Medication Safety Checker
Check Your Medications for Dangerous Interactions
Enter your medications to see if you have dangerous combinations. The FDA reports 6.7 million Americans accidentally exceed the safe acetaminophen limit daily.
Every year, millions of people reach for combination cold and allergy meds thinking they’re doing the smart thing-grabbing one pill to handle runny nose, cough, fever, and congestion all at once. But here’s the truth: those pills might be doing more harm than good. You’re not just taking medicine. You’re mixing chemicals that can clash in ways you never expect. And if you’re already on prescription drugs, the risk goes up fast.
What’s Actually in Those Combination Pills?
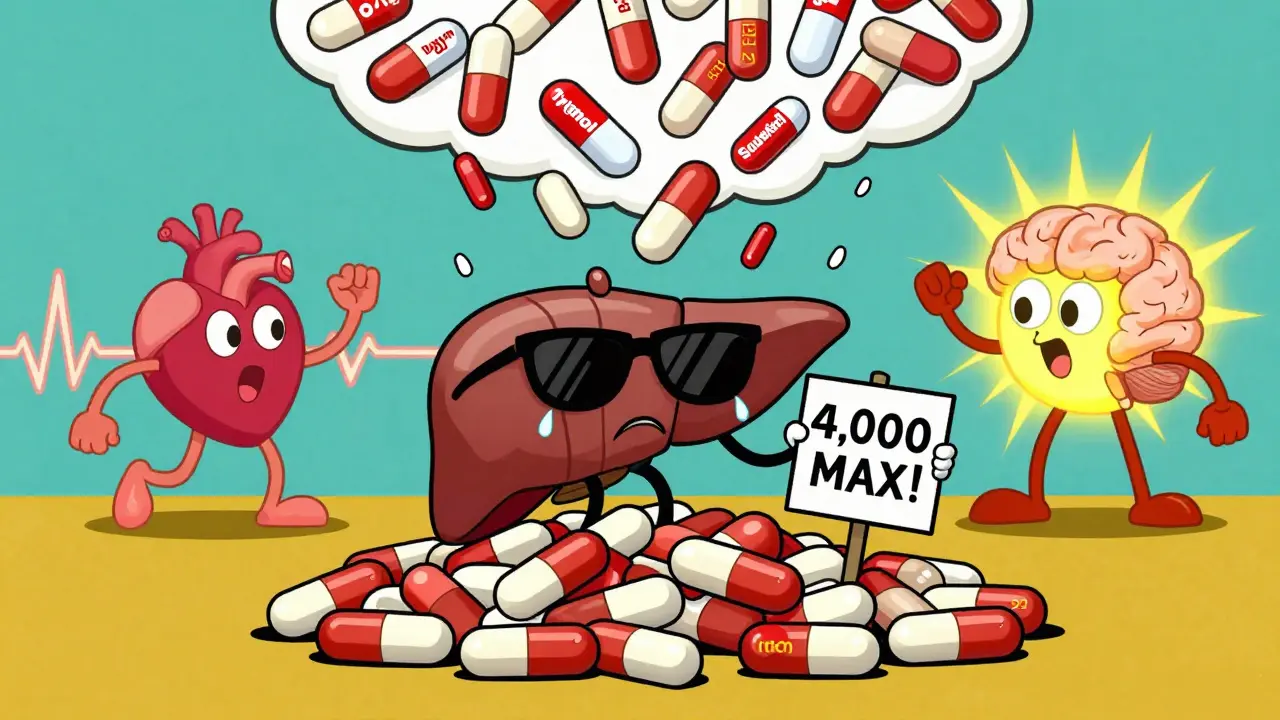
Most cold and allergy combos pack four main ingredients into one bottle: an antihistamine (like chlorpheniramine or diphenhydramine), a decongestant (pseudoephedrine or phenylephrine), a cough suppressant (dextromethorphan), and a pain reliever (usually acetaminophen). Sounds simple, right? It’s not.Acetaminophen, the most common painkiller in these combos, shows up under different names-APAP, paracetamol, or just listed as "acetaminophen." About 68% of people don’t realize "APAP" means acetaminophen. That’s why so many end up taking two or three products with it, accidentally hitting 5,000 or 6,000 mg in a day. The safe limit? 4,000 mg. Exceed it, and you risk liver failure. The CDC says 6.7 million Americans do this every year.
