Switch Generic to Brand: When It Makes Sense and When It Doesn't
When you switch generic to brand, the process of changing from a lower-cost generic drug to its original, patent-protected version. Also known as brand substitution reversal, it’s something many people consider after noticing side effects, inconsistent results, or just plain distrust in the cheaper version. The truth? For most drugs, generics work just as well. But not always. And that’s where things get messy.
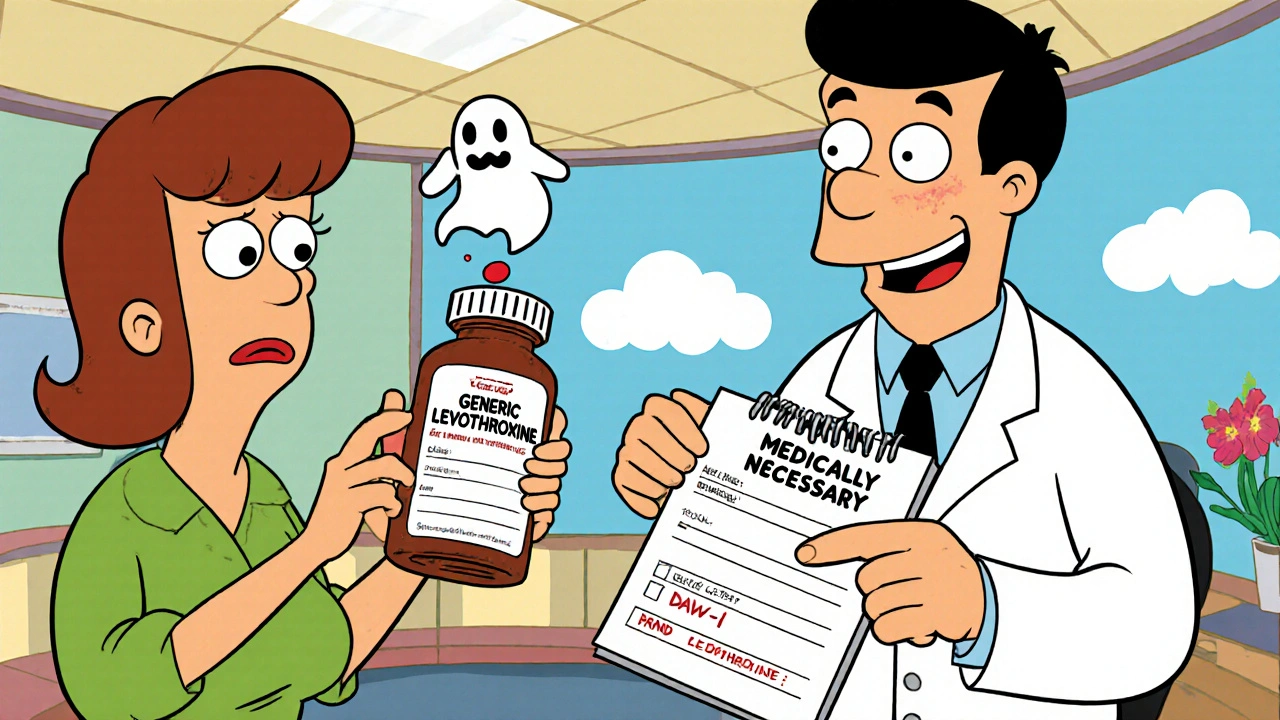
Take antidepressants, medications like sertraline or amitriptyline used to treat depression and nerve pain. Some patients swear their generic Zoloft doesn’t help as much as the brand. Is that placebo? Sometimes. But in rare cases, differences in fillers, coatings, or absorption rates can change how the drug behaves in your body. The same goes for thyroid meds, like levothyroxine, where even tiny variations in bioavailability can throw off hormone levels. One study from the FDA found that while generics must be within 80–125% of the brand’s absorption, that range still leaves room for noticeable differences in sensitive patients.
Then there’s the cost. Generic drugs cut prices by 80% or more. But if you’re on a tight budget and your generic gives you headaches, dizziness, or weird mood swings, switching back might be the only way to feel normal again. That’s not vanity—it’s functionality. People with chronic conditions, like epilepsy, heart disease, or autoimmune disorders, often need rock-solid consistency. A 5% variation in blood levels might mean the difference between staying in remission or ending up in the ER.
But here’s the catch: most of the time, switching back isn’t necessary. The FDA requires generics to meet the same standards as brands. If your generic works fine, there’s no reason to pay more. The real issue? Marketing. Big pharma spends billions convincing you that brand = better. But if your doctor says the generic is safe and effective, trust them. Unless you’ve personally noticed a drop in how you feel, you’re probably paying for a logo, not better medicine.
Still, if you’ve tried the generic and it didn’t sit right—itchy skin, strange fatigue, worse anxiety—talk to your doctor. Don’t just quit. Don’t just switch blindly. Ask for a trial. Ask for a prescription for the brand. Ask for a blood test if it’s something like warfarin or thyroid meds. Some pharmacies even let you return a generic if it doesn’t work, and your insurance might cover the brand if you document the issue.
What you’ll find below are real stories from people who made the switch—from going back to brand-name drugs after bad reactions, to staying on generics and saving hundreds a month. Some switched because of drug interactions, like how certain generics reacted poorly with blood pressure meds or antidepressants. Others switched because their body just didn’t respond. And a few realized they never needed to switch at all.
How to Switch Back from a Generic to a Brand Medication Safely
Switching back from a generic to a brand-name medication can be necessary for safety, but it requires medical documentation, insurance approval, and careful monitoring. Learn the steps to do it right.




