.
Mary K
November 21, 2025 AT 05:35Imagine your bones as the pillars of an ancient citadel, each calcium ion a brick laid down by sunlight, movement, and mindful eating – together they forge an unbreakable legacy for future generations!
Ria Ayu
November 25, 2025 AT 09:22Your metaphor really resonates – I find that visualizing strong bones helps me stay motivated to include leafy greens and fish in my meals.
kathy v
November 29, 2025 AT 13:10Our nation's health is a reflection of our collective resolve, and calcium is the silent guardian of that strength. When we ignore the subtle signals of deficiency, we undermine the very foundation of our society. The article wisely points out that celiac patients need extra vigilance, but we must go further and demand that our food manufacturers label calcium content with crystal clarity. No more hidden gluten in supplements, no more guesswork about fortified milks. We should champion policies that ensure every grocery aisle offers affordable, calcium‑rich, gluten‑free options. Our children deserve bones that can withstand the rigors of sport and study. By embracing weight‑bearing exercises, we reinforce the skeletal architecture laid down by nutrition. Let us not be complacent; let us be proactive in fortifying our diet. The synergy of vitamin D and calcium is not a luxury, it is a necessity. Together, we build a robust future for our nation.
Jorge Hernandez
December 3, 2025 AT 16:57Totally agree 🙌 let’s push for clearer labels and more community workshops on calcium rich meals 🙏 it’ll make a huge difference for everyone
Raina Purnama
December 7, 2025 AT 20:45In many cultures, calcium‑rich foods are traditional staples, and incorporating them into a gluten‑free diet honors both heritage and health.
April Yslava
December 12, 2025 AT 00:32But don’t be fooled by the mainstream diet industry – they push low‑calcium processed gluten‑free products to keep us dependent on their supplements.
Daryl Foran
December 16, 2025 AT 04:19Honestly the whole calcium hype is overblown; most people get enough from regular diet if they just stop over‑processing everything.
Rebecca Bissett
December 20, 2025 AT 08:07Wow!!! This article is a lifesaver!!! So many details!!! Thank you!!!
Michael Dion
December 24, 2025 AT 11:54meh just another health article not much new
Trina Smith
December 28, 2025 AT 15:41Reflecting on bone health reminds me that our bodies are like temples, each nutrient a prayer whispered in daily routine 🙏