Every time you pick up a new prescription, there’s a small paper insert tucked inside the bottle. It’s easy to ignore. But that little guide could be the difference between staying safe and ending up in the hospital. Medication interactions are one of the most common causes of preventable harm - and they’re not always obvious. A common painkiller, a daily vitamin, even a glass of grapefruit juice can turn a safe drug into a dangerous one. Learning how to read those warnings isn’t just helpful - it’s necessary.
Where to Find Interaction Warnings
Interaction warnings don’t hide. They’re in clear, labeled sections. For prescription drugs, look for the Drug Interactions section - usually Section 7 in the full prescribing info. For over-the-counter meds, check the Warnings section on the Drug Facts label. These aren’t random notes. They’re required by the FDA to be clear, specific, and standardized.
Some guides use bold text for absolute no-go warnings: "Do not take if you are using...". Others use italics for cautionary advice: "Ask your doctor before use if...". The difference matters. Bold means stop. Italic means pause and ask.
Understanding the Severity Levels
Not all interactions are created equal. Medication guides now use simple, consistent language to tell you how serious a warning is:
- Contraindicated - Don’t take it together. Ever. This could be life-threatening.
- Avoid - Strong risk of serious side effects. Only use if no other option exists and under close supervision.
- Use with Caution - Possible side effects. Your doctor may still prescribe it, but you’ll need monitoring.
- Minor - Low risk. Usually just a tweak in timing or dosage.
These terms were standardized by the FDA in 2024 to cut through confusion. Before this, you might see "significant," "moderate," or "potential" - terms that meant different things to different people. Now, if it says "Avoid," you know it’s serious.
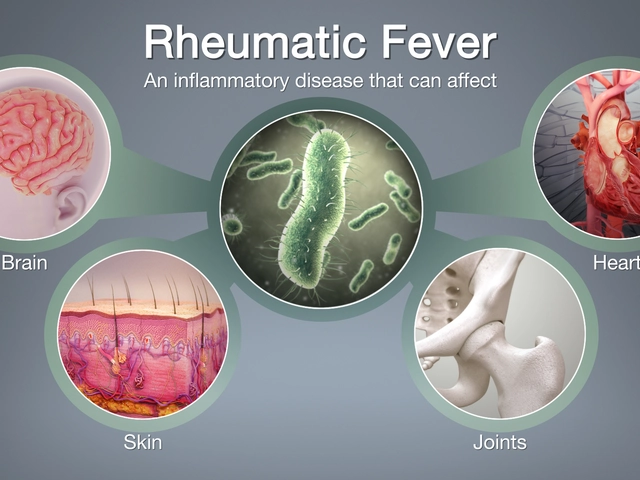
What Makes an Interaction Dangerous?
There are two main ways drugs can clash: through your body’s chemistry or through how they affect your system.
Pharmacokinetic interactions change how your body absorbs, breaks down, or gets rid of a drug. The most common culprit? The CYP3A4 enzyme. It handles about half of all prescription medications. If another drug blocks or speeds up this enzyme, levels of your medication can spike or crash. For example, taking simvastatin (a cholesterol drug) with clarithromycin (an antibiotic) can raise simvastatin levels tenfold - turning a rare risk of muscle damage into a 10x higher chance of serious injury.
Pharmacodynamic interactions happen when two drugs do the same thing to your body - and together, they go too far. Think blood thinners like warfarin combined with NSAIDs like ibuprofen. Both thin your blood. Together, they can increase bleeding risk by up to 100%. That’s why warfarin guides explicitly warn against NSAIDs - and why even one dose can be risky.
Don’t Forget the Hidden Players
Most people think only about prescription drugs. That’s the mistake. Over-the-counter meds, herbal supplements, and even food can trigger dangerous interactions.
According to FDA data, 37% of serious interactions involve OTC drugs or supplements. St. John’s Wort - often taken for mood - can make birth control, antidepressants, and even heart meds stop working. Grapefruit juice? It interferes with more than 85 drugs, including blood pressure pills and statins. One glass can raise drug levels for 24 hours. That’s why warfarin guides say "avoid grapefruit" - but don’t always explain how much is too much. A 2017 study showed just one glass could raise INR (a blood clotting measure) by 1.5 to 2.0 points. That’s enough to trigger bleeding.
Even common vitamins like vitamin K can interfere with warfarin. And don’t assume "natural" means safe. Many supplements aren’t tested for interactions the way prescription drugs are.
How to Use the Guide - A Simple 4-Step Process
Reading the guide isn’t enough. You need to act on it. Here’s how:
- List everything you take - prescriptions, OTC meds, vitamins, herbs, even occasional painkillers. Write down the name, dose, and how often you take it. Most people take 4-5 medications daily, according to the Agency for Healthcare Research and Quality.
