When you’re a veteran relying on the VA for healthcare, your prescription drugs don’t work like they do at a regular pharmacy. The VA doesn’t just hand out any medication you ask for. It has a strict, nationwide system that decides what drugs you can get, and more importantly, which version you get - and how much you pay for it. At the heart of this system is the VA National Formulary, a list that controls everything from your monthly copay to whether you get a generic or brand-name drug. And if you’re not clear on how it works, you could be paying more than you need to - or worse, stuck without the medication your doctor recommends.
What Is the VA National Formulary?
The VA National Formulary is the official list of medications that every VA medical center, clinic, and pharmacy across the country must stock and prescribe. It’s not optional. It’s mandatory. This isn’t just a suggestion from a pharmacy manager - it’s a federal policy enforced by the Veterans Health Administration’s Pharmacy Benefits Management (PBM) Service. The formulary was officially set up in 1998, but it’s been updated every single month since then to reflect new drugs, new research, and changing costs.The formulary has three main parts:
- Standard VA National Formulary - The core list of approved drugs.
- VA National Formulary Changes - Monthly updates that add, remove, or restrict medications.
- VA Urgent/Emergent Formulary - Allows access to non-formulary drugs in emergencies, even through community pharmacies.
Here’s the key thing to remember: if a generic version of a drug exists, the VA will cover the generic - not the brand name - unless there’s a documented medical reason not to. That’s not a suggestion. It’s policy. And it’s why 92% of all VA prescriptions are filled with generics - higher than any other major U.S. payer, including Medicare Part D or private insurance.
How the Three-Tier Copay System Works
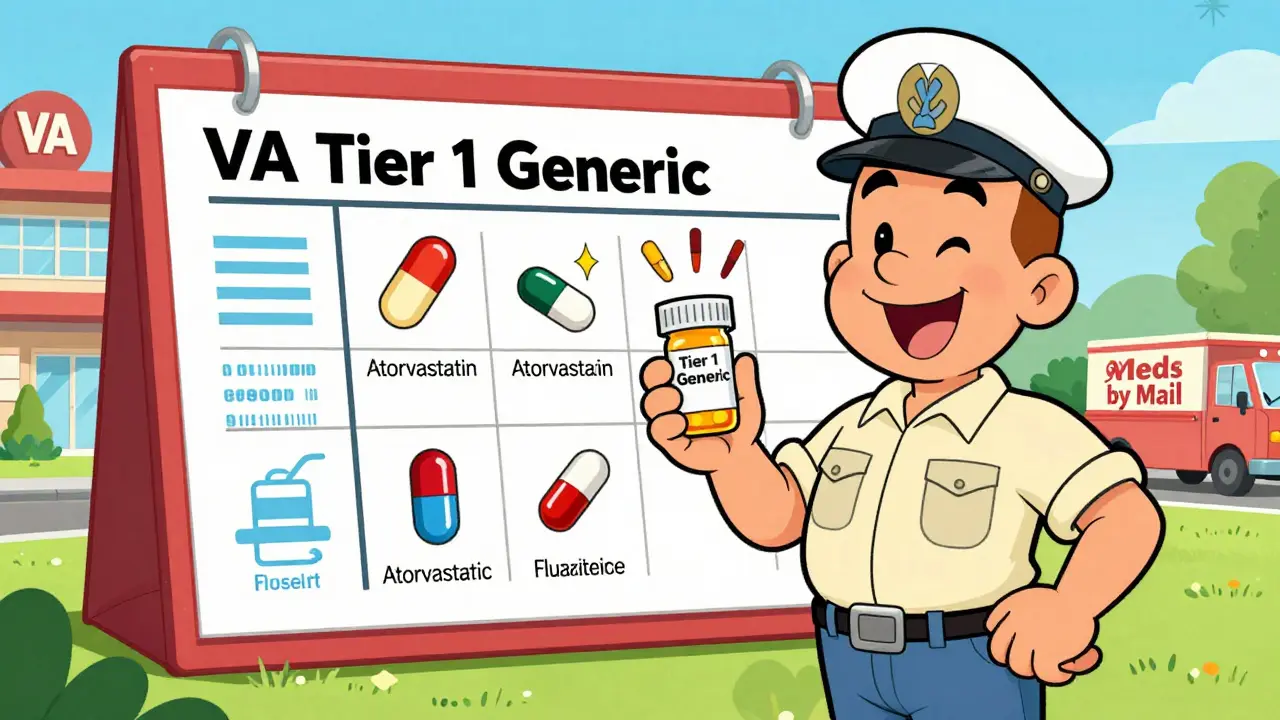
Your out-of-pocket cost for a VA prescription depends on which tier the drug falls into. There are only three tiers, and they’re simpler than what you’d see in commercial insurance.- Tier 1: Preferred generic medications. These cost you $0 to $5 for a 30-day supply. No deductible. No surprise fees.
