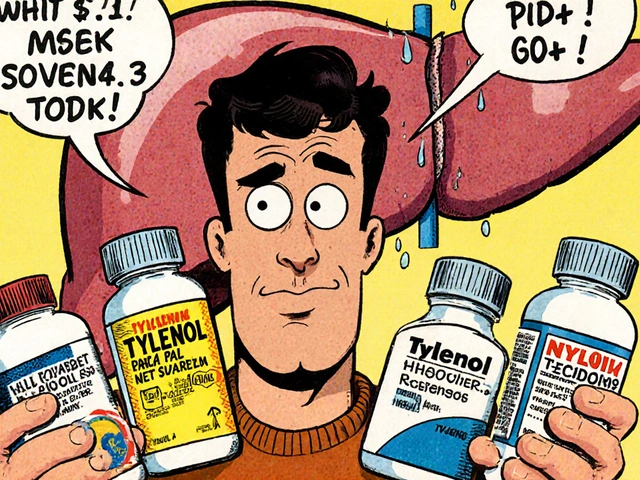
Every year, thousands of people end up in the hospital with severe liver damage-not from alcohol, not from viral hepatitis, but from something they thought was safe: acetaminophen. It’s in painkillers, cold medicines, sleep aids, and even some prescription opioids. The problem? Most people don’t realize they’re taking multiple doses at once. And when they do, their liver can’t keep up.
Why Combination Products Are Dangerous
Acetaminophen, also known as paracetamol, is one of the most common pain relievers in the world. It’s in Tylenol, Excedrin, and dozens of other brands. But it’s also hidden in prescription painkillers like Vicodin (hydrocodone/acetaminophen), Percocet (oxycodone/acetaminophen), and others. These are called combination products because they mix acetaminophen with another drug-usually an opioid-to treat moderate to severe pain. The danger isn’t the opioid. It’s the acetaminophen. Many patients take their prescription painkiller as directed, then reach for a cold medicine or headache pill later in the day. They don’t see the acetaminophen on the label, or they assume it’s safe because it’s "over-the-counter." But each pill adds up. The maximum safe daily dose for adults is 4,000 milligrams. One Vicodin tablet contains 325 mg. That means you can hit the limit after just 12 pills. And if you’re also taking a cold medicine with 650 mg of acetaminophen per dose? You’re already over the edge. In 2011, the FDA found that acetaminophen was the top cause of acute liver failure in the U.S., and nearly half of those cases came from unintentional overdose of combination products. Even today, 27% of all acetaminophen-related liver injuries are from people who didn’t realize they were taking too much.How Acetaminophen Damages the Liver
Your liver normally breaks down acetaminophen safely using two main pathways: glucuronidation and sulfation. But when you take too much, those pathways get overwhelmed. The excess acetaminophen gets processed by a different enzyme-CYP2E1-which creates a toxic byproduct called NAPQI. Under normal conditions, your liver uses glutathione to neutralize NAPQI. But when glutathione runs out, NAPQI starts attacking liver cells. It damages mitochondria, causes oxidative stress, and triggers cell death. This isn’t slow damage. It can happen within hours. And it doesn’t always come with warning signs. Many people feel fine until their liver enzymes spike, sometimes days after taking the last pill. By then, it’s often too late for simple fixes.What the FDA Did-and What’s Still Missing
In 2011, the FDA stepped in. They forced manufacturers to cap acetaminophen in prescription combination products at 325 mg per tablet or capsule. That rule took full effect in 2014. The goal? To make it harder to accidentally overdose. It helped. Unintentional overdoses dropped by 29% after the change, according to the Institute for Safe Medication Practices. But the problem didn’t disappear. Why? Because the same risk exists in over-the-counter products. Tylenol Extra Strength still has 500 mg per pill. Extra Strength Cold & Flu has 325 mg per caplet. And many people still don’t check labels. Even worse, some people think "natural" or "prescription-only" means safer. It doesn’t. A 2022 study in Hepatology found that nearly 70% of acetaminophen-related liver injuries from combination products were unintentional. People weren’t trying to hurt themselves. They just didn’t know what they were taking.
How to Protect Yourself
If you’re prescribed a combination painkiller, here’s what you need to do right now:- Check every medication you take-prescription or OTC-for acetaminophen. Look for "APAP," "acetaminophen," or "paracetamol" on the label. Don’t rely on brand names.
- Add up your total daily dose. If you’re taking two Vicodin pills (325 mg each) and one Tylenol (500 mg), you’re already at 1,150 mg. That’s almost a third of your daily limit. Add a NyQuil, and you’re over.
- Never mix painkillers. If you’re on a prescription combo product, avoid all other acetaminophen-containing products. That includes cold medicine, allergy pills, sleep aids, and even some migraine treatments.
- Set a daily limit of 3,000 mg if you drink alcohol, have liver disease, or are underweight. Your liver’s ability to detoxify acetaminophen is already reduced. The 4,000 mg limit doesn’t apply to you.
- Ask your pharmacist. They’re trained to catch these interactions. Don’t be shy. Say: "I’m on hydrocodone/acetaminophen. What else can I take for fever or headaches?"