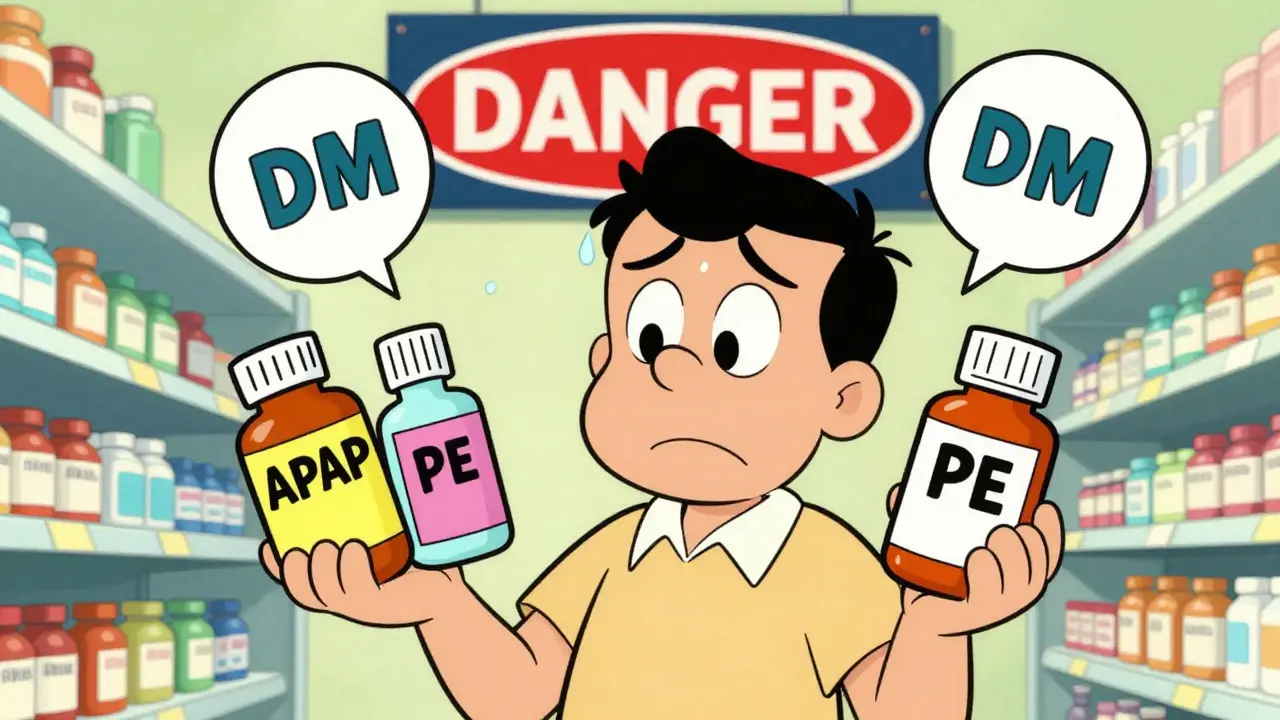
Then there’s phenylephrine. It’s the decongestant you’ll find in Tylenol Sinus, Sudafed PE, and half the store-brand cold meds on shelves. But here’s the kicker: research shows oral phenylephrine at standard doses (10 mg) doesn’t work any better than a placebo. Yet it’s still everywhere. Worse, when it’s mixed with acetaminophen, your body absorbs up to four times more phenylephrine than if you took it alone. That spike can raise your blood pressure fast-sometimes dangerously so.
