tinea versicolor treatment
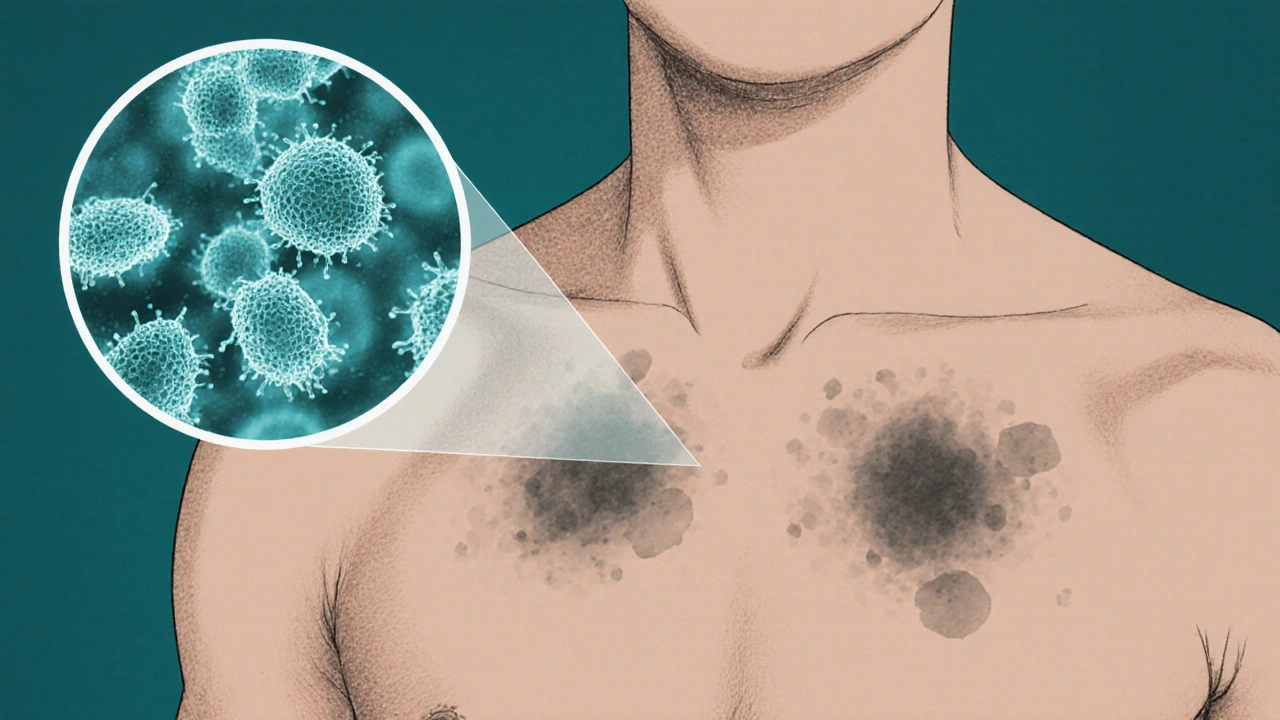
When you’re looking for effective tinea versicolor treatment, the first step is understanding the cause. tinea versicolor treatment, the set of methods used to clear the yeast‑like skin infection that causes tan‑colored patches. Also known as pityriasis versicolor, it works by eliminating the skin fungus, a Malassezia yeast that lives on the surface of the skin and can overgrow under certain conditions that leads to discoloration. The process encompasses both topical and oral antifungal medication, and requires accurate diagnosis to choose the right approach. In short, the fungus influences the choice of therapy, and proper diagnosis sets the stage for success.
Key considerations for choosing treatment
Accurate diagnosis usually comes from a dermatology assessment, where a professional examines the patches, sometimes using a Wood's lamp to confirm the presence of the yeast. The dermatologist will weigh factors like the extent of the rash, how long it’s been present, and any previous attempts at treatment. This evaluation determines whether a simple over‑the‑counter option will work or if stronger prescription therapy is needed. Knowing the severity helps avoid under‑treating a stubborn infection or over‑using potent drugs.
For most mild to moderate cases, antifungal medication, agents such as ketoconazole, selenium sulfide, or zinc pyrithione that kill or inhibit the growth of the skin fungus comes in the form of creams, lotions, shampoos, or soaps. Topical creams are easy to apply, work quickly on visible patches, and have minimal side effects. Shampoos and body washes can treat larger areas or prevent re‑infection by reducing the yeast load on the scalp and torso. Choosing the right product often hinges on where the rash appears and personal preference for a cream versus a wash.
When the infection covers a wide area, recurs often, or doesn’t respond to topicals, doctors may prescribe an oral antifungal. Pills like itraconazole or fluconazole travel through the bloodstream to reach deeper layers of skin where the yeast can hide. Oral therapy typically runs for a few weeks and can clear the infection more completely, but it requires monitoring for liver function and potential drug interactions. Understanding the benefits and risks helps patients decide if a short course of oral medication is worth the added caution.
Beyond medicines, lifestyle tweaks boost results and keep the fungus from coming back. Keeping the skin dry, avoiding heavy oily lotions, and wearing breathable fabrics reduce the environment the yeast loves. Limiting excessive sun exposure can also help, as UV light may trigger pigment changes that make the rash more noticeable. With a clear diagnosis, the right medication, and simple daily habits, you’ll be set to clear up the patches and prevent future flare‑ups. Below you’ll find a collection of articles that dive deeper into specific creams, prescription options, and practical tips, so you can pick the exact solution that fits your situation.
Self‑Care Tips for Managing Fungal Skin Discoloration
Learn how to blend medical treatment with self‑care habits-like gentle cleansing, sunscreen, probiotics, and stress management-to effectively treat and prevent fungal skin discoloration.





