Generic Drug Side Effects: What You Need to Know Before Taking Them
When you pick up a generic drug, a non-brand version of a medication that contains the same active ingredient as the original. Also known as generic medication, it works the same way as the brand-name version but costs far less—often 80% cheaper. But just because it’s cheaper doesn’t mean it’s risk-free. Generic drug side effects can be just as real, and sometimes even harder to predict because people assume they’re harmless.
Many people think brand-name drugs are safer or more effective, but that’s not true. The FDA requires generics to match the brand in strength, dosage, and how they work in your body. But here’s what most don’t realize: the inactive ingredients—fillers, dyes, preservatives—can be different. And those can trigger reactions. One person might get a rash from the dye in a generic version of amitriptyline, while the brand version doesn’t bother them. That’s not a flaw in the active drug—it’s a difference in the formulation. These small changes can lead to drug interactions, when two or more medications affect each other’s behavior in your body, especially if you’re taking multiple pills. For example, a generic version of metronidazole might use a different binder that slows absorption, leading to longer exposure and higher risk of nerve damage. Or a generic hydrochlorothiazide might have a different excipient that raises blood pressure in people already on beta-blockers.
adverse drug reactions, unexpected and harmful responses to a medication aren’t rare. They’re common—especially in older adults on multiple meds. The posts below show real cases: nasal sprays causing rebound congestion, antibiotics triggering nerve tingling, and skin creams leading to steroid dependency. These aren’t just side effects—they’re preventable mistakes. Many people don’t know that generic versions of the same drug can come from different manufacturers, and quality can vary by batch. Some generics are made in the same factory as the brand, others aren’t. And if you switch brands mid-treatment, your body might react differently. That’s why tracking what version you’re taking matters. If you start feeling dizzy after switching to a new generic, it’s not "just in your head." It could be the filler.
You don’t need to avoid generics. They’re a smart choice for most people. But you need to be aware. Know the active ingredient. Check the manufacturer. Watch for new symptoms. And don’t assume that because it’s cheap, it’s safe. The posts here cover exactly these risks—from how antidepressants affect your heart to how common painkillers can wreck your liver. You’ll find clear guides on what to watch for, when to call your doctor, and how to avoid the traps most people never see coming. This isn’t about scaring you. It’s about giving you the facts so you can take control.
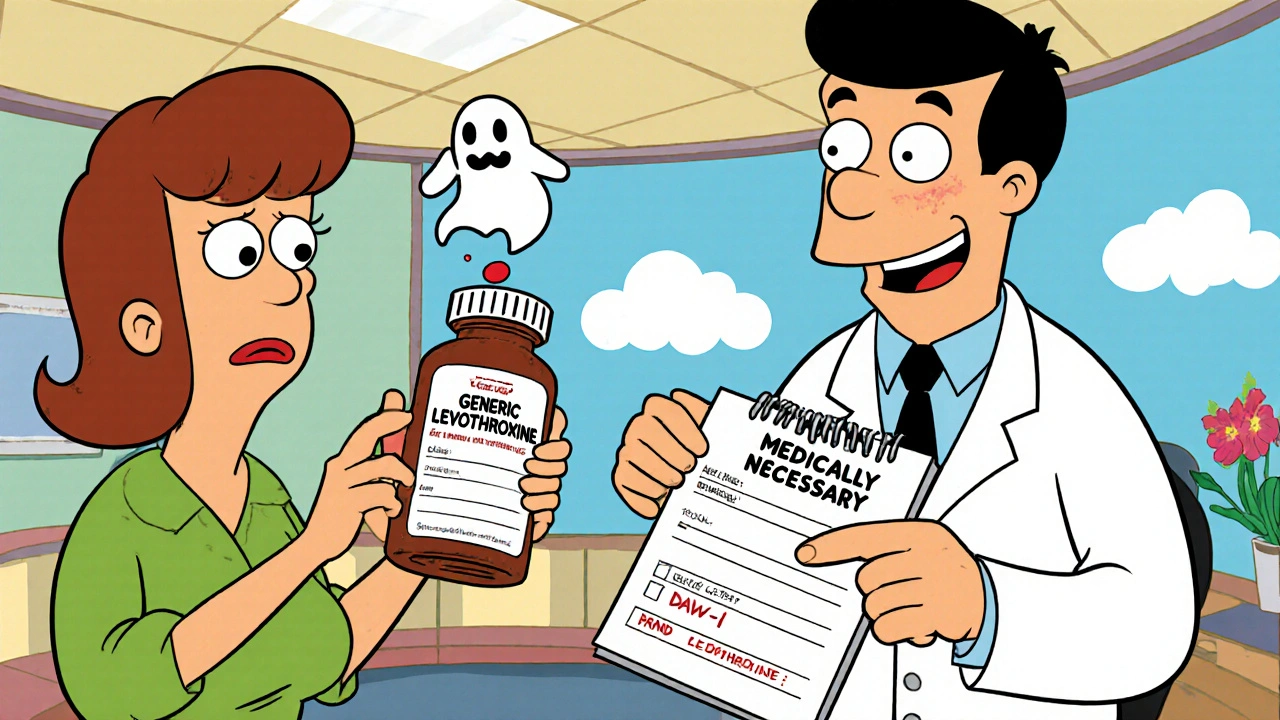
How to Switch Back from a Generic to a Brand Medication Safely
Switching back from a generic to a brand-name medication can be necessary for safety, but it requires medical documentation, insurance approval, and careful monitoring. Learn the steps to do it right.





