When to Stop PPIs: Signs You Might Not Need Them Anymore
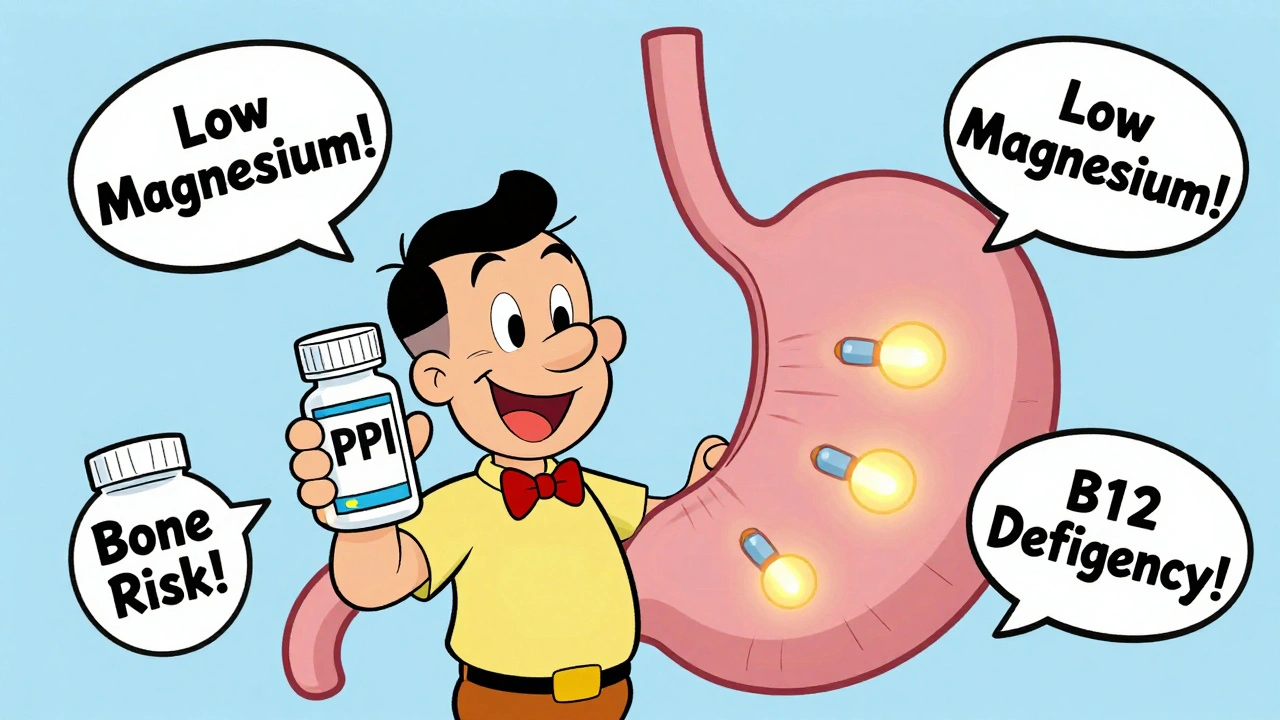
When you’ve been taking proton pump inhibitors, a class of medications that reduce stomach acid production, commonly used for heartburn and GERD for months or years, it’s easy to forget you ever started them. But many people take PPIs longer than needed—and that can bring risks like nutrient deficiencies, bone loss, or rebound acid hypersecretion. The question isn’t just can you stop? It’s when should you stop? And how do you do it without waking up in the middle of the night with burning chest pain?
Stopping PPIs isn’t as simple as skipping a pill. Your stomach can overcompensate by making even more acid after you stop, which feels like your original symptoms came back worse. This is called rebound acid hypersecretion, and it’s why doctors often recommend tapering slowly instead of quitting cold turkey. If you’ve been on PPIs for more than 4 to 8 weeks for mild heartburn, or if your symptoms improved with lifestyle changes like eating smaller meals, avoiding late-night snacks, or cutting out caffeine and alcohol, you might be a good candidate to try reducing your dose. People with confirmed GERD or ulcers often need longer treatment, but even then, regular check-ins with your provider can help determine if you’re still benefiting.
Other clues you might be able to stop include: no symptoms for 3+ months, no history of Barrett’s esophagus or severe esophagitis, and no use of NSAIDs or blood thinners that increase stomach irritation risk. If you’re on PPIs just because you "always have a little heartburn," that’s a red flag. Many people with occasional acid reflux do better with H2 blockers like famotidine, or even just antacids when needed. And if you’re taking a PPI because your doctor prescribed it for a short-term condition—like healing an ulcer after an H. pylori infection—you should already be off it by now.
There’s also a big difference between taking a PPI daily for years and using it only when you need it. Some people learn to recognize triggers—spicy food, stress, lying down after dinner—and manage symptoms without daily meds. Studies show that over half of people who try to stop PPIs successfully, especially with a slow taper and support from their doctor. The key is planning: don’t just quit. Talk to your provider about a schedule to reduce your dose over weeks, maybe switching to every-other-day use first. Keep a symptom diary. Note what you eat, when you feel burning, and how you sleep. That data helps you and your doctor decide if the PPI is still necessary.
What you’ll find in the posts below aren’t just general tips—they’re real, practical stories and science-backed strategies from people who’ve been there. From how to handle rebound acid without going back on PPIs, to why some people need to switch to H2 blockers instead, to how to spot when your stomach issues might be something else entirely. You’ll also see how other medications, like NSAIDs or antidepressants, can make acid reflux worse, and what to do about it. This isn’t about fear. It’s about empowerment. You don’t have to live with a daily pill if you don’t need it. The question is: are you ready to find out if you still do?
Proton Pump Inhibitors: Long-Term Risks and When to Stop
Proton pump inhibitors (PPIs) help with heartburn, but long-term use can cause low magnesium, bone fractures, and vitamin B12 deficiency. Learn when to stop and how to do it safely.





