Autoimmune Diseases: What They Are and How to Live With Them
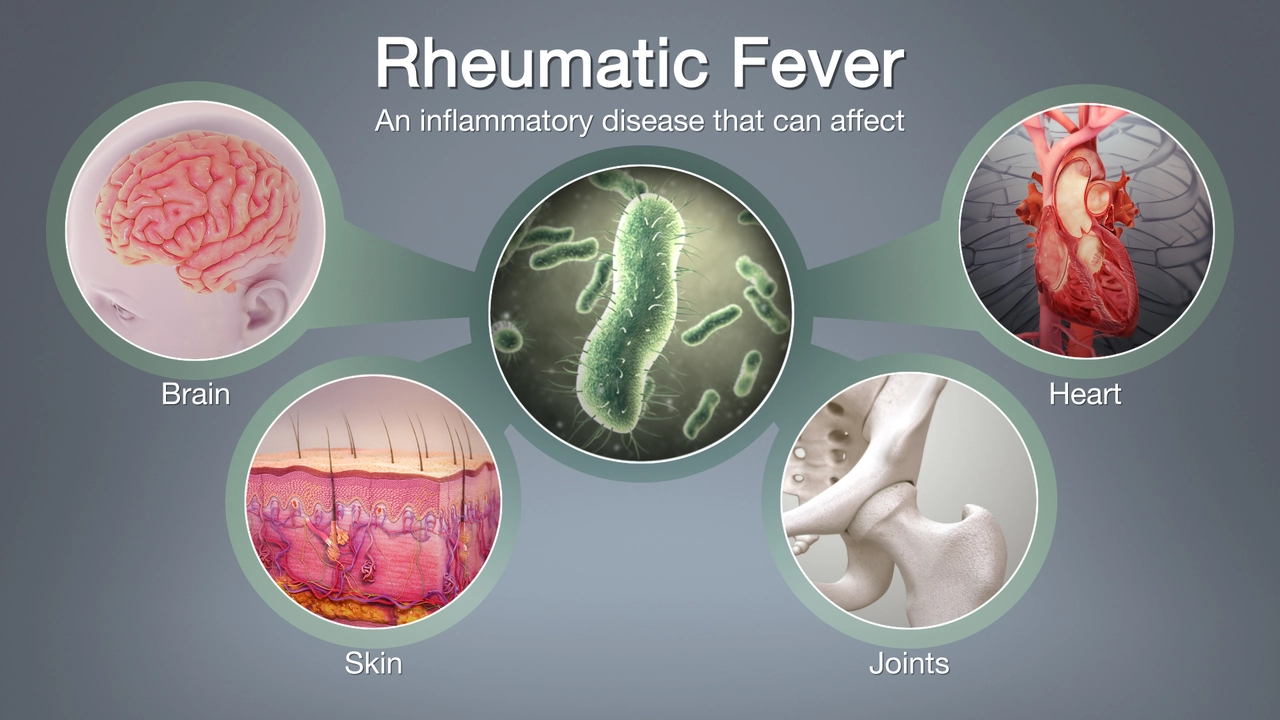
If your body’s defense squad starts attacking you instead of protecting you, you’re looking at an autoimmune disease. It’s not a single illness – it’s a whole family of conditions where the immune system goes rogue. People often think it only affects older folks, but anyone can develop one. Knowing the basics helps you spot problems early and get the right help.
Common Symptoms & Warning Signs
The symptoms overlap a lot because many autoimmune diseases target similar tissues. Fatigue that won’t quit, joint pain, muscle aches, and unexplained fevers are front‑line clues. Skin rashes, especially on sun‑exposed areas, can hint at lupus, while tingling or numbness might point to multiple sclerosis. If you notice a new pattern of swelling or stiffness that lasts more than a few weeks, it’s worth getting checked.
Doctors use blood tests for markers like ANA (antinuclear antibodies) and CRP (C‑reactive protein) to confirm an autoimmune response. Imaging studies, such as MRIs, help when the nervous system is involved. The key is not to self‑diagnose but to bring a detailed symptom list to your appointment.
Treatment & Everyday Management
There’s no one‑size‑fits‑all cure, but treatments can calm the immune attack. Anti‑inflammatory drugs, steroids, and newer biologic agents are common prescriptions. Many patients start with low‑dose medicines and adjust as needed under a doctor’s watch.
Lifestyle tweaks make a big difference. A balanced diet rich in omega‑3 fatty acids—think fish, walnuts, flaxseed—can reduce inflammation. Regular gentle exercise, like walking or yoga, helps keep joints flexible without overloading them. Stress is a hidden trigger; mindfulness, breathing exercises, or short daily breaks can lower flare‑ups.
Sleep matters too. Aim for 7‑9 hours of quality rest; poor sleep fuels fatigue and inflammation. If you’re on medication, never stop it abruptly—talk to your healthcare provider before any changes.
Support networks are gold. Online forums, local groups, or a trusted friend who gets what you’re dealing with can lift morale when symptoms flare. Sharing tips on diet, coping strategies, and doctor experiences creates a community of practical help.
If you suspect an autoimmune disease, schedule a visit sooner rather than later. Early diagnosis often leads to milder treatment plans and better long‑term outcomes. Keep a symptom journal, stay curious about how your body reacts, and partner with a knowledgeable clinician.
Living with an autoimmune condition isn’t a life sentence; it’s a call to listen to your body and make smart choices every day. With the right medical care, diet tweaks, stress control, and community support, you can keep symptoms in check and enjoy a full, active life.
The connection between skin irritations and autoimmune diseases.
In my recent exploration, I've discovered a fascinating link between skin irritations and autoimmune diseases. Autoimmune diseases can lead to skin issues as the immune system mistakenly attacks the body, affecting the skin too. Common skin irritations like psoriasis and lupus are often associated with these diseases. These conditions cause the skin to become inflamed, red, itchy, and sometimes painful. It's crucial to understand that if you're dealing with persistent skin irritations, it might be more than just a skin issue but an underlying autoimmune disease.