Pseudoephedrine, the older decongestant found in Sudafed, actually works better. Studies show it reduces congestion by 65%, compared to phenylephrine’s 45%. But it comes with a price: it raises systolic blood pressure by 8-12 mmHg and heart rate by 5-8 beats per minute. If you already have high blood pressure, heart disease, or an irregular heartbeat, this isn’t worth the risk.
The Silent Killer: Dextromethorphan and Antidepressants
Dextromethorphan, or "DM," is the cough suppressant in DayQuil, Robitussin DM, and many others. It’s generally safe if you take it alone. But combine it with antidepressants like SSRIs (Prozac, Zoloft) or SNRIs (Cymbalta, Effexor), and you’re playing Russian roulette with your brain.That’s because both dextromethorphan and these antidepressants affect serotonin levels. When they’re together, serotonin can build up too fast. That’s serotonin syndrome-a rare but life-threatening condition. Symptoms include confusion, rapid heart rate, high fever, muscle rigidity, and seizures. A 2017 study in the Journal of Clinical Psychiatry found the risk jumps 300% when you mix these two. And it’s not just prescription meds. Some herbal supplements like St. John’s Wort also raise serotonin. You might not even know you’re taking something that interacts.
Why Labels Don’t Protect You
The FDA requires OTC labels to list active ingredients and warn about interactions. But here’s the problem: most people don’t read them. A 2022 Consumer Reports survey found 41% of people don’t check all the ingredients before buying. They see "cold medicine" and assume it’s safe. They don’t notice that the "sinus relief" bottle and the "cough syrup" both contain acetaminophen. Or that the nighttime version has diphenhydramine-the same thing as Benadryl.And the labels aren’t always clear. "Do not use with MAO inhibitors" sounds technical. Most people don’t know what an MAOI is. But if you’re on an antidepressant like phenelzine or selegiline, taking dextromethorphan within 14 days could trigger a hypertensive crisis-your blood pressure could spike to stroke-level danger.
Even the packaging is designed to confuse. Different brands use different names for the same ingredient. One bottle says "phenylephrine HCl," another says "PE." One says "acetaminophen," another says "APAP." You’re supposed to be a detective just to pick a safe product.
What You Should Do Instead
Stop reaching for the combo pack unless you have all the symptoms it treats. If you only have a stuffy nose, get a single decongestant. If you only have a cough, get plain dextromethorphan. If you have a headache and fever, get plain acetaminophen or ibuprofen. Yes, it’s less convenient. But it’s safer.Here’s a simple 3-step plan:
- Read every label. Look for the "Active Ingredients" section. Write down each one.
- Check for duplicates. If you’re taking two products and both have acetaminophen, stop. Same with dextromethorphan or phenylephrine.
- Ask a pharmacist. Walk into any pharmacy and say: "I’m taking this list of meds. Are any of them dangerous together?" Pharmacists are trained for this. They’ll catch things you miss.
Use tools like the WebMD Drug Interaction Checker or the Medisafe app. They scan barcodes and flag hidden duplicates. It takes 15 minutes-maybe less. That’s the cost of avoiding the ER.
Who’s Most at Risk?
Some people are walking into danger without even knowing it:- People over 60: Slower metabolism means drugs stay in the body longer. Higher chance of side effects.
- People with high blood pressure or heart disease: Decongestants can trigger chest pain, stroke, or heart attack.
- People on antidepressants: Serotonin syndrome risk is real. Don’t guess.
- People with liver disease: Acetaminophen is toxic to the liver. Even normal doses can be dangerous.
- Parents giving kids meds: Kids’ cold syrups often contain the same ingredients as adult versions. Dosing errors are common.
One Reddit user shared how they took DayQuil and Tylenol together, thinking they were different. They ended up in the ER with liver enzymes five times higher than normal. Another person took Sudafed PE and an SSRI, then had heart palpitations so bad they called 911. These aren’t rare stories. They’re everyday mistakes.