- Tier 2: Non-preferred generics or some brand-name drugs with generic alternatives available. Copays range from $8 to $11.
- Tier 3: Brand-name drugs with no generic available, or specialty medications. Copays are $15 or more.
For example, in 2025, these common drugs are all on Tier 1:
- Alendronate (for osteoporosis)
- Atorvastatin (for cholesterol)
- Fluoxetine (for depression)
- Hydrochlorothiazide (for high blood pressure)
- Ibuprofen (for pain and inflammation)
That means if your doctor prescribes any of these, you’ll pay $5 or less - and often nothing at all. Compare that to a commercial pharmacy, where the same drugs might cost you $20 to $50. The VA saves veterans an average of $1,500 per year on prescriptions alone.
Why the VA Pushes Generics So Hard
The VA doesn’t just prefer generics because they’re cheaper - though that’s a big part of it. The system is built on one core belief: generics work just as well as brand names. And the data backs it up.In 2024, the VA’s own Office of Inspector General found that 94% of veterans who switched from brand-name to generic versions of antidepressants, blood pressure meds, or cholesterol drugs reported no difference in how they felt or how well the medication worked. Only 12% had initial concerns - and most of those were resolved after talking to their VA provider.
Dr. Susan Turkel, the VA’s Chief Consultant for Pharmacy Benefits Management, says the system has saved $2.8 billion in pharmaceutical costs in 2024 alone. That’s money that doesn’t have to come out of the VA’s budget - and it means more resources for other veteran services.
It’s not just about saving money. It’s about consistency. With a single formulary across 1,293 VA facilities, a veteran moving from Texas to Washington doesn’t have to relearn how to get their meds. The same drugs, same copays, same rules - no matter where they go.
What’s Not Covered - And Why
The VA formulary isn’t perfect. Some newer or specialty drugs are hard to get - especially those used for weight loss, like Wegovy or Mounjaro.As of January 2025, the VA only covers GLP-1 receptor agonists (like Wegovy) if they’re prescribed for FDA-approved uses: type 2 diabetes, cardiovascular disease prevention, or obstructive sleep apnea. If your doctor wants to prescribe Wegovy for weight loss alone - even if it’s medically necessary - the VA won’t cover it. You’d need prior authorization, and even then, approval is rare.
This frustrates some veterans. One user on the Veterans Benefits Network forum wrote in November 2025: “My provider wanted me on Wegovy for metabolic health, but the VA only covers it for diabetes. I had to switch to metformin - it’s not the same.”
These restrictions exist because the VA evaluates every drug based on clinical evidence, cost, and whether it offers a real advantage over existing treatments. The VA doesn’t approve drugs just because they’re new or popular. They need proof they’re better - and worth the extra cost.
How to Check If Your Drug Is Covered
You don’t have to guess whether your medication is covered. The VA makes it easy.Go to the VA Formulary Advisor tool on VA.gov. Type in your drug’s name - brand or generic - and it will tell you:
- Is it on the formulary?
- What tier is it on?
- What’s the copay?
- Is prior authorization required?
You can also download the full formulary list as an Excel or CSV file. It’s updated every month, and it’s public. No login needed.