- Check each guide - Pull out the interaction section for every drug. Don’t skip the supplements. Use your phone to take a photo of each guide so you can review them later.
- Look for the red flags - Bold text, "Avoid," "Contraindicated," and any mention of bleeding, dizziness, muscle pain, or irregular heartbeat. These aren’t suggestions - they’re warnings.
- Talk to your pharmacist - Pharmacists are trained to spot interactions you might miss. Ask: "Do any of these meds clash?" and "Should I space them out?" Even separating doses by 2-4 hours can cut moderate interaction risks by 60%.
What to Do When You Find a Warning
If you spot a warning you don’t understand, don’t guess. Don’t stop the med on your own. Do this:
- Write down the exact drug names and the warning.
- Call your pharmacist or doctor. Say: "I saw this warning in my guide - what does it mean for me?"
- If the interaction is labeled "Avoid" or "Contraindicated," ask: "Is there a safer alternative?"
- For food interactions, ask: "How much is dangerous? Can I have it at a different time?"
One patient on Reddit avoided serotonin syndrome - a rare but deadly condition - after spotting the warning between sertraline and tramadol. She didn’t ignore it. She called her pharmacist. That’s the move.
What’s Changing - And What to Expect
Medication guides are getting better. Since 2023, new drugs must include a QR code linking to a digital version with voice navigation and interactive warnings. By 2025, all guides will use the same safety language: "Contraindicated," "Avoid," "Use with Caution." This isn’t just paperwork - it’s saving lives.
Studies show these changes work. A 2022 Mayo Clinic pilot found that patients who got personalized digital interaction reports had 42% fewer adverse events. The FDA says standardized guides have cut hospitalizations from drug interactions by 28% since 2010.
But progress isn’t perfect. Only 53% of generic drug guides meet readability standards. Some still use confusing jargon. That’s why your job - reading, asking, verifying - still matters more than ever.
Real Tips That Work
People who stay safe with their meds do three things:
- Keep a running list - digital or paper - updated every time something changes.
- Take photos of every medication guide - so they’re always on their phone.
- Ask the pharmacist every time they pick up a new script: "Is this safe with everything else I take?"
One survey found that 78% of people read their medication guides. But only 32% could correctly identify a major warning. The gap isn’t in the guide - it’s in how we use it.
Don’t assume you know what it means. Don’t assume your doctor already checked. Don’t assume it’s "just a supplement." Every drug - even aspirin - has a story. Learn how to read it.
What should I do if I see a "Contraindicated" warning on my medication guide?
If a warning says "Contraindicated," it means taking the two drugs together could cause serious harm or death. Do not take them together. Call your doctor or pharmacist immediately to ask for a safe alternative. Never stop a prescribed medication without professional advice - but do not combine it with the listed drug until you’ve talked to someone.
Can over-the-counter medicines cause dangerous interactions?
Yes. In fact, 37% of serious drug interactions involve OTC medications or supplements. Common culprits include ibuprofen, naproxen, antacids, St. John’s Wort, and even vitamin K. Always check the "Warnings" section on the Drug Facts label. If you’re taking a prescription drug, assume any OTC product could interfere - and ask your pharmacist before using it.
Why does my medication guide say to avoid grapefruit juice?
Grapefruit juice blocks an enzyme in your gut called CYP3A4, which normally breaks down many drugs. When that enzyme is blocked, your body absorbs much more of the drug than intended. This can lead to dangerous side effects. For example, with statins like simvastatin, grapefruit can raise drug levels by 5 to 15 times. Even one glass can affect you for 24 hours. Avoid grapefruit entirely if your guide says so - no exceptions.
Are generic drugs less safe than brand-name ones when it comes to interactions?
The active ingredient in generic drugs is the same as brand-name, so the interaction risks are identical. But the medication guides for generics often have worse readability - only 53% meet current standards, according to a 2022 study. That means the warnings might be harder to understand. Always compare the generic guide to the brand-name version if you’re unsure. If in doubt, ask your pharmacist to review both.
How can I remember all the interactions I need to watch for?
Keep a simple, updated list of all your medications - including doses and times - and take a photo of each medication guide. Use a notes app or a physical notebook. Review it every time you start a new drug or see a new doctor. Many people who avoid interactions do this. You can also use free online tools like the FDA’s Drug Interaction Checker (updated quarterly) to cross-reference your list. But never rely on apps alone - always confirm with a pharmacist.





prasad gaude
November 25, 2025 AT 11:26Man, I never thought about how grapefruit juice could mess with my meds until my uncle ended up in the ER. Now I keep a little note on my fridge: "NO GRAPES WITH PILLS." It’s weird how something so natural can be so dangerous. We think herbal = safe, but nah, man. Nature don’t care if you’re trying to live.
Srikanth BH
November 25, 2025 AT 13:25This is such a needed post. I used to just toss the insert in the trash. Then my mom had a bad reaction to ibuprofen and her blood thinner. Now I read every single one. Took me 20 years to learn this. Don’t wait like I did.