What’s Changing in 2025?
The FDA is finally stepping in. In March 2023, they announced new labeling rules for combination cold meds. By December 2024, all products must have high-contrast ingredient lists and bold warnings about duplicate ingredients. That’s a start.But bigger changes might be coming. In September 2023, the FDA’s advisory committee reviewed data showing phenylephrine doesn’t work as a nasal decongestant at standard doses. If they decide to pull it from the market, half the cold meds on shelves could disappear or reformulate. Companies like Johnson & Johnson are already patenting new blends using caffeine and guaifenesin instead.
Meanwhile, sales of these products are still rising. The U.S. market hit $8.2 billion in 2022 and is expected to hit $10.7 billion by 2027. But the number of ER visits linked to these meds is rising too. The Institute for Safe Medication Practices says the risks can’t be fixed by better labels alone. We need smarter choices.
When in Doubt, Skip It
The body can handle a cold on its own. Most colds last 7-10 days. Medications don’t cure them-they just mask symptoms. If you’re not sleeping, struggling to breathe, or in serious pain, then yes, treat it. But don’t reach for the combo pack just because it’s on sale.Use single-ingredient products. Know what’s in them. Double-check with your pharmacist. And if you’re on any prescription meds, especially antidepressants, blood pressure pills, or heart medications-talk to your doctor before buying anything off the shelf.
It’s not about being paranoid. It’s about being informed. Your liver, your heart, and your brain will thank you.
Can I take allergy medicine with a cold medicine?
You can, but only if you check the ingredients. Many allergy meds already contain decongestants and pain relievers. If you add a cold medicine with the same ingredients, you’ll double your dose. For example, Zyrtec-D has pseudoephedrine. Adding Sudafed means you’re taking two decongestants. That’s dangerous. Always compare active ingredients before combining.
Is it safe to take acetaminophen with cold medicine?
Only if you know how much acetaminophen is already in the cold medicine. Most combination cold meds contain 325-650 mg per dose. If you also take Tylenol, Excedrin, or other pain relievers, you can easily hit 4,000 mg or more in a day. That’s the max safe limit. Exceed it, and you risk liver damage-even if you feel fine. Always check for APAP or acetaminophen on the label.
What’s the safest decongestant for someone with high blood pressure?
The safest option is to avoid oral decongestants entirely. Instead, try saline nasal sprays, humidifiers, or steam inhalation. If you must use a decongestant, oxymetazoline nasal spray (like Afrin) is local and doesn’t raise blood pressure as much-but don’t use it for more than 3 days. Pseudoephedrine and phenylephrine both carry cardiovascular risks. Talk to your doctor before using any decongestant if you have hypertension.
Can I take cold medicine if I’m on antidepressants?
Be extremely careful. Avoid any cold medicine with dextromethorphan (DM) if you’re on SSRIs, SNRIs, or MAO inhibitors. That combo can cause serotonin syndrome, which can be fatal. Also avoid pseudoephedrine if you’re on tricyclic antidepressants-it can spike your blood pressure dangerously. Always tell your pharmacist or doctor what antidepressants you’re taking before buying anything OTC.
Why do some cold medicines work better than others?
It’s not about the brand-it’s about the active ingredients. Products with pseudoephedrine work better for congestion than those with phenylephrine. But phenylephrine is cheaper and easier to sell, so it’s everywhere. Dextromethorphan works for cough, but only if taken at the right dose. Acetaminophen is fine for pain, but ibuprofen might be better if you don’t have liver issues. The best product is the one with the fewest ingredients you actually need.




Nikki Brown
December 24, 2025 AT 13:25Let me just say this: if you're taking combo cold meds without reading the label, you're not just irresponsible-you're a walking public health hazard. I've seen people stack acetaminophen like it's candy. Your liver doesn't care how 'convenient' it is. Stop it. Just stop.