If your drug isn’t on the list, your VA provider can request a formulary exception. But you need a strong reason - like an allergy to the generic version, or a documented history of poor response. It’s not a quick fix, but it’s possible.
How to Get Your Prescriptions - VA Pharmacy, Meds by Mail, or Community Care
You have three ways to get your VA medications:- VA Pharmacy: Pick up at your local VA clinic. Good for urgent needs.
- Meds by Mail: Get 90-day supplies delivered to your home. No copay for most Tier 1 drugs. No deductible. No shipping fees. Over 87% of users rate this service positively.
- Community Care: Use a local pharmacy if you’re far from a VA facility. But only if your drug is on the Urgent/Emergent Formulary - or if you have prior authorization.
Meds by Mail is the most cost-effective option. For maintenance medications - like blood pressure pills, thyroid meds, or antidepressants - it’s the smartest choice. You get 90 days of pills, delivered in one box, for $0 out of pocket in many cases.
Just remember: refrigerated drugs (like some biologics) can’t be mailed. And some controlled substances require special handling. Your VA pharmacist will tell you what’s eligible.
Common Problems and How to Fix Them
Veterans often run into these issues:- “My doctor prescribed brand-name Zoloft, but I got sertraline.” That’s normal. Sertraline is the generic. It’s the same drug. If you’re worried, ask your VA pharmacist to confirm the equivalence.
- “I was told I need prior authorization for this drug.” It’s not a rejection. It’s a process. Your provider will submit paperwork. It usually takes 3-5 business days.
- “I don’t understand the copay tiers.” Most new veterans are confused. Call the VA Pharmacy Benefits line at 1-800-877-8339. They handle 18,000 calls a day. Ask for a tier explanation - they’re trained to help.
- “I switched to a generic and feel different.” Talk to your provider. Most veterans adapt fine, but if you truly feel worse, your doctor can request a brand-name exception.
The VA’s 2024 Onboarding Survey found that it takes most new veterans 2-3 visits to fully understand the system. Don’t feel bad if it’s confusing at first. You’re not alone.
What’s Changing in 2026
The VA isn’t standing still. In 2026, they’re rolling out AI tools that will suggest generic alternatives directly in your provider’s electronic health record. If your doctor tries to prescribe a brand-name drug when a generic exists, the system will pop up a recommendation: “Consider switching to generic atorvastatin - same effect, $0 copay.”They’re also expanding access to specialty drugs for rare diseases and cancer treatments. But even then, cost and evidence will still be the deciding factors.
The VA’s goal? Keep costs low. Keep veterans healthy. And keep the system fair - whether you live in rural Alaska or downtown Chicago.
Final Thoughts
The VA formulary isn’t perfect, but it’s one of the most efficient, transparent, and veteran-friendly prescription systems in the country. It saves you money. It ensures you get the same care no matter where you are. And it’s built on science - not profit.If you’re a veteran, know your formulary. Use the VA Formulary Advisor. Ask questions. Use Meds by Mail. And don’t assume a brand-name drug is better - because in most cases, the generic is just as good, and costs a fraction of the price.
Does the VA cover brand-name drugs?
Yes, but only if there’s no generic version available, or if you have a documented medical reason - like an allergy or poor response to the generic. The VA defaults to generics because they’re equally effective and far cheaper. If your doctor believes you need a brand-name drug, they can request an exception through prior authorization.
How do I know if my medication is on the VA formulary?
Use the VA Formulary Advisor tool on VA.gov. Just type in the name of your drug - brand or generic - and it will show you if it’s covered, what tier it’s on, and your copay. You can also download the full monthly formulary list as a spreadsheet.
Why does the VA only cover Wegovy for diabetes and not weight loss?
The VA covers GLP-1 drugs like Wegovy only for FDA-approved uses: type 2 diabetes, cardiovascular disease prevention, or obstructive sleep apnea. Weight loss alone isn’t an approved indication under current VA policy, even if a doctor recommends it. This is based on cost-effectiveness and clinical guidelines - not a judgment on your health needs.