Jennifer Griffith
November 26, 2025 AT 02:19fridge note? lmao. i just google my meds + grapefruit and hope for the best. also why does everyone act like pharmacists are wizards? they read the same pamphlet i do 😴
Kimberley Chronicle
November 26, 2025 AT 19:43The standardization of interaction terminology by the FDA in 2024 represents a significant paradigm shift in pharmacovigilance communication. The adoption of hierarchical risk descriptors-Contraindicated, Avoid, Use with Caution, Minor-reduces cognitive load and mitigates interpretive variance across patient populations. This is a triumph of regulatory linguistics.
Shirou Spade
November 27, 2025 AT 22:03It’s funny how we treat medicine like it’s a magic spell. You take the pill, the problem disappears. But the body’s not a machine you can just plug things into. Everything’s connected. Even that vitamin you think is harmless? It’s whispering to your liver. You just don’t hear it until it screams.
Pallab Dasgupta
November 28, 2025 AT 02:35YOOOOO I JUST REALIZED I’VE BEEN TAKING ST. JOHN’S WORT WITH MY ANTIDEPRESSANT FOR 3 YEARS 😭😭😭 I’M CALLING MY PHARMACIST RIGHT NOW. THANK YOU FOR THIS POST. I THOUGHT IT WAS JUST "NATURAL MOOD BOOSTER" BUT NOW I GET IT. NO MORE RISKING MY BRAIN. 🙏
Ellen Sales
November 28, 2025 AT 10:05So… you’re telling me… that the thing I’ve been ignoring… is literally the thing that could kill me? And I thought I was being efficient by not reading it? I’m a disaster. I’m a walking clinical trial. Someone please take my meds away.
Josh Zubkoff
November 29, 2025 AT 09:48Look, I get it, the FDA wants to save lives, but let’s be real-this whole system is designed to make you paranoid. "Avoid"? What does that even mean? Is it 10% risk? 50%? 90%? They don’t tell you. And don’t even get me started on the "minor" label. My grandma took aspirin with warfarin for 15 years and she’s still alive. So who’s the real danger here? The drugs or the fear-mongering?
fiona collins
December 1, 2025 AT 07:48Always check with your pharmacist. They’re trained for this. Don’t guess. Don’t Google. Ask.
giselle kate
December 1, 2025 AT 19:57Why are we trusting a government agency that can’t even mail out stimulus checks on time to give us safe drug labels? This is just another way to control us. Natural remedies have been used for centuries. Why do we listen to Big Pharma’s corporate pamphlets? I’m sticking with my turmeric and lemon water.
Emily Craig
December 1, 2025 AT 20:24OMG I just realized I’ve been taking my blood pressure med with grapefruit juice for 2 years 😂😂😂 guess I’m just lucky? Or maybe I’m secretly a superhero? 🍊💥
Leisha Haynes
December 2, 2025 AT 21:13Same. I used to think the insert was just there so the company could say "we warned you." But now I take a pic of every one. I’ve got a folder called "Don’t Die Today." It’s weirdly comforting.
Amy Hutchinson
December 3, 2025 AT 02:45hey so i read this and now i’m scared to take anything. like… what if my coffee messes with my thyroid med? what if my tea? what if my cat licks my pill and then i pet him? is he now a drug delivery system? 😭
Erika Hunt
December 3, 2025 AT 16:30I’ve been keeping a digital list in Notion since my last hospital stay. I log every pill, supplement, and even the occasional melatonin gummy. I also scan the inserts and tag them by risk level. It’s taken me months to build, but now when I see a new doctor, I just hand them my tablet. No more "what are you taking?" confusion. And honestly? It’s made me feel more in control than I have in years. It’s not just about avoiding danger-it’s about reclaiming agency over your own body.
Lisa Odence
December 5, 2025 AT 01:17Thank you for this comprehensive, meticulously researched exposition on pharmacological interaction protocols. 🙌 The FDA’s 2024 terminology standardization initiative represents a landmark advancement in patient safety literacy, particularly in light of the documented 28% reduction in hospitalizations attributable to improved risk stratification lexicons. 📊 I have personally implemented the 4-step process outlined herein, and I now maintain a color-coded, cloud-synced, QR-enabled medication guide archive, with automated alerts for concurrent CYP3A4 inhibitors. 🌿💊 #MedicationSafety #Pharmacovigilance #NoMoreGuesswork
prasad gaude
December 5, 2025 AT 08:42lol i just saw ur comment about not trusting the fda… bro i live in india, we don’t even get the inserts half the time. my mom’s blood pressure med came with a hand-written note in hindi. i had to call the pharmacy to ask if "avoid grapefruit" meant "don’t eat the fruit" or "don’t hug the tree."