And don't even get me started on phenylephrine. It's a placebo disguised as medicine. The FDA should ban it tomorrow. Companies are literally selling water and calling it relief. Shameful.
Also, if you're on an SSRI and took DM last week? Go see a doctor. Now. Not tomorrow. Now. Serotonin syndrome isn't a 'maybe'-it's a countdown.
I'm not mad. I'm just disappointed. In you. And in the pharmaceutical industry. And in the FDA for letting this continue.
And yes, I'm the person who keeps a printed list of all my meds in my wallet. You should too.
- Nikki, because someone has to be the adult here.
Fabio Raphael
December 25, 2025 AT 21:55I really appreciate this breakdown. I had no idea phenylephrine was basically useless. I’ve been buying Sudafed PE for years thinking I was getting something effective.
My grandma takes a combo med every winter and I’ve been trying to get her to switch to single ingredients, but she says it’s ‘too many pills.’ I’ll send her this. Maybe the numbers will convince her.
Also, the part about APAP vs acetaminophen? That’s wild. I didn’t even know they were the same. Thanks for making it so clear.
And yeah, pharmacists are underrated heroes. I’m going to start asking them every time I pick something up. Even if it’s just ‘Hey, does this have acetaminophen?’
Amy Lesleighter (Wales)
December 27, 2025 AT 02:24people just dont read labels and its crazy
i used to take nyquil and tylenol together cause i thought nyquil was just for sleep and cough
then my friend got sick and went to er cause she took 3 things with apap
now i write down every ingred on my phone before i buy anything
also phenylephrine is a scam
just use saline spray or steam
and if your on antidepressants dont even touch dm
its not worth it
your brain will thank you later
roger dalomba
December 27, 2025 AT 10:14Wow. A 10,000-word essay on how to read a medicine bottle. Groundbreaking.
Next up: ‘How to Avoid Drowning: Don’t Go in the Water.’
Also, ‘Don’t mix medicine.’ Who knew?
Meanwhile, the FDA is still letting phenylephrine exist. So I guess we’re all just supposed to be smart while the system stays dumb.
Bravo. You’ve solved everything.
- Roger, the guy who still takes DayQuil and doesn’t care.
Peter sullen
December 27, 2025 AT 12:23It is imperative to underscore, with the utmost gravity, that the concomitant administration of multiple pharmacological agents-particularly those containing acetaminophen and dextromethorphan-constitutes a statistically significant risk factor for hepatotoxicity and serotoninergic dysregulation.
Per the FDA Adverse Event Reporting System (FAERS), the incidence of acute liver injury secondary to unintentional APAP overdose has increased by 22% year-over-year since 2020.
Furthermore, the pharmacokinetic interaction between phenylephrine and acetaminophen-specifically, the enhanced bioavailability of phenylephrine in the presence of hepatic CYP2E1 substrate competition-warrants immediate clinical attention.
Therefore, I strongly recommend, as a matter of public health protocol, that all individuals maintain a current, digitally synchronized medication reconciliation list, cross-referenced against the DailyMed database, prior to any OTC acquisition.
Prevention is not merely prudent-it is a bioethical obligation.
Sophia Daniels
December 27, 2025 AT 21:16OH MY GOD I JUST REALIZED I’VE BEEN TAKING DAYQUIL AND TYLENOL TOGETHER FOR 3 YEARS.
MY LIVER IS PROBABLY A CHARCOAL BRICK.
AND I THOUGHT I WAS BEING SMART BY USING ‘ALL-IN-ONE’ MEDS.
MY MOM WAS RIGHT. SHE SAID ‘DON’T BE LAZY WITH YOUR HEALTH.’
AND NOW I’M SCARED TO EVEN LOOK AT THE COLD AISLE.
WHY IS PHENYLEPHRINE EVEN ON THE SHELF?!
WHO’S PROFITING FROM THIS? WHO’S LAUGHING?
THEY’RE LAUGHING AT US.