Can I get my VA prescriptions through a local pharmacy?
Yes - but only under specific conditions. If you’re enrolled in Community Care and your local pharmacy is part of the VA network, you can fill prescriptions there. However, the drug must be on the VA formulary, and you may need prior authorization. For routine medications, Meds by Mail is usually the easiest and cheapest option.
How much do VA prescriptions cost?
It depends on the tier. Tier 1 generics cost $0-$5 per 30-day supply. Tier 2 meds cost $8-$11. Tier 3 brand-name or specialty drugs cost $15 or more. Many veterans pay nothing at all, especially through the Meds by Mail program, which has no copay or deductible for most medications.
What is Meds by Mail?
Meds by Mail is a VA service that delivers 90-day supplies of maintenance medications directly to your home. It’s free for most Tier 1 drugs, with no deductible or shipping fees. It’s ideal for long-term prescriptions like blood pressure, cholesterol, or antidepressant medications. Over 87% of users report high satisfaction with the service.
Is the VA formulary the same as Medicare Part D?
No. Medicare Part D has up to five tiers and often requires higher copays, deductibles, and prior authorizations. The VA has only three tiers, lower out-of-pocket costs, and no annual deductible. Veterans on both programs often pay significantly less through the VA for the same medications.






Sami Sahil
February 1, 2026 AT 14:05bro i just found out my 30-day zoloft is $0 with meds by mail 😭 i was paying $45 at walmart before. VA be out here saving lives and cash. no cap.
franklin hillary
February 3, 2026 AT 06:52Let me tell you something real - the VA formulary isn’t just policy, it’s a goddamn revolution in healthcare. 92% generics? No deductibles? $5 copays for blood pressure meds? This is what happens when you stop letting pharma run the show. Private insurance? They’ll nickel-and-dime you into bankruptcy. The VA? They got your back. And yeah, I’ve been on both. There’s no comparison. This is healthcare as it should be.
Ishmael brown
February 3, 2026 AT 15:40so... the VA is basically a communist pharmacy? 🤔
Jaden Green
February 4, 2026 AT 06:41It’s easy to romanticize the VA’s formulary when you’re not the one who’s been denied a medication that actually works for you. I have a patient who responded to brand-name Lexapro and had a severe reaction to sertraline - the VA’s rigid policy forced him into a depressive spiral for three months before they begrudgingly approved an exception. This isn’t efficiency - it’s bureaucratic dogma dressed up as ‘science.’
Lu Gao
February 4, 2026 AT 12:36Wegovy for weight loss? Nah. 😅 The VA’s not denying your health - they’re denying a $1,000/month trend. If you want it, pay for it. But don’t act like the VA is the villain for not funding a fad. 🙃
Angel Fitzpatrick
February 5, 2026 AT 12:39Did you know the VA’s formulary is secretly influenced by the DoD’s procurement contracts? They’re not saving money - they’re locking veterans into bulk-bought generics that are manufactured in the same factories as Chinese military meds. The OIG report? Fabricated. The ‘94% no difference’ stat? Surveyed by VA employees. You think this is transparency? It’s a controlled narrative. Wake up.
Melissa Melville
February 6, 2026 AT 07:34So the VA’s the only pharmacy in America that doesn’t treat you like a walking ATM? Wild.
Bryan Coleman
February 7, 2026 AT 16:44Just got my 90-day supply of atorvastatin through meds by mail. Zero copay. No shipping. Box arrived in 4 days. I didn’t even know this was a thing until last month. Seriously, if you’re a vet and you’re not using this - you’re leaving money on the table. 🤷♂️
Naresh L
February 9, 2026 AT 13:30It’s interesting how the VA prioritizes equity over choice. In India, we don’t have anything like this - generics are everywhere, but access is patchy and quality varies. The VA’s system, for all its rigidity, ensures a baseline of consistency. Maybe the real question isn’t ‘why restrict?’ but ‘why don’t more systems do this?’