What Your Doctor Should Be Doing
Doctors aren’t always the best at explaining this. A 2022 Johns Hopkins study found that even after counseling, only 62% of patients understood their acetaminophen risk. That’s not good enough. The CDC now recommends that electronic health records (EHRs) track acetaminophen doses across all prescriptions. Most major systems like Epic now do this. But if your doctor doesn’t mention it, ask: "Is there acetaminophen in this? How much? Can I take something else for pain?" Some clinics now use printed cards or apps to help patients track daily intake. The Acetaminophen Hepatotoxicity Prevention Consortium developed a smartphone app that scans medication barcodes and warns you when you’re approaching the limit. Beta testing showed 89% accuracy across 150 products. If your doctor doesn’t know about it, ask if they can recommend one.What to Do If You Think You’ve Taken Too Much
If you suspect you’ve taken more than 4,000 mg of acetaminophen in 24 hours-even if you feel fine-go to the ER immediately. Don’t wait for symptoms. Nausea, vomiting, and right-side abdominal pain often appear late. By then, liver damage may already be advanced. The antidote is N-acetylcysteine (NAC). It works by replenishing glutathione and protecting liver cells. It’s most effective if given within 8 hours of overdose, but it still helps up to 48 hours later. The Rumack-Matthew nomogram, used in hospitals, tells doctors whether you need NAC based on your blood level and when you took the last dose. Newer treatments are emerging. In 2021, the FDA approved fomepizole as an adjunct to NAC. It blocks the enzyme that turns acetaminophen into NAPQI. In trials, it reduced severe liver injury by 32% when given within 12 hours. But NAC is still the gold standard. Don’t delay.






malik recoba
November 19, 2025 AT 15:20man i just took tylenol for my headache and didn't even think about my vicodin from last week. i'm gonna check every bottle in my cabinet right now. thanks for the wake-up call.
Sarbjit Singh
November 19, 2025 AT 15:45so true bro 😅 i live in india and people here mix paracetamol with everything - cold, fever, even stress 😅 i told my uncle he was taking 5 pills a day and he said 'but it's just paracetamol!' 😭
Angela J
November 20, 2025 AT 10:05you know what's really scary? the fact that the FDA only capped it in prescriptions… but OTC is still 500mg per pill. they’re letting us kill ourselves slowly. big pharma doesn’t care. they just want you hooked on painkillers and then fix the damage later. it’s a money machine.
Sameer Tawde
November 21, 2025 AT 11:43simple rule: if it’s not just acetaminophen, treat it like a bomb. read the label. write it down. ask your pharmacist. you’re not being paranoid - you’re being smart.
Jeff Hakojarvi
November 21, 2025 AT 18:19the 3,000 mg limit for people who drink or have liver issues is CRUCIAL. i had a friend who drank one beer a night and took 4 tylenol - ended up in the hospital. liver enzymes were through the roof. doc said if he’d waited another 6 hours, he’d have needed a transplant. don’t be that guy.
Timothy Uchechukwu
November 21, 2025 AT 20:18Ancel Fortuin
November 23, 2025 AT 00:08oh please. the real problem? doctors don’t even warn you. i’ve been on vicodin for years and no one ever said 'hey don’t take nyquil.' and now you want us to read tiny print on bottles? yeah right. this is just another way to make us feel guilty while they get richer.
Hannah Blower
November 23, 2025 AT 21:39the tragic irony here is that acetaminophen isn't toxic - it's a symptom of our collective epistemic collapse. we’ve outsourced our cognitive labor to pharmaceutical marketing, and now we’re paying the price in hepatic necrosis. the real villain isn't the drug - it's the commodification of bodily autonomy.
deepak kumar
November 25, 2025 AT 02:35in india, we call it paracetamol and think it's harmless. but this post opened my eyes. i asked my cousin who takes it for fever and headaches - she was taking 3 tablets a day plus cold syrup. i showed her the label. she cried. now she uses only one. small change, big difference.
Dave Pritchard
November 25, 2025 AT 07:40my mom took 2 tylenol and a cold med after surgery. she didn't feel anything until she turned yellow. spent 3 days in ICU. now she carries a little card in her wallet with all her meds and the acetaminophen limit. best thing she ever did.
kim pu
November 26, 2025 AT 10:06let’s be real - the FDA’s 325mg cap is a performative gesture. they didn’t reduce the daily limit. they didn’t mandate clear warnings on OTC packaging. they didn’t ban combo products. they just made it slightly harder to OD in one go. meanwhile, the marketing still screams 'safe!' 'gentle!' 'doctor recommended!' it’s psychological gaslighting.
Gregory Gonzalez
November 27, 2025 AT 13:38you people are so easily manipulated. if you can’t read a label, maybe you shouldn’t be allowed to own a phone, let alone a medicine cabinet. this isn’t a public health crisis - it’s a failure of basic literacy. blame the people, not the system.
Ronald Stenger
November 28, 2025 AT 13:55acetaminophen? more like american pharmaceutical propaganda. we’re being fed this narrative that 'over-the-counter' means 'safe' - but in reality, it’s just cheaper for them to let us overdose than to make safer alternatives. this is capitalism at its finest: profit from your suffering.
Samkelo Bodwana
November 30, 2025 AT 00:05you know, i used to think this was just a u.s. problem - but after reading this, i realize it’s global. here in south africa, people buy paracetamol in bulk from street vendors, mix it with traditional herbs, and don’t know the dosage. i’ve seen it. the liver failure rates are rising. maybe we need community health workers going door to door, not just app warnings. education has to be human, not digital. and yes, i know this sounds idealistic - but what’s the alternative? more obituaries?