AND I’M CRYING IN THE PHARMACY.
- Sophia, now reading every label like it’s a contract with the devil.
Steven Destiny
December 28, 2025 AT 07:06Stop being scared of medicine. Your body can handle it. Cold meds aren’t poison. You’re not a lab rat. Stop overthinking.
I’ve taken every combo under the sun. I’m 42. Still standing. Still breathing.
Phenylephrine doesn’t work? Fine. I don’t care. It helps me sleep. That’s all I need.
And if you’re on antidepressants? Maybe you should just stay home and not take anything.
Stop scaring people. Most of this is fearmongering wrapped in a CDC report.
Live a little. Take the damn pill.
Erwin Asilom
December 28, 2025 AT 15:36For anyone reading this and feeling overwhelmed: start small.
Next time you need something for a headache, grab plain acetaminophen or ibuprofen. Just one thing.
Don’t buy the ‘sinus + cough + fever’ pack unless you actually have all those symptoms.
It’s not about being perfect. It’s about being intentional.
I used to grab whatever was on sale. Now I ask the pharmacist: ‘What’s the bare minimum I need?’
They always give me a better answer than the label.
And yes, it takes 2 extra minutes.
But your liver will thank you in 10 years.
Sumler Luu
December 29, 2025 AT 14:32Thank you for writing this. I’ve been helping my elderly neighbor sort through her medicine cabinet, and I can’t believe how many duplicates she had.
She was taking two different cold meds with acetaminophen, plus a sleep aid with diphenhydramine, and a ‘heart health’ supplement with St. John’s Wort.
We cleared it all out. Now she just takes one thing at a time.
She’s sleeping better. Her blood pressure is lower.
It’s not about being afraid. It’s about being careful.
And sometimes, that’s enough.
sakshi nagpal
December 30, 2025 AT 06:08This is so important. In India, people buy cold medicines without even knowing the ingredients. They just ask for ‘something for cough and cold’ and the shopkeeper gives them whatever is cheapest.
My cousin took a combo med and ended up with high blood pressure because it had pseudoephedrine. He didn’t even know he had high BP.
We need better education here too.
Maybe pharmacists should be required to explain ingredients in simple words, not just hand over the bottle.
Thank you for raising awareness.
- Sakshi, from Mumbai
Sandeep Jain
December 31, 2025 AT 12:30bro i took dextromethorphan and zoloft once by accident
felt like my brain was melting
heart racing
thought i was having a stroke
called my mom
she made me go to er
they said serotonin syndrome
stayed overnight
never again
now i check every label
even if its just a cough drop
damn
Brittany Fuhs
January 2, 2026 AT 10:27Wow. Just wow. Another American overreaction to a perfectly normal thing.
Other countries don’t have this panic about cold meds. They just take what works.
Here, we turn a common cold into a medical thriller.
And now we’re blaming Big Pharma? Please. The real problem is Americans who think every pill is a time bomb.
Stop being so paranoid. Your anxiety is worse than the medicine.
- Brittany, who doesn’t need a PhD to take Tylenol.
Becky Baker
January 4, 2026 AT 08:12I used to be the person who took every combo pack on sale. Then I got sick and took 3 things with acetaminophen. My liver enzymes went nuts.
Now I only buy one thing at a time.
And I always ask the pharmacist.
They’re not there to upsell you. They’re there to save your life.
So stop being lazy.
And yes, I’m talking to you, guy who just grabbed that ‘all-in-one’ bottle.
Nikki Brown
January 6, 2026 AT 06:04Steven Destiny, you’re the reason this post is necessary.
You’re the person who thinks ‘I’ve been fine for years’ means ‘I’m invincible.’
But your liver doesn’t care how ‘fine’ you feel.
It’s silent until it’s not.
And then you’re in the ER, wondering why you didn’t listen.
So no, I’m not scared. I’m just tired of people like you thinking they’re too tough for common sense.
- Nikki, still reading labels. Because someone